Health
Vol.5 No.7A4(2013), Article ID:34862,13 pages DOI:10.4236/health.2013.57A4011
Low utilization of skilled birth attendants in Ngorongoro Conservation Area, Tanzania: A complex reality requiring action
![]()
1Athena Institute for Research on Innovation and Communication in Health and Life Sciences, Faculty of Earth and Life Sciences, VU University, Amsterdam, The Netherlands; *Corresponding Author: y.roggeveen@vu.nl
2VU University Medical Centre, Amsterdam, The Netherlands
3Global Health & International Partnerships, Faculty of Medicine, University of Calgary, Calgary, Canada
4Department of Anatomy, Catholic University of Health & Allied Sciences, Mwanza, Tanzania
Copyright © 2013 Yadira Roggeveen et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 21 April 2013; revised 1 June 2013; accepted 1 July 2013
Keywords: Collaboration; Maternal Health; Quality of Care; Maasai; Complexity
ABSTRACT
Limited integration of contextual factors in maternal care contributes to slow progress towards achieving MDG5 in sub-Sahara Africa. In Ngorongoro, rural Tanzania, the maternal mortality ratio is high with 642 maternal deaths/100,000 live births. Skilled birth attendants (SBAs) assist only 7% of deliveries. This study, undertaken from 2009 to 2011, used Participatory Action Research involving local stakeholders (Maasai women and men, traditional birth attendants (TBAs), hospital staff) to examine reasons for low utilization of SBAs and moreover to develop proposals how to integrate contextual factors and local needs in the health care system. Interviews, observations and literature study were also conducted. Thaddeus and Maine’s Three Delays model is used to structure the analysis. Delaying factors in decision making at home: negative perceptions by the community on availability and quality of care in the hospital; discontinuity of care by TBAs; food and financial insecurity; desired nearness to cattle and family; limited recognition of maternal deaths; limited male health education and suboptimal birth preparedness. Delaying factors in reaching the hospital: vehicle and road limitations. Delaying factors in receiving hospital care: limited (human) resources and limited knowledge sharing at the hospital. Community members and health workers proposed: increasing food/financial security; tailoring male health education; combining TBA/SBA care to provide continuous, culturally appropriate labour support; creating separate maternity wards; increasing the number and training of staff; ensuring continuous availability of Emergency Obstetric Care. Applying solutions to increase hospital utilization seems complex as collaborative actions by multiple actors and institutions are needed to create both a needs based and clinically sound continuum of maternal care. To follow-up this process of integrating local solutions into the maternal care system, we suggest to adapt the WHO Strategic Approach—a top-down framework for the implementation of innovations—to fit this bottom-up approach.
1. INTRODUCTION
Sub-Sahara Africa faces the challenge of insufficient progress towards Millennium Development Goal (MDG) 5, concerning maternal and reproductive health. Increasing utilization of skilled birth attendants (SBAs) and access to Comprehensive Emergency Obstetric Care (CEmOC)1 are global, evidence based strategies to reduce maternal mortality and improve maternal health [1]. However, translation of global strategies into local implementation is difficult. Even when national maternal health policies are in place, locally, utilization of SBAs may remain low and maternal mortality high [2,3].
Research suggests that this policy-practice gap is caused by limited adaptation of maternal health care to local contexts [4]. When linkages between maternal health, local culture, gender, socio-economic and political factors are better acknowledged [3-7] and community experiences and needs are addressed, the acceptability, appropriateness, use and sustainability of services increases [8,9]. However, achieving both locally appropriate care during childbirth while simultaneously safeguarding clinical best practices is not straightforward and insufficiently researched [3,4,10]. This study aims to research and assist the development of such care in a local setting: Ngorongoro, rural Tanzania.
2. METHODS
2.1. Setting
In 2008, Tanzania had a maternal mortality ratio (MMR) of 790 maternal deaths per 100,000 live births (range 470 - 1300) [1]. While in 2008 antenatal care (ANC) attendance in Tanzania had increased to 76% of pregnant women attending at least once, utilization of SBAs lagged behind at 43% of deliveries [1]. In Ngorongoro, where the population consists of 97% pastoralists, mainly Maasai [11], even 90% of pregnant women received ANC at least once, but only 7% of deliveries were assisted by SBAs. Most childbirths (93%) took place at home, alone or with presence of traditional birth attendants (TBAs) [12].
The Ngorongoro Maasai are a semi-nomadic pastoralist population that have settled in the Ngorongoro Conservation Area (NCA) due to eviction from grazing lands in the adjacent Serengeti plains [13]. At the time of settlement in the NCA, Maasai were promised resources such as access to healthcare, water and education. Although UNESCO’s declaration of the NCA as a World Heritage Site in 1979 increased tourism and job opportunities, Maasai living in the area experienced loss of land rights and loss of access to other resources. Implementation of services fell short of commitments which led to distrust of government services, including healthcare [11,14,15].
In 2008, a 72-bed hospital served the 77,580 population of Ngorongoro Conservation Area (NCA), an area of 8292 km2 [11,16]. Annually, some 3351 births are expected in the hospital’s catchment area (calculation based on population and a crude birth rate of 43.2) [17]. Although not all these women might need hospital care, at least an estimated 500 women would need CEmOC from the hospital [18]. Although the hospital maternal care included CEmOC and also Prevention of Mother-to-child HIV Transmission (PMTCT), only 47 hospital deliveries occurred in 2008, illustrating severe underutilization of the hospital-based SBAs.
Low utilization of hospital maternal care takes place in a context where delivering at home is potentially fatal [12]. Maternal deaths are a major cause of death among pastoralist women [19] and the MMR in Ngorongoro District has been estimated at 642/100,000 live births (CI 329/955) [20].
In 2008, 62 hospital cases (10% of 603 female admissions) provided an illustration of local maternal morbidity: prolonged labour (5), post partum haemorrhage/sepsis after home deliveries (20), complicated miscarriages (11) and indirect maternal morbidity (26), mostly malaria. In addition to maternal risks, homebirths have been suggested to increase risk of HIV infection for all involved and hinder full provision of PMTCT [21].
Low utilization of SBAs in Ngorongoro is linked to negative attitudes of health care providers and limited time and human resources to educate women on birth preparedness during ANC [12,22]. However, the local hospital was not included in previous studies.
2.2. Aims
We undertook an in-depth exploration of reasons for almost non-use of SBAs in Ngorongoro. We aimed to first understand why and secondly—from this understanding and in collaboration with local stakeholders—to develop proposals for increasing utilization of SBAs.
2.3. Approach
To study problems in low resource settings, combining knowledge of communities, practitioners and researchers, has been advised. However, experiential knowledge of local actors, such as health workers and communities is underestimated and poorly utilized in maternal health research [4,23,24]. This study used a combination of methods, with an emphasis on Participatory Action Research (PAR), which engaged local stakeholders as experts, incorporating them as co-researchers. Co-generative inquiry, which generates knowledge on problems and solutions through communication between researchers and local experts [25], took place in order to identify actions linked to increased use of SBAs.
When using PAR, additional data collection strategies are commonly used to enrich and clarify information. These included: naturalistic and participant observation, semi-structured, in-depth interviews and reflexive journaling. Literature (research articles, books and reports on Maasai culture and health) assisted study of the historical and cultural context.
During the 2009-2011 period, 23 research meetings were conducted with 3 - 28 persons, lasting in duration from 30 minutes to 4 hours. Participants (Table 1) were included on the basis of convenience, purposeful and snowball sampling [25]. Participants were Maasai women and men of reproductive age, SBAs (medical/clinical officers, nurse-midwives) from the hospital and TBAs, community health workers, nurse attendants and hospital officers. Contact with all participants was initiated during informal conversations explaining the research at the hospital and in the community, as well as during formal meetings with local authorities. TBAs from the hospital catchment area were actively invited to participate. The study started with sessions that separately discussed topics with small numbers of participants from one group. Due to snowball sampling, the groups per session enlarged. The separation of categories of participants in the beginning ensured that perspectives of different categories of participants were discussed while limiting the possible inhibiting factor of presence of other stakeholders. However YR was always present, in agreement with community members, due to her respected work as medical doctor in the local hospital. In later stage, when discussing local care adaptations, community members and more hospital workers were mixed in the same session. This mix enhanced detailed discussion of different viewpoints, which created additional insights in problems and solutions. To enrich the mainly female community perspectives with male viewpoints, we included a session with 13 male community leaders, respecting their community role and knowledge. Research meetings varied in terms of composition of participants and took place in either the hospital or surrounding villages, following the advice from participants.
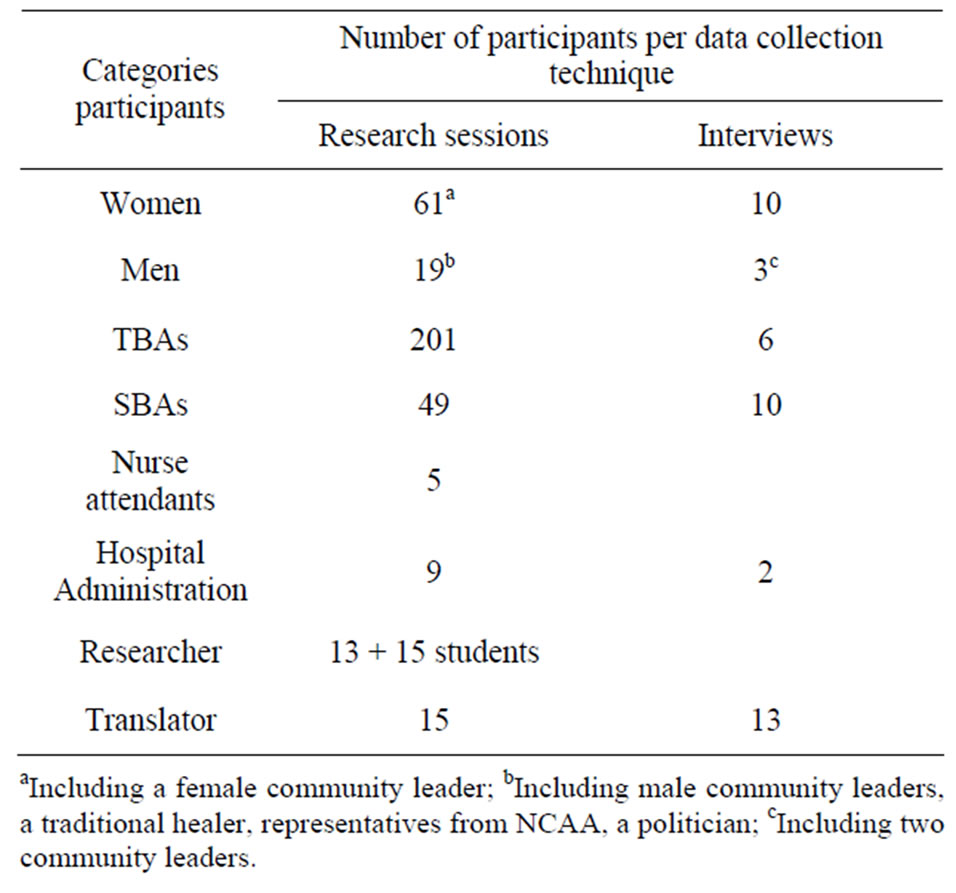
Table 1. Participant distribution.
YR worked as a medical doctor at the local hospital during the 2008-2010 period. Her inclusion in the research team, combining the dual roles of practitioner and researcher, is intrinsic to PAR. This contributed to continuous contact and the development of trust-based relationships with participants, and facilitated reflection on observations.
The majority of the participants spoke Kiswahili, which was the language spoken during health care. Translation to Maa, the language of the Maasai, was undertaken when necessary by a male research assistant, also working as a local community health worker and fluent in English, Maa and Kiswahili. Concerns from the research team that his male and health worker status might bias answers, were opposed by community members, who preferred his facilitation to any other person. Starting points for discussion were questions raised by YR and LKB regarding childbirth and knowledge of HIV/PMTCT, as PMTCT was originally planned as large part of the research. Questionnaires and topic guides on childbirth and knowledge of HIV/PMTCT were available in both Kiswahili and English, the languages of technical instruction in Tanzania.
Discussions were facilitated in a manner that accommodated concerns of the participants (community members, SBAs—including YR), such as requests to discuss HIV within the broader context of maternal health. During these discussions, participants linked low utilization of maternal health services to the absence of locally adapted maternal care. These conversations were included in data analysis. Maternal health topics identified using the questionnaires mentioned above were expanded in discussion with participants. To generate additional insights from hospital maternal care users and providers, in-depth interviews were undertaken with 31 hospital staff and community members (Table 1).
Meeting minutes with verbatim quotes were recorded in field note books or audio recorded with participants’ consent. Respondent validation after transcription and the collaborative discussion of gained knowledge in the following meetings increased accuracy and validity of the data [26]. Transcripts of field notes and recordings were analyzed manually and with ATLAS.ti research software. An iterative process of data analysis identified emerging themes. Informal remarks by community members and hospital staff, assisted analysis and reflection [27]. Because of its assistance in reflections on contextual consideration’s influence on utilization of care [4], we used the Three Delays model [28] to structure our analysis.
This model recognizes that delay in receiving treatment consists of three phases: phase 1) delay in taking the decision to seek care, phase 2) delay in reaching a health facility and phase 3) delay in receiving adequate treatment in the health facility.
The Tanzanian Commission for Science and Technology (COSTECH) and the National Institute for Medical Research (NIMR) (NIMR/HQ/R.8a/VolX./876), University of Calgary and VU Medical Centre provided ethical approval for the research. Local approval from the hospital, village leader, village and ward council and Ngorongoro Conservation Area Authority (NCAA) was obtained. Informed verbal consent was obtained from research participants.
3. RESULTS
3.1. Phase 1 Delay: Deciding to Seek Care
Proposed solutions plus identification of actors who could implement solutions are summarized in Box 1.
3.1.1. Food Security
Maasai originally relied on cattle as their main food source for milk, fat, blood and meat [11,29], but the NCA offers limited areas for extensive grazing of cattle, making their livestock less productive. To supplement nutritional needs, small scale farming was temporarily allowed in the NCA [13,30,31] but during our study, the ban on farming was renewed in 2009 due to ecological pressure [32].
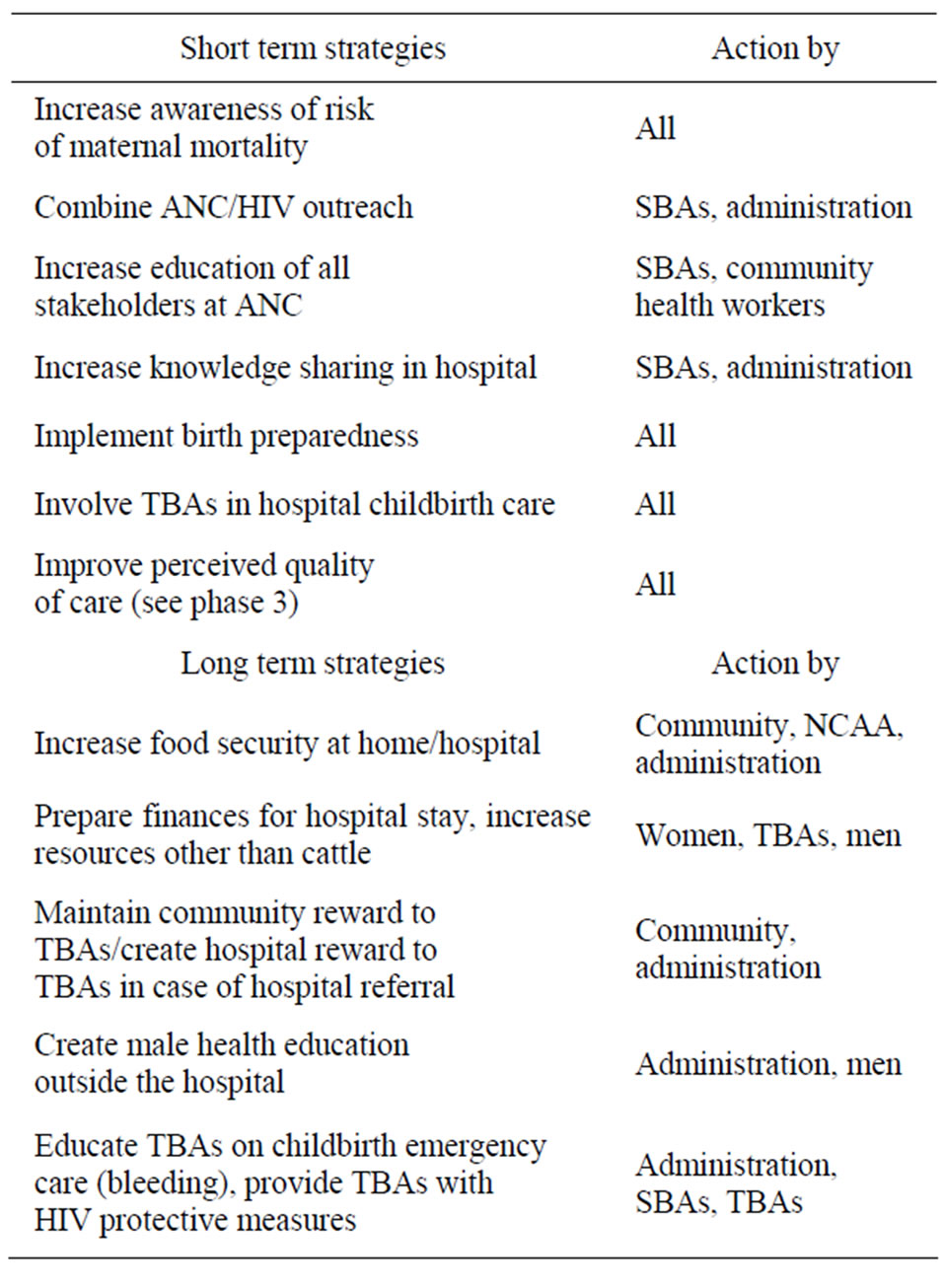
Box 1. Solutions to delay in deciding to seek care.
Resulting food insecurity affected our participants significantly. According to one TBA:
“There are many problems; even those days we have no fields to grow our food. This brings kwashiorkor to our children. So we are having a very difficult time.”
Maasai participants considered that hospital childbirth increased food insecurity because of the distance from cattle. Furthermore, food from canteens and markets close to the hospital is expensive because it is imported from outside NCA. The hospital offers one daily meal plus kitchen facilities, facilitating low food costs during admission. In addition to the concerns about food security, Maasai women and TBAs stated they disliked pregnant women having to mix with other patients in kitchens and wards, risking contagious diseases such as tuberculosis. They requested unlimited access to separate kitchens to allow care for women in labour at night.
3.1.2. Opportunity Costs
Hospital birth increased costs for women by diminishing their capacity to gather firewood, collect water and nurture children at home. As one woman delivering in hospital stated: “So the children were just taken care of by children.” Some men regarded the Maasai’s polygamous structure to be protective of pregnant women, as most of the women had co-wives or female family to assist them. According to a male community member: “If they have co-wives they would get people in the same village. That is usually not a big problem.”
3.1.3. Meaning of Childbirth, Connection to Traditions
Wives, children and cattle are signs of wealth in Maasai culture. Childbirth is crucial to women, proving their ability to give life and prosperity to husband and family [33]. Biomedical health services have been available since 1976 [34], but assistance at childbirth has traditionally been provided by TBAs. The TBAs are regarded as having a spiritual relationship with Eng’ai (the Maasai god) while they share the ability to give life [35]. At the same time, they meet women’s expectations of care before, during and after labour [12].
TBAs participating in the study showed their shelldecorated-bracelets and explained the spiritual linkage as those are worn to avert blame for difficulties during childbirth (i.e. breech delivery, placental problems, maternal/neonatal deaths). Participants stated that TBAs’ efforts are recognized by families in the form of sharing quality sheep meat with them. On the first day postpartum, men announce the child’s sex by performing cattle rituals. These actions of cultural significance could not be performed in hospital. Both participating women and TBAs themselves argued that hospital births lacked the continuous care, rituals and massage, which were provided by TBAs. To increase utilization of the hospital, TBAs and SBAs suggested to combine TBA and SBA care in the hospital.
3.1.4. Perceived Risks of Childbirth
Seeking help from SBAs is based on awareness of the risks of childbirth and recognition that SBAs are able to assist [28]. Maasai traditionally view childbirth as Eng’ai’s practice, with limited human influence. Trust in Eng’ai as a life giving entity and prayers are central [35].
Although all participants experienced maternal deaths in their communities, most thought that these were exceptions. The practice of not talking about the deceased seemed to reduce awareness of the magnitude of maternal deaths and the urgency to act. As one male community leader noted:
“When somebody dies while she is pregnant or after delivery it is sad, it is very bad … After seven days, they slaughter a sheep and then from there everybody tries to forget what happened.”
Although maternal death was not generally perceived as a significant risk, Maasai women and TBAs recognized the risk of obstructed labour. In their eyes, obstructed labour could be prevented by dietary restrictions to limit foetal growth. Women related giving birth to large babies to lack of self-discipline in adherence to these dietary restrictions. Vaginal delivery was considered to be the norm to the extent that some husbands perceived that the woman had failed if she needed instrumental intervention. Hospital fees for instrumental deliveries served to reinforce this trend of ’blaming the victim’ exhibited by some Maasai women and TBAs.
The TBAs considered that referral to hospital was necessary in cases of abnormal foetal position, high estimated birth weight, intrapartum bleeding and placenta previa. Bleeding was considered to be a major cause of maternal deaths at home where limited measures could be taken. As one TBA noted: “We can only give cows blood to drink and it is Eng’ai that stops bleeding”. Immediate breastfeeding was not employed to reduce bleeding nor was abdominal massage, despite its use during labour, because, as one TBA said: “We are afraid to touch”.
The TBAs also recognized that the home is an unsafe environment to prevent HIV infection. Instead of considering this to be a reason for hospital referral, TBAs requested protective measures at home:
“Women say: we are at big risk of transmission, also at home. When we are helping women to deliver, we have nothing, no apron, no gloves. We would really like these things, to be safe at home.”
It is noteworthy that most women who delivered in hospital had previously experienced obstetric complications at home and demonstrated increased awareness of risks. As one woman noted: “I am afraid that I may die … so that is a risk.” In comparison with community perceptions, hospital staff regarded hospital as the safest environment to deliver.
3.1.5. Education
In our study, SBAs also considered limited training and knowledge sharing by hospital staff as a factor in low SBA utilization. As one SBA argued:
“We need to counsel women more and to do this properly, more training is needed. Some staff is trained, but those without secondary school diplomas are not sent for training. When the ones who go for training come back, they do not always give feed back to the nurse attendants, so for them it is difficult to learn.”
Staff attitudes to TBAs at ANC could be more welcoming and more focused on education. As one TBA remarked:
“When I came, I was not welcome. I never heard I should come to hospital. The women come to me. I do not come to the clinics.”
Men and women requested male education on SBA utilization. SBAs agreed:
“More health education at antenatal clinics is needed for TBAs and community leaders, because women need permission from their husband to deliver in hospital. But change is very slow, because there have been many seminars already and I didn’t see more women coming.”
Men considered that ANC was not the right place for male health education because ANC was regarded a women’s territory. Male ANC outreach visits were associated with being sick (seeking medical care, collecting tuberculostatics/antiretrovirals). For this reason, men suggested that male education should take place during gatherings at council offices or in the community.
To increase maternal care and education in general, SBAs proposed combining ANC with HIV outreach:
“People live far away; many mothers do not reach [antenatal] clinics. And even then sometimes clinics are too short to counsel and test for HIV … We have outreach camps, where hospital staff camps for 1 - 2 weeks on one spot to do extensive counselling and testing, but pregnant women do not come to those places. There is no service for them there. It would be possible to combine care for pregnant women with VCT [Voluntary Counselling and Testing] outreach, but then we need a campbase where we can also see people privately. Now the camp is for us only, we visit people in their homes or in schools, halls. Aside a camp-base, we would also need all the things to do ANC.”
It seems that the ANC services that the hospital offers could be adapted to fit both community needs and to spend limited resources more efficiently.
3.1.6. Finances
Our study found that uncertainty about hospital costs led to delay in seeking care because male absence, bi-weekly cattle markets and unsure business outcomes combined badly with the unpredictable timing of childbirth. As one TBA noted:
“Also money for the car and fuel: it depends on cows or goats to sell. Suppose you do not have anybody who can just buy [your cattle] at that time, then what will you do?”
One woman delivering in hospital overcame the delay: “I said okay, we borrow money from people because my father was not at home on that day.” Participants suggested that a flat fee structure would be best. At the moment, the uncertainty of the size of hospital bills meant that cattle could not be sold until after discharge. Women also recognized that some women could not afford hospital stays. Income generation independent of cattle, such as women’s enterprises, was suggested.
3.1.7. Decision Making Process
Pastoralist women historically carry a double burden: public underrepresentation of pastoralists and limited female influence within the pastoralist community [36].
The decision whether or not to go to hospital was not made by participating Maasai women themselves. Husbands, and, in exceptional cases, family or friends decided. Although TBAs had an advisory role, it was not their decision.
Decision-making was complicated by the fact that many husbands are at a distance because of cattle grazing or urban employment. Although the mobile phone network was expanding, communication with absent husbands was difficult. When to communicate was unclear, as many women did not know their due date. A male community member mentioned some people used moon calendars, market dates or mobile phones to keep track of date.
Some men accused TBAs of keeping women at home and avoiding the hospital. However, TBAs stated that women often called TBAs too late in labour, leaving them with no option. TBAs were afraid to decide on hospital births without the husband’s support and, in the absence of birth plans, women stayed home, surrounded by indecisive people. Women delivering in hospital had often prepared birth plans with decision-makers or they communicated well by phone.
3.2. Phase 2 Delay: Reaching the Hospital
Proposed solutions plus identification of actors who could implement solutions are summarized in Box 2.
3.2.1. Distance to Hospital
Historically, rainfall dictated Maasai migration with cattle to pastures and temporary homesteads. As one SBA noted “Still even pregnant women go with the cattle”. Creation of artificial water holes allowed some people to reside in semi permanent bomas (settlements or compounds) all year [14,19]. In case of obstetric complications, long distances (up to 70 km) and rough terrain need to be covered to reach SBAs. Therefore, SBAs suggested that women who are due to give birth should await childbirth near health facilities.
3.2.2. Transport, Roads & Communication
Transport to hospital was by foot, motorbike, car or small aircraft, with immobile patients sometimes being carried on stretchers of hides and sticks. Market days increased availability of private vehicles for hospital transport. However, transport is a challenge due to mainly “black cotton soil” roads with hazardous driving conditions during rainy periods. Nocturnal driving restrictions (to maintain nocturnal peace for wildlife), restricted people to call a car for women in labour.
Increasing mobile phone availability and network coverage facilitated arranging ambulances. Most people knew the private telephone numbers of ambulance drivers. Some refused to keep these numbers at home because this was believed to invite obstetric complications. This resembles an evil eye, as a Maasai woman noted, “Looking at you and causing things.” TBAs regarded this as an ancient, declining belief. To facilitate arrangements, one telephone number for hospital emergencies was proposed.
Participants reported that cars were usually called in prolonged labour, requiring drivers to approach bomas closely, gaining community respect for the hospital. None of the participants knew of maternal deaths due to phase two delay. All participants suggested that more ambulances would facilitate emergency transport, but recognized hospital budget and resource limitations. Male community members suggested men should develop community car planning.
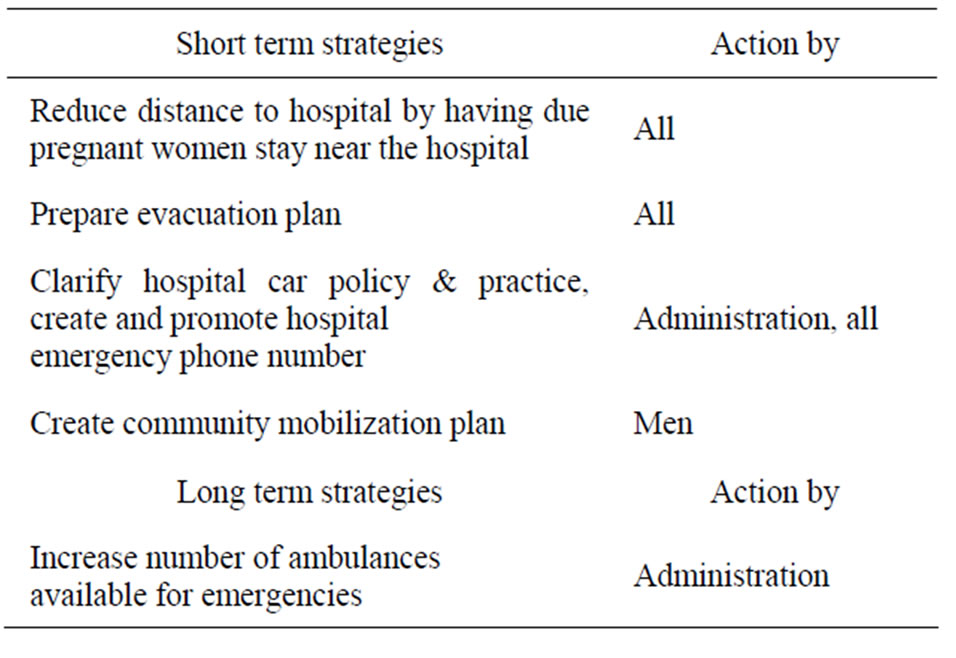
Box 2. Solutions to delay in reaching the hospital.
3.2.3. Travel Costs
Community members and hospital staff perceived hospital transport fees as unclear. Hospital policy was free transport for childbirth, but women with pregnancy complications and not in labour sometimes had to pay. HIV positive or very poor women could request fee exemption. Men requested simplification of the billing structure to increase awareness of and adherence to the hospital transport policy.
3.3. Phase 3 Delay: Receiving Adequate Treatment
Proposed solutions plus identification of actors who could implement solutions are summarized in Box 3.
3.3.1. Perception of Hospital Services, Quality of Care & Provider Reputation
Negative user perceptions of quality of care, staff attitudes, waiting times, lack of supplies and inefficiency hinder SBA utilization [28]. When community decisions
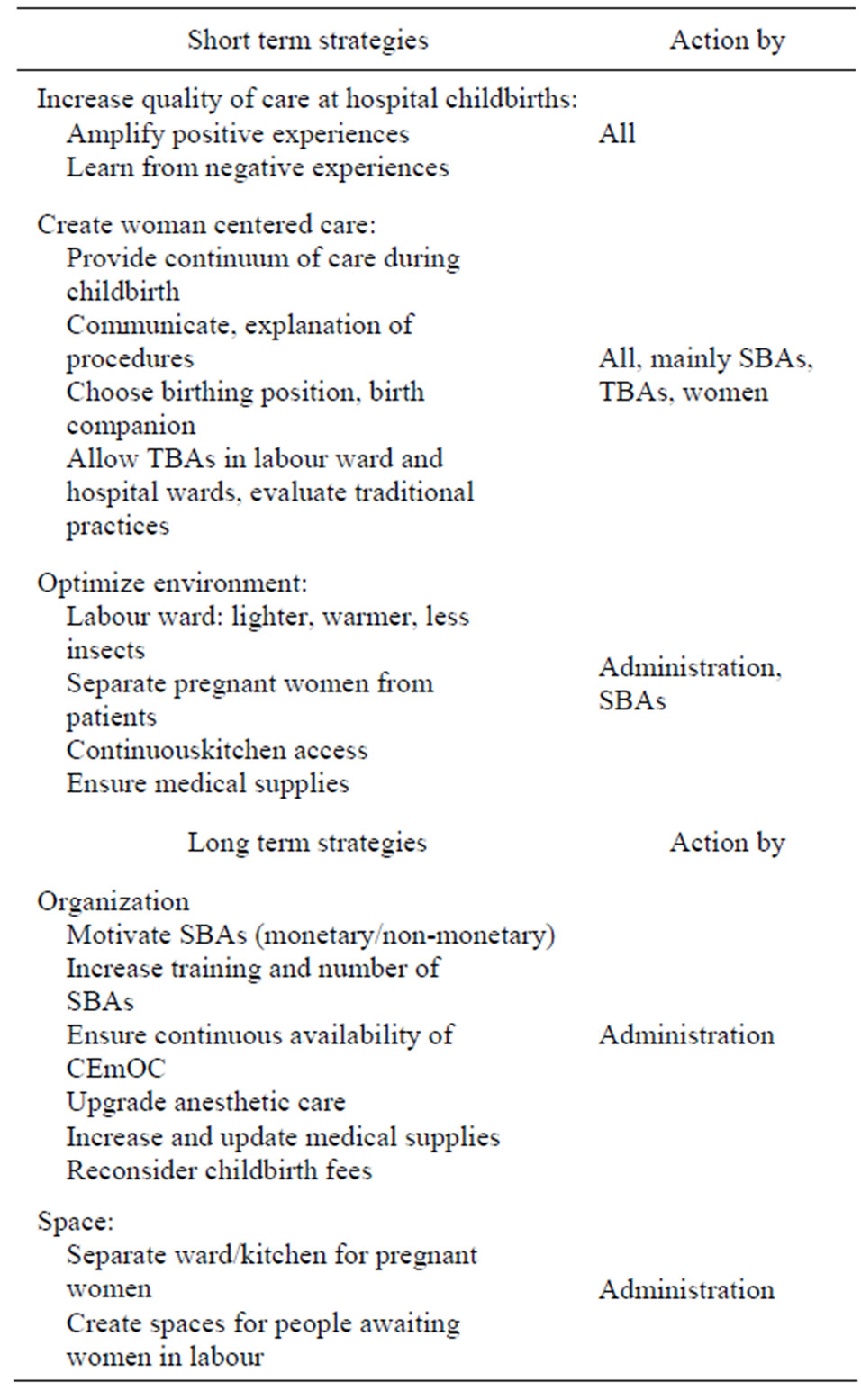
Box 3. Solutions to delay in receiving adequate treatment.
not to use SBAs can be simply reduced to cultural background—as illustrated by a one SBA participant, “It is just their culture”—critical appraisal of care and health services might be hindered.
Women who delivered in hospital had positive hospital experiences, reporting that SBAs handled complications well. Some mentioned negative stories about SBAs circulated in the community, not in line with their own positive experiences, as a woman shared:
“I was scared of the history of the nurses, that okay, they can just help you, they are helpful, but not much. But when I came here I saw that they are really very sharp, smart, not like the people were telling.”
Women who preferred home births, perceived hospital services negatively, based on stories and past experiences. Women disapproved of non-pregnant patients to be admitted in maternity ward (due to hospital overcrowding). Although labour wards were private, the wards were perceived as cold when compared to bomas. Women also said that they felt alone when TBAs were excluded from the labour ward. As one woman said: “There is a new environment for us, there are new people there we don’t know, and then someone else is taking care of you.” SBAs requested TBAs to stay outside the labour ward. According to one TBA: “TBAs aren’t allowed in labour ward. This is hurting us, as we want to be with the mother. We feel not respected.” Women and TBAs desired to be close to each other, even if this meant TBAs would sit in the same hospital bed while awaiting delivery.
Other issues concerned differing approaches to labour and delivery. For example, women preferred the ‘all fours’ position taken at home births over the supine position of hospital births. As one TBA noted: “We Maasai don’t like to lie down.” Vaginal examination was also disliked: “We don’t like to be touched in our vagina.” The massage, rituals and hot drinks associated with home delivery were missed in the hospital. A TBA participant compared the different locations: “We are not allowed to use oil for massage in the hospital. At home, fat is melted and used to massage the abdomen of women who are giving birth.” Women and TBAs preferred perineal tears to episiotomy. Misconceptions about the word ‘cut’ in the Maa language (used interchangeably for both episiotomies and caesarean sections), led people to fearfully believe that childbirth in the hospital often implied surgery.
SBAs explained past collaboration with TBAs had been difficult, often due to late TBA referral to hospital, causing delay in care for complications. SBAs felt that they had been blamed by community members for childbirth complications, which occurred in hospital, but may have been prevented if women had arrived earlier. SBAs said they kept TBAs outside the labour ward because of past TBA interference with vaginal examination and episiotomy. Additionally, most SBAs perceived rituals and massage as not contributing to care, although some SBAs mentioned they did not know enough about TBA care to judge. SBAs also disliked working conditions in the labour ward (dark, cold, easily accessible to mosquitoes). Some SBAs regretted not being able to provide continuous support during labour due to high workload and staff shortages. A SBA summarized:
“People don’t like hospital. They say the mother is left alone in the labour ward. They want a nurse to be there all the time, but this isn’t possible, there aren’t enough. At the boma, TBAs do abdominal massage; we do not allow that in hospital. People dislike birthing position in the hospital, they would like to squat [note YR: opposed by women and TBAs, who preferred “all fours” position]. They are afraid of episiotomy and pv [vaginal] examination, they say: my child will come out by itself. In the boma, there is a big fire, which makes it very hot; in labour ward it is very cold. During delivery women don’t eat, [in the boma] they have porridge. After delivery, they have soup of blood with local herbs.”
Both TBAs and SBAs stated that confidence in SBAs facilitated the choice for hospital childbirth. Incentives and inspiring leadership were mentioned as motivating SBAs. Despite negative past experiences, SBAs and TBAs proposed to increase collaboration. As one asserted: “If we can work together, we can make it better!”
3.3.2. Communication
Positive experiences for TBAs and women included conversations with SBAs awaiting childbirth and guidance during labour. SBAs recognized the importance of having good relationships to optimize labour outcome. However, language barriers between SBAs, women and TBAs contributed to miscommunication because SBAs felt they could not provide optimal care if women did not speak Kiswahili. Additionally, some TBA did not understand differences between nurses, technicians and nurse assistants, which led to wrong expectations (e.g. a TBA expected a nurse assistant to perform delivery, while the nurse assistant was present to watch over a woman while the SBA attended another patient. When the nurse assistant walked out of labour ward to call the SBA, the TBA felt helpless, being outside labour ward, while the woman was alone inside and the TBA thought the SBA was leaving instead of being called). Such factors may cause women to stay at home according to a SBA: “So some [women] deliver at home, because they are afraid of coming to hospital because of communication.” One male community member proposed that Kiswahili speaking TBAs should assist hospital staff: “Language can be problematic, culture can be problematic. TBAs would be a big help to alleviate that kind of thing if they were working with professional staff.”
3.3.3. Resources
Medication, intravenous fluids and blood were well appreciated by community members and SBAs. SBAs suggested CEmOC equipment could be expanded and updated, but mentioned staff shortages challenged continuous availability of CEmOC:
“We only have one doctor. So once doctor isn’t here … complicated cases can appear here and no management can be taken. So that is why the clinical officer decided to refer.”
Both SBAs and community members mentioned that limited human resources could inhibit SBA utilization: “I think if there is no doctor, also patients aren’t coming, they are going to another hospital.” SBAs suggested the need to increase the number of SBAs and the availability of anaesthetist training to ensure around the clock provision of CEmOC.
3.3.4. Hospital Fee Structure
Uncomplicated hospital delivery was free, but instrumental delivery or treatment of complications was not. Many Maasai women stated that this was unfair because complications were caused by Eng’ai and were not the fault of individuals. Furthermore, women felt this fee structure and the costs it imposed on the family encouraged husbands to blame women for complications. Women proposed flat fee structures for hospital childbirth, regardless of complications, because fixed costs would facilitate discussions with husbands and inclusion of foreseeable hospital costs when they prepare for birth.
Women stated that husbands would be willing to pay for good quality care. TBAs and women suggested that the hospital should explain who (hospital, government or donors) paid the costs if childbirth was free because previous experiences with free items, such as promotion articles from commercial companies, had led to associations of free care with bad quality.
4. DISCUSSION
4.1. Low Utilization of SBAs: A Complex Reality
Low utilization of SBAs in the NCA is a complex issue, influenced by a variety of factors and actors. Delaying factors could be identified in all phases of Thaddeus and Maine’s model. Many of these factors did not only have their origins directly in health services but other interdependent domains (politics and policies, traditions, food security, family life, cattle, gender, infrastructure, conservation of flora and fauna) were also implicated. Additionally, the culture of silence surrounding maternal deaths in the Maasai community hampered a sense of urgency to address the issue.
4.2. Finding Solutions
None of the actors alone held the power to implement all suggested solutions to increase utilization of SBAs. Participants identified a need for increased collaboration and communication between various actors and institutions. This will require behavioural changes in both maternal health services and the community. Viability of solutions can be determined through implementation of the proposed solutions, creating a life experience, vivencia [37] that will further test the internal and external validity of study results [38]. Choosing a solution to start implementation is difficult considering the diversity of proposed solutions. In our study the choices where to start off were not made rigidly, but evolved from which stakeholders were most active in changing existing patterns. The “lowest fruit” to pick, was the enthusiasm of TBAs and SBAs to increase collaboration.
4.3. Collaborative Labour Care
Participants proposed to combine traditional and biomedical care to women in labour, which would involve active collaboration between TBAs and SBAs in the form of shared care. This would be an innovation [2] in local maternal care as this is no current practice.
The Maasai have been labelled as reluctant to change practices, but this does not do justice to the complexity of traditional ways of life. In reality, Maasai combine use of both traditional (male) healers and biomedical health providers [39] and adapt to circumstances when change is desired by the community itself [40,41]. Combined care by SBAs and Maasai TBAs has not previously been reported. To facilitate change, TBAs wanted hospital staff to inform community leaders of the need for TBAs to accompany women to hospital. One woman who delivered in hospital illustrated change from within and the role of men in this process:
“My husband talked for a long time to them [cowives], but they just delivered at home. But because I started now here [in hospital], it will be custom now that no one can just deliver at home.”
Suggestions for SBA-TBA collaboration in literature range from case referrals by TBAs to TBAs providing psychosocial support during labour [42]. The integration of TBAs with formal health systems has been previously suggested as a way of increasing utilization [43]. Moreover, birth companions enhance both quality of care and progress of labour, and reduce the need for CEmOC [44,45]. Respect for the central role of Maasai TBAs would include allowing them to be a continuous birth companion if women desire, not only at home but also in hospital. We expect that collaboration could enhance a continuous learning environment for both TBAs and SBAs. To identify which roles Maasai TBAs could fulfil in collaboration with SBAs, precise childbirth practices by TBAs are subject of further study.
4.4. Institutional Responsiveness & Resources
The promotion of SBAs should occur simultaneously with the improvement of the quality of health care services, health systems and (human) resources in order to ensure continuity of care and access to CEmOC [28,43, 45]. In the NCA, as in other low resource settings in Tanzania and elsewhere, these are challenging issues [46-48]. Clinical audits, but also funding of locally identified solutions and flexible financing from donors would be supportive [8,49-52]. Community preference for flat rate maternal care fees should be seriously considered. Participants also suggested that the maternity ward and kitchen should be a separate unit, resembling Maternity Waiting Homes. Although it is unknown if such facilities reduce maternal mortality or morbidity [53], respecting the call for a separate hospital structure for pregnant women may increase perceived quality of services.
4.5. Persistent Problem
The complex linkages and long history of low utilization of SBAs in the NCA begs the question of whether low utilization is a “persistent” problem. Application of this terminology from policy science and information technology has been suggested to analyze longstanding health problems [54]. Persistent problems are systemic in nature, while deeply rooted within our actions, institutions and societies. By repeating our common actions, problems are enforced rather than solved. Recognizing persistent problems can be the start of solving them. However, conservative approaches from one sector’s perspective, such as simply promoting SBAs as “best practice”, do not suffice. Other approaches are needed, such as embracing different perspectives to care to successfully create context specific maternal care practices. This multifaceted approach is suggested to eventually make health systems “accessible, affordable, of high quality and trustworthy” [54]. This is a fragile process, as it relies on the willingness of actors and institutions, users and providers to communicate, collaborate and share power [23]. However, collaborative approaches to increase utilization of SBAs have proved successful and cost-effective in Tanzania and Kenya [10,55]. Implementation of solutions could further clarify if low utilization of SBAs in NCA is a persistent problem.
4.6. Follow-Up
Rapidly changing low resource settings require flexible adaptation to local circumstances [23]. This research was of direct interest to those participating because we included local researchers, practitioners and community experts and focused on maternal health topics which were identified as important. We are of opinion that:
“Lessons learnt from project interventions that are based on local knowledge and practices, take a highly participatory approach and allow interventions to be managed flexibly should be taken forward in project design and policy development” [11].
To follow up the implementation of suggested solutions, we propose an adaptation of the WHO Strategic Approach, a top down approach to incorporate innovations into policies and programmes [56]. This approach stimulates policymakers to start a multidisciplinary exploration of Sexual and Reproductive Health challenges, identify local needs and stimulates that local successful health innovations can be used to scale up quality, use of and access to services. We argue, that the Strategic Approach could be applied to maternal health in a bottom up process (Figure 1), in which local stakeholders themselves initiate this process, recognizing that context specific problem solving by local stakeholders (in our case women, men, management, healthcare workers and community leaders) can also start the adaptation of maternal policies and practices in health systems [57]. Local stakeholders can then connect with policy makers from bottom up. The bottom up implementation of local innovations into health systems is under-researched.
The WHO Strategic Approach has three stages. The process our participants engaged in shows similar stages: Stage I: they identified challenges, needs and proposed solutions. In the context of our study of utilization of SBAs, Stage II would involve the further development, testing and study of proposed innovations. This is the focus of ongoing research in our case study. Stage III would involve scaling up of successful innovations. Connecting with policy makers and common health services mainly takes place in Stage II and III.
Limitations of our study require discussion. First, sample size was limited and selection of participants was narrowed to those available. Second, participatory approaches such as PAR are biased by inclusion of active and articulate participants, resulting in underrepresentation of those who are not. In order to mitigate this bias, we included participants that did and did not use hospital for childbirth, and during the research created a respectful and patient atmosphere. Third, TBAs outnumbered SBAs in our sample and women who were not TBA were underrepresented. In addition, PAR is evidently context specific and results cannot be automatically generalized, nor is it intended to produce results that can be generalized. Research involvement of policy makers and NCAA representatives was limited, which may hamper implementation and up-scaling of results. A more extended approach with focus groups of policy makers and NCAA representatives could create additional insights. Quantitative data gathering strategies and analysis could assist to show the dominate factors of low utilization of skilled birth attendants and could help to create further insight in behavior patters. Magoma et al. [12] have started research on Birth Preparedness and Complication Readiness and the use of SBAs in the area. We propose that prospective follow up study of a big cohort of pregnant women which studies utilization of SBAs and inhibiting and facilitating factors/implementations could further quantify dominate factors and problem-solving. Quantitative data on current maternal mortality ratio in the area is also needed. Awareness of limitations has informed our follow-up study of this local setting.
5. CONCLUSION
Low utilization of SBAs in NCA is a complex issue which requires context specific problem solving. The implementation of solutions requires communication and collaboration by all actors and institutions, while creating continuity of care during childbirth and a needs-based,

Figure 1. WHO Strategic Approach [56] from “bottom up”.
comprehensive maternal care pathway that is both culturally appropriate and clinically optimal.
6. ACKNOWLEDGEMENTS
We thank participants, administrative bodies, community leaders and hospital staff in Ngorongoro Conservation Area for their support of this study. Our thanks to Saning’o Godwin Ole Mshumba for facilitation and translation. YR acknowledges financial support from the Tweega Medica Foundation and the Netherlands Society for Tropical Medicine and International Health. Finally, we thank Prof. Wilfreda Thurston, Fiona Budge, Ellen Nelissen and Andrea Solnes Miltenburg for their review of this manuscript.
REFERENCES
- WHO, World Bank, UNICEF and UNFPA (2010) Trends in maternal mortality: 1990 to 2008. WHO, Geneva. http://whqlibdoc.who.int/publications/2010/9789241500265_eng.pdf
- Fajans, P., Simmons, R. and Ghiron, L. (2006) Helping public sector health systems innovate: The strategic approach to strengthening reproductive health policies and programs. American Journal of Public Health, 96, 435- 440. doi:10.2105/AJPH.2004.059907
- Freedman, L.P., Graham, W.J., Brazier, E., Smith, J.M., Ensor, T., Fauveau, V., et al. (2007) Practical lessons from global safe motherhood initiatives: Time for a new focus on implementation. The Lancet, 370, 1383-1391. doi:10.1016/S0140-6736(07)61581-5
- Gil-González, D., Carrasco-Portiño, M. and Ruiz, M.T. (2006) Knowledge gaps in scientific literature on maternal mortality: A systematic review. Bulletin of the World Health Organization, 84, 903-909. http://www.who.int/bulletin/volumes/84/11/05-029454.pdf
- Filippi, V., Ronsmans, C., Campbell, O.M.R., Graham, W.J., Mills, A., Borghi, J., et al. (2006) Maternal health in poor countries: The broader context and a call for action. The Lancet, 368, 1535-1541. doi:10.1016/S0140-6736(06)69384-7
- Graham, W.J. and Hussein, J. (2007) Minding the gaps: A reassessment of the challenges to safe motherhood. American Journal of Public Health, 97, 978-983. doi:10.2105/AJPH.2005.073692
- Hussein, J., Mavalankar, D.V., Sharma, S. and D’Ambruoso, L. (2011) A review of health system infection control measures in developing countries: What can be learned to reduce maternal mortality. Globalization and Health, 7, 14. doi:10.1186/1744-8603-7-14
- Cochran, P.A.L., Marshall, C.A., Garcia-Downing, C., Kendall, E., Cook, D., McCubbin, L., et al. (2008) Indigenous ways of knowing: Implications for participatory research and community. American Journal of Public Health, 98, 22-27. doi:10.2105/AJPH.2006.093641
- Neumann, A.K. and Lauro, P. (1982) Ethnomedicine and biomedicine linking. Social Science & Medicine, 16, 1817-1824. doi:10.1016/0277-9536(82)90442-7
- UAFD and FCI (2007) Testing approaches for increasing skilled care during childbirth: Key findings from Igunga District, Tanzania. Ubora wa Afya kwa Familia Duniani (UAFD) & Family Care International (FCI), Dar es Salaam. http://familycareintl.org/UserFiles/File/SCI%20Tanzania%20Report%20March%202008.pdf
- Kipuri, N. and Sørensen, C. (2008) Poverty, pastoralism and policy in Ngorongoro. In Tauli-Corpus, V., EnkiweAbayao, L. and De Chavez, R., Eds., Indigenous People’s Self-Determined Development—Towards an Alternative Development Paradigm, Tebtebba Foundation, Baguio City, 349-415.
- Magoma, M. and Requejo, J. (2010) High ANC coverage and low skilled attendance in a rural Tanzanian district: A case for implementing a birth plan intervention. BMC Pregnancy and Childbirth, 10, 13. doi:10.1186/1471-2393-10-13
- Lithgow, T. and Van Lawick, H. (2004) The Ngorongoro story. Camerapix Publishers International, Nairobi.
- Århem, K. (1985) Two sides of development: Maasai pastoralism and wildlife conservation in Ngorongoro, Tanzania. Ethnos, 49, 186-210. doi:10.1080/00141844.1985.9981281
- Swanson, L.A. (2007) Ngorongoro Conservation Area: Spring of life. Master Thesis, University of Pennsylvania, Philadelphia. http://repository.upenn.edu/cgi/viewcontent.cgi?article=1009&context=mes_capstones
- Ngorongoro District Council (2008) Census Ngorongoro District (local print-out).
- Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC), National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS) and Macro International Inc. (2008) Tanzania HIV/AIDS and Malaria Indicator Survey 2007-08. TACAIDS, ZAC, NBS, OCGS, and Macro International Inc., Dar esSalaam. http://www.tacaids.go.tz/dmdocuments/THMIS%202007-08.pdf
- WHO, UNFPA, UNICEF and AMDD (2009) Monitoring emergency obstetric care: A handbook. WHO, Geneva. http://www.who.int/reproductivehealth/publications/monitoring/9789241547734/en/index.html
- Kipuri, N. and Ridgewell, A. (2008) A double bind: The exclusion of pastoralist women in the east and horn of Africa. Report Minority Rights Group International, London. http://www.unhcr.org/refworld/pdfid/494672bc2.pdf
- Johnson, R.B., Magoma, M., Leslie, P.W., Bennett, T. and Gallo, M. (2005) Maternal mortality and morbidity in Ngorongoro district, Northern Tanzania. As cited in: Magoma, M., Requejo, J., Campbell, O.M.R., Cousens, S. and Filippi, V. (2010) High ANC coverage and low skilled attendance in a rural Tanzanian district: A case for implementing a birth plan intervention. BMC Pregnancy and Childbirth, 10, 13. doi:10.1186/1471-2393-10-13
- Birks, L., Powell, C., Thomas, A., Medard, E., Roggeveen, Y. and Hatfield, J. (2011) Promoting health, preserving culture: Adapting RARE in the Maasai context of Northern Tanzania. AIDS Care, 23, 585-592. doi:10.1080/09540121.2010.516344
- Magoma, M. and Requejo, J. (2011) How much time is available for antenatal care consultations? Assessment of the quality of care in rural Tanzania. BMC Pregnancy and Childbirth, 11, 64. doi:10.1186/1471-2393-11-64
- Chambers, R. (2010) Paradigms, poverty and adaptive pluralism. IDS Working Papers, 344, 1-57. doi:10.1111/j.2040-0209.2010.00344_2.x
- Bergström, S. (2005) Obstetric ectoscopy: An eye-opener for hospital-based clinicians. Acta Obstetricia et Gynecologica Scandinavica, 84, 105-107. doi:10.1111/j.0001-6349.2005.00664.x
- Hennink, M., Hutter, I. and Bailey, A. (2011) Qualitative Research Methods. Sage Publications, London, Los Angeles, New Delhi, Singapore, Washington DC.
- Mays, N. and Pope, C. (2000) Qualitative research in health care. Assessing quality in qualitative research. BMJ (Clinical Research Ed.), 320, 50-52. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1117321/pdf/50.pdf doi:10.1136/bmj.320.7226.50
- Creswell, J.W. (2007) Qualitative inquiry & research design: Choosing among five approaches. Sage, Thousand Oaks.
- Thaddeus, S. and Maine, D. (1994) Too far to walk: Maternal mortality in context. Social Science & Medicine, 38, 1091-1110. doi:10.1016/0277-9536(94)90226-7
- Århem, K. (1989) Maasai food symbolism: The cultural connotations of milk, meat, and blood in the pastoral Maasai diet. Antropos, 84, 1-23. http://www.jstor.org/stable/10.2307/40461671
- Boone, R.B., Galvin, K.A., Thornton, P.K., Swift, D.M. and Coughenour, M.B. (2006) Cultivation and conservation in Ngorongoro conservation area, Tanzania. Human Ecology, 34, 809-828. doi:10.1007/s10745-006-9031-3
- Neumann, R.P. (1995) Local challenges to global agendas: conservation, economic liberalization and the pastoralists’ rights movement in Tanzania. Antipode, 27, 363-382. doi:10.1111/j.1467-8330.1995.tb00285x
- UNESCO (2009) Decision—33COM 7B.9—Ngorongoro Conservation Area (United Republic of Tanzania) (N 39). Seville. http://whc.unesco.org/en/decisions/1801
- Talle, A. (2007) “Serious Games”: Licences and prohibitions in Maasai sexual life. Africa, 77, 351-370. doi:10.3366/afr.2007.0062
- Watschinger Family (1994) “Don’t give up hope”, Herbert Watschinger, A life in the service of the Maasai.
- Hodgson, D.L. (2005) The curch of women—Gendered encounters between Maasai and Missionaries. Indiana University Press, Bloomington, Indianapolis.
- Ngoitiko, M. (2008) The pastoral women’s council: Empowerment for Tanzania’s Maasai. International Institute for Environment and Development Gatekeeper Series, 137e, 1-20. http://pubs.iied.org/pdfs/14571IIED.pdf
- Borda, O.F. (2001) Participatory (action) research in social theory: Origins and challenges. In: Reason, P. and Bradbury, H., Eds., Handbook of Action Research: Participative Inquiry and Practice, SAGE, London, 27-37.
- Greenwood, D.J. and Levin, M. (2007) Introduction to action research: Social research for social change. Sage Publications, Thousand Oaks.
- Westerlund, D. (2006) African indigenous religions and disease causation—From spiritual beings to living humans. Brill, Leiden.
- May, A. and Ikayo, F.N.O. (2007) Wearing illkarash: Narratives of image, identity and change among maasai labour migrants in Tanzania. Development and Change, 38, 275-298. doi:10.1111/j.1467-7660.2007.00412.x
- McCabe, J.T., Leslie, P.W. and DeLuca, L. (2010) Adopting cultivation to remain pastoralists: The diversification of Maasai livelihoods in northern Tanzania. Human Ecology, 38, 321-334. doi:10.1007/s10745-010-9312-8
- van Roosmalen, J., Walraven, G., Stekelenburg, J. and Massawe, S. (2005) Editorial: Integrating continuous support of the traditional birth attendant into obstetric care by skilled midwives and doctors: A cost-effective strategy to reduce perinatal mortality and unnecessary obstetric interventions. Tropical Medicine & International Health, 10, 393-394. doi:10.1111/j.1365-3156.2005.01411.x
- Byrne, A. and Morgan, A. (2011) How the integration of traditional birth attendants with formal health systems can increase skilled birth attendance. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics, 115, 127-134. doi:10.1016/j.ijgo.2011.06.019
- Hodnett, E.D., Gates, S., Hofmeyr, G.J. and Sakala, C. (2012) Continuous support for women during childbirth. Cochrane Database of Systematic Reviews, 10, Article ID: CD003766. doi:10.1002/14651858.CD003766.pub4
- Mathai, M. (2011) To ensure maternal mortality is reduced, quality of care needs to be monitored and improved alongside increasing skilled delivery coverage rates. BJOG: An International Journal of Obstetrics & Gynaecology, 118, 12-14. doi:10.1111/j.1471-0528.2011.03104.x
- Dogba, M. and Fournier, P. (2009) Human resources and the quality of emergency obstetric care in developing countries: A systematic review of the literature. Human Resources for Health, 7, 7. doi:10.1186/1478-4491-7-7
- Manzi, F., Schellenberg, J.A., Hutton, G., Wyss, K., Mbuya, C., Shirima, K., et al. (2012) Human resources for health care delivery in Tanzania: A multifaceted problem. Human Resources for Health, 10, 1-10. doi:10.1186/1478-4491-10-3
- Tanzania Ministry of Health and Social Welfare (2008) The national road map strategic plan to accelerate reduction of maternal, newborn and child deaths in Tanzania 2008-2015. Dar es Salaam, Tanzania. http://www.unfpa.org/sowmy/resources/docs/library/R224_MOHTanzania_2008_Roadmap_MNCH.pdf
- Borghi, J., Ensor, T., Somanathan, A., Lissner, C. and Mills, A. on Behalf of the Lancet Maternal Survival Series Steering Group (2006) Mobilising financial resources for maternal health. The Lancet, 368, 1457-1465. doi:10.1016/S0140-6736(06)69383-5
- Campbell, O. and Graham, W. (2006) On behalf of the lancet maternal survival series steering group (2006) strategies for reducing maternal mortality: Getting on with what works. The Lancet, 368, 1284-1299. doi:10.1016/S0140-6736(06)69381-1
- Hofmeyr, G.J., Haws, R.A., Bergström, S., Lee, A.C.C., Okong, P., Darmstadt, G.L., et al. (2009) Obstetric care in low-resource settings: What, who, and how to overcome challenges to scale up? International Journal of Gynecology & Obstetrics, 107, S21-S45. doi:10.1016/j.ijgo.2009.07.017
- Kerber, K.J., de Graft-Johnson, J.E., Bhutta, Z.A., Okong, P., Starrs, A. and Lawn, J.E. (2007) Continuum of care for maternal, newborn, and child health: From slogan to service delivery. The Lancet, 370, 1358-1369. doi:10.1016/S0140-6736(07)61578-5
- van Lonkhuijzen, L., Stekelenburg, J. and Van Roosmalen, J. (2012) Maternity waiting facilities for improving maternal and neonatal outcome in low-resource countries. Cochrane Database of Systematic Reviews, 10, Article ID: CD006759. doi:10.1002/14651858.CD006759.pub3
- Broerse, J. and Bunders, J. (2010) Transitions in health care systems: Dealing with persistent problems. VU University Press, Amsterdam.
- Boulenger, S. and Dmytraczenko, T. (2007) Cost of family care international’s skilled care initiative in Kenya and Tanzania. Abt. Associates Inc., Bethesda. http://familycareintl.org/UserFiles/File/SCI%20Costing%20Analysis.pdf
- Fajans, P., Simmons, R. and Ghiron, L. (2006) Helping public sector health systems innovate: The strategic approach to strengthening reproductive health policies and programs. American Journal of Public Health, 96, 435- 440. doi:10.2105/AJPH.2004.059907
- Behague, D., Tawiah, C., Rosato, M., Some, T. and Morrison, J. (2009) Evidence-based policy-making: The implications of globally-applicable research for context-specific problem-solving in developing countries. Social Science & Medicine, 69, 1539-1546. doi:10.1016/j.socscimed.2009.08.006.
ABBREVIATIONS
CEmOC: Comprehensive Emergency Obstetric Care NCA: Ngorongoro Conservation Area NCAA: Ngorongoro Conservation Area Authority SBA(s): Skilled birth attendant(s)
TBA(s): Traditional birth attendant(s)
WHO: World Health Organisation
NOTES
1Comprehensive emergency obstetric care: Administer parenteral antibiotics, administer uterotonic drugs (i.e. parenteral oxytocin), administer parenteral anticonvulsants for preeclampsia and eclampsia (i.e. magnesium sulfate), manually remove the placenta, remove retained products (e.g. manual vacuum extraction, dilation and curettage), perform assisted vaginal delivery (e.g. vacuum extraction, forceps delivery), perform basic neonatal resuscitation (e.g. with bag and mask), perform surgery (e.g. caesarean section) and perform blood transfusion [18].

