Open Journal of Medical Microbiology
Vol.2 No.3(2012), Article ID:22827,6 pages DOI:10.4236/ojmm.2012.23017
Microbiological Examination of Sachet Water Due to a Cholera Outbreak in Ibadan, Nigeria
1Department of Microbiology, Federal University of Agriculture, Abeokuta, Nigeria
2Department of Microbiology, Leads City University, Ibadan, Nigeria
Email: *foluwafemi2000@yahoo.co.uk
Received June 15, 2012; revised July 15, 2012; accepted July 25, 2012
Keywords: Sachet Water; Coliforms; Vibrio sp.; Cholera; Water Borne Diseases; Human Health
ABSTRACT
A severe outbreak of cholera in Ibadan (Oyo state, Nigeria) occurred after a devastating flood in August, 2011, causing the death of over 18 persons and several cases of hospitalization. The project aimed at screening sachet water for microorganisms related to water-borne diseases. One hundred sachet water samples were randomly collected. The pH was determined using a digital pH meter. Values ranged between 6.3 - 8.7, with 28% of the samples being above the WHO approved range of 6.4 - 7.6. No residual chlorine was detected. Gram negative isolates were 80%, while 20% were Gram positive. Faecal coliforms above the recommended WHO zero coliforms per 100 mL were 30%. Escherichia coli had the highest incidence (17%), followed by Acinetobacter sp. (12%), Enterobacter aerogenes (11%), Flavobacterium sp. (11%), Proteus mirabilis (11%), Staphyloccocus aureus (10%), Bacillus subtilis (8%), Micrococcus sp. (5%), Streptococcus faecalis (2%), Klebsiella sp. (2%) and Vibrio cholerae (1%). There is urgent need for public awareness campaigns against water-borne diseases.
1. Introduction
Ibadan, the capital of Oyo state in southwestern Nigeria has a population of over 4.1 million people [1]. In the city, people from all works of life depend on water from questionable environmental sources to satisfy their drinking needs. Good drinking water is of basic importance to human physiology, and man’s continued existence depends very much on its availability. The human body is made up of 70% water. People begin to feel thirsty after a loss of only 1% of body fluid and risk death, if body fluids loss is near 10% [2]. The provision of potable water to the rural and urban population is necessary to prevent health hazards [3]. Before water can be described as potable, it has to comply with certain physical, chemical and microbiological standards, which are designed to ensure that the water is palatable and safe for drinking [4]. Potable water is defined as water that is free from disease-producing microorganisms and chemical substances deleterious to health [5].
Water can be obtained from a number of sources, among which are streams, lakes, rivers, ponds, springs and wells [6] Unfortunately, clean, pure and safe water only exists briefly in Nature and is immediately polluted by prevailing environmental factors and human activities. Water from most sources is unfit for immediate consumption without some sort of treatment [7].
In Nigeria, and Ibadan in particular, with an increasing population density the scarcity and pollution of surface water pose a serious problem for urban drinking water supplies [8-10]. A report in 2004 [10] showed that out of the total urban households in Ekiti state (Nigeria) only 53.3% have access to pipe-borne water and only 43.3% of the households in the southwestern part of the country have such access. Rapid urban growth often puts tremendous pressure on water resources.
In many parts of Nigeria and several other African countries, piped water supply is either unavailable or irregular, especially in the small-sized communities and towns. Even in most Nigerian cities, the supply of water for domestic purposes has several accompanying inadequacies. According to Sangodoyin [11] reasons given for these inadequacies include an enormous socio-economic rate of development, a growing industrial base, poor planning, insufficient funding, haphazard implementation of programs, and a lack of maintenance culture as well as technically deficient personnel.
The consequences of water-borne bacteria and viral infections such as polio, hepatitis, cholera, typhoid, diarrhea, stomach cramps, etc., have been well established. In 2006, water-borne diseases were estimated to cause 1.8 million deaths worldwide each year, while about 1.1 billion people lacked safe drinking water [12]. Consequent to the realization of the potential health hazards that may result from contaminated drinking water, contamination of drinking water from any source is therefore of primary importance because of the danger and risk of water-borne diseases [13]. To live in good health, people need to have access to good quality water in adequate quantity.
It is often assumed that natural, uncontaminated water from deep wells is clean and healthy, and this is usually true with regard to bacteriological composition. However, bacterial pollution of water sources may occur and is mostly derived from watershed corrosion as well as drainage from sewage, swamps or soil with high humus content. This type of hazard exists particularly in limestone areas where underground chambers or fissures may permit water to flow into the freely moving streams without caution for human drinking purposes because of the inherent risk [10,14-17].
In August, 2011, a devastating flood hit the city of Ibadan, Nigeria leading to loss of several lives. After the flood there was subsequent outbreak of cholera that claimed 18 lives and left several hospitalized. Prior to the cholera incidence was the general knowledge that sachet water sources were was not sterile and that they may contain bacteria from naturally occurring sources as well as those introduced during manufacturing and consumer handling [18]. The aim of the study was to ascertain if sachet water, popularly called pure water, was actually indeed pure or poor after the flood disaster. The specific objectives were:
1) To isolate microorganisms present in sachet water;
2) To enumerate microorganisms present in sachet water;
3) To characterize isolates obtained using biochemical parameters;
4) To determine some physicochemical properties of sachet water
2. Materials and Methods
The study was carried out in Ibadan, a city in southwest of Nigeria with five local government areas: the Ibadan South West, Ibadan South East, Ibadan North West, Ibadan North East and Oluyole Local Government areas. The population of Ibadan was estimated to be 4.1 million people in 2009 [1].
2.1. Study Design
The study is descriptive in nature and it involved a random sampling designed to provide baseline data on the bacteriological quality of sachet packaged water through laboratory analysis. Samples were analyzed within 12 h of collection.
2.2. Study Sample
Sachet water was drawn randomly from a street vendor from each of the five local Government Areas of Ibadan. Two bags were randomly picked from each bag of 20 sachets and sampling was done three times. The same brand was collected three times because the brands were written on each sachet and analyzed within 12 hours of collection. The information on the sachets was noted and sachet water companies were visited. All companies visited had their own boles sunk within the vicinity of the company.
2.3. Physicochemical Properties of Sachet Water
Physicochemical properties examined were pH, colour, turbidity, residual chlorine and iron content. pH was determined using a pH meter (Engineered Systems and Design Serial No. 574924) USA, residual chlorine was analyzed using DPD No. 1 tablets, iron levels were determined using DPD Iron No.1 and colour and turbidity were assessed visually.
2.4. Isolation of Microorganisms
One milliliter of each sachet water was serially diluted and I mL of an appropriate dilution was inoculated on nutrient agar plates in triplicate for total viable counts. For coliform count, faecal streptococcal counts, 100 mL of each sachet water was filtered through a membrane filter (size 0.45 µm; batch No. BM 9KN3121) and plated on MacConkey agar and Eosin Methylene Blue agar plates and incubated at 37˚C for 24 hours, after which visible colonies were counted and results were expressed in cfu/mL. The choice of Eosin Methylene Blue for Vibrio cholerae is due to the fact that it can grow on many kinds of media including Thiosulphate Citrate Bile Sucrose Agar, which is very expensive.
2.5. Characterization and Identification of Isolates
This was done according to standard methods described by Olutiola et al. [19]. The methods involved Gram staining, morphological, cultural and biochemical characteristics (catalase, coagulase, oxidase, methyl red, Voges Proskauer, citrate reduction, indole, and sugar fermentations test).
2.6. Test for Coliforms
(a) Presumptive test:
Single strength lactose broth was inoculated with 0.1 mL of water sample and incubated at 37˚C for 24 to 48 h. The lactose broth tubes were observed for gas production after 24 hours of incubation. A gas production of 10% or more is taken as a presumptive test for coliforms.
(b) Confirmed test:
Two plates of Eosin Methylene plates were streaked with broth from presumptive positive tubes and incubated at 37˚C for 24 hours. Growth of bluish black colonies with metallic sheen confirms the presence of E. coli. Colonies of Enterobacter aerogenes, if present, appeared brownish and tend to coalesce.
(c) Completed test:
Two confirmed coliform colonies were inoculated into lactose broth with Durham tubes and incubated at 37˚C for 24 hours for gas production. Evidence of gas production was an indication of a completed coliform test.
2.7. Statistical Analysis
All results were analyzed using Analysis of Variance and Student t test.
3. Results
The pH of the sachet water ranged between 6.3 - 8.7. Twenty eight percent of the screened water samples had pH values above the WHO approved range of 6.4 - 7.6 (Table 1). No residual chlorine was detected. It was also gathered that most sachet water companies do not chlorinate their water and so results of residual chlorine was negative. Iron levels were minimal in all water samples. Thirty percent of water samples had faecal coliforms above the recommended WHO standard of zero coliforms per 100 mL (Table 2). Sugar fermentation results revealed Escherichia coli had the highest incidence of 17%. Other probable isolates were Staphylococcus aureus, Bacillus sp., Enterobacter aerogenes, Flavobacterium sp., Proteus sp., Klebsiella sp., Streptococcus faecalis, Acinetobacter sp. Only one sample of sachet water had Gram negative cocoid bacilli that were curved, indicating Vibrio sp. (Figure 1). Vibrio cholerae was confirmed using sugar fermentation tests.

Table 1. Physicochemical parameters of sachet water sold in Ibadan and its environment.

Table 2. Total bacterial and coliform counts in sachet water sold in Ibadan and its environs.
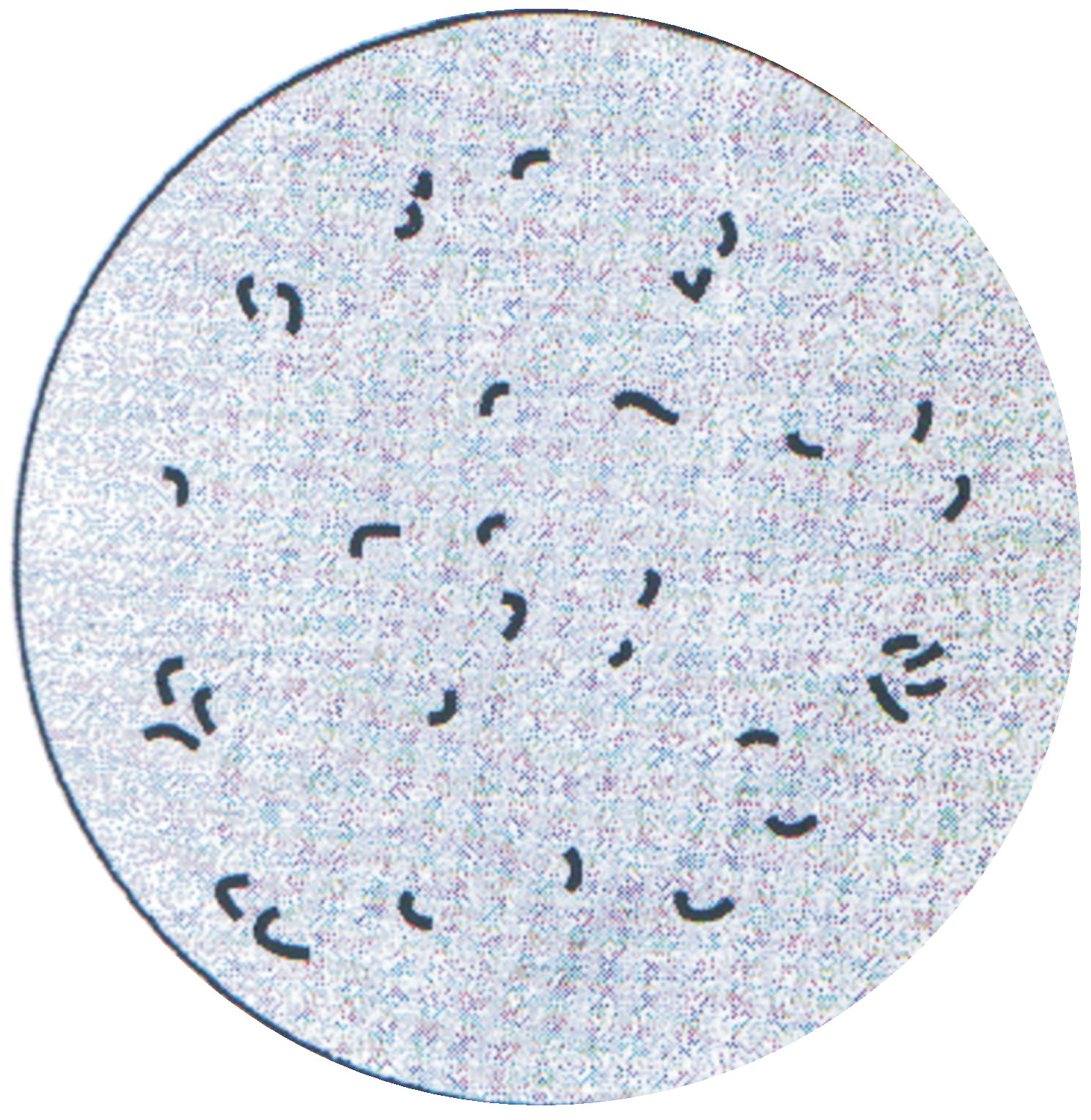
Figure 1. Isolate of Vibrio cholerae from a sample of water cultured on Eosin Methylene Blue agar.
4. Discussion
Water-borne diseases are caused by pathogenic microorganisms which are directly transmitted when contaminated water is consumed. According to the World Health Organization, diarrhoeal disease accounts for an estimated 4.1% of the total daily global burden and is responsible for the deaths of 1.8 million people every year. It was estimated that 88% of that burden is attributable to unsafe water supply, sanitation and hygiene [21].
This study is unique and quite different from previous studies because in 2011, a severe flood in the city of Ibadan caused several deaths and thereafter, a devastating cholera broke out leading to several hospitalizations and 18 recorded deaths. Several cases of diarrhea in Nigeria and most developing countries are not reported at the Ministry of Health and often the numbers of mortalities in the environment are higher than numbers given by the Federal Ministry of Statistics.
Water samples sold as sachet water were analyzed and Table 1 shows their physicochemical properties. The physicochemical quality affects water acceptability because of its aesthetic considerations. Results show that water samples were colourless, odourless, had no residual chlorine and were not turbid. Only 92% met WHO standard of being tasteless and 72% of the sachet waters met the WHO pH standard of 6.4 - 7.6. pH levels of less than 7 may cause severe corrosion of metals while at pH 8 , there is progressive decrease in the efficiency of chlorine disinfection process. An acceptable pH of drinking water is 6.4 - 7.6. In the absence of a distribution system, the acceptable range of pH may be broader [22]. pH affects various water treatment processes that contribute to the removal of viruses, bacteria and other harmful organisms; it could be claimed that pH has an ill-effect on health [23].
All sachet water analyzed had Total Dissolved Solids (TDS) below 500 mg/L. According to consumer ratings, any water with TDS of <500 mg/L is described as excellent [24] and greater than 1700 mg/L as unpalatable. Chemical substances leached into underground or surface water may be hazardous to health.
Tables 2 and 3 show the bacteriological load seen in the screened sachet water samples. A bacteriologically pure water is one that is free from faecal pollution. Results showed the presence of pathogenic organisms at levels above the approved WHO standard in thirteen sachet water samples which are consequently termed unsatisfactory that is unhealthy for consumption and requiring extensive treatment before use. Ten other samples were totally unacceptable and sources of such water samples should be avoided and only be used when unavoidable even after treatment [21,23]. The likely causes of unacceptable water will be seepage from septic tanks, cow dungs which litters the roads and generally unhygienic practices contributing to the Enterobacteriaceae counts observed in affected boreholes used in making sachet water. Detection of coliforms shows the danger of faecal pollution and the consequent hazard of contracting diseases. The presence of pathogenic organisms in sachet

Table 3. Microorganisms isolated from sachet water sold in Ibadan and its environs.
water has been previously reported by Olaoye and Onilude [25]. It has been reported that typical enteropathogenic Escherichia coli is a leading cause of infantile diarrhea in developing countries, whereas this is rare in industrialized countries [26].
Organisms isolated included Escherichia coli, Staphylococcus aureus, Enterobacter aerogenes, Flavobacterium sp., Proteus mirabilis, Acinetobacter, and Vibrio cholerae. Most samples had multiple pathogens as coliform counts indicated not only E. coli, but other members of the Enterobacteriaceae e.g., Salmonella, Shigella, Campylobacter, etc. These bacteria have been implicated in water related diseases [27].
Poor personal hygiene of handlers and environmental hygiene have been reported to contribute significantly to the level of contamination in packed water in developing countries [28]. The poor microbiological quality of drinking water samples have been reported in other countries [29-31].
The detection of Escherichia coli, E. aerogenes and Vibrio cholerae implied that the water samples might have been potentially contaminated with faecal matter and are therefore not safe for human consumption. WHO [23] has reported that occurrence of pathogens or indicator organisms in water sources depends on the intrinsic physical and chemical characteristics of the catchment area, the magnitude and range of the human activities and animal sources that release pathogens to the environment [21].
The detection of Vibrio in a water sample (Figure 1) indicates that the water sample is contaminated with faecal matter or the producers of the particular brand of sachet water contaminated the water by unhygienic practices from their faecal waste [32] Vibrio cholerae is the organism that causes cholera, which is a dreaded disease worldwide. The disease is characterized by profuse diarrhea and vomiting [33].
The disease resurgence in Ibadan—the third most populous city south of the Sahara occurred in August, 2011 after a devastating flood that hit the city after 12 hours of torrential rainfall. The flood contributed in no small measure to the sporadic occurrence of cholera in some parts of the city. This led to much agony and mortality as reported by The Nation Newspaper where 945 cases were reported and 11 deaths [34]. Most of the patients were rejected in the hospitals on the grounds that there were no beds for admission. According to Lawoyin et al. [35], the disease had occurred in the city first in 1970 and is still reoccurring sporadically due to poor sanitation of the inhabitants.
From the 100 sachet water screened, it is noteworthy that 70% met the WHO standard of zero colifoms; 7% of sachet water had 2 - 3 coliforms, 13% had 4 - 10 coliforms and 10% had 10 - 100 coliforms. Only one brand of sachet water located in a particular area in the city had Vibrio cholerae. A visit to the company clearly revealed that the environment was not ideal and sanitary practices were not adhered to. There was no UV light for sterilization of water samples.
5. Conclusion
In conclusion, due to the public health significance of cholera, the government should attend to the outbreaks of cholera with prompt attention and take proactive steps to halt its future resurgence. Although the present findings have been forwarded to the Nigerian Regulatory Agency called the National Agency for Food, Drug Administration and Control (NAFDAC) for prompt action, and NAFDAC has already undertaken its best prompt action by sealing off the factory, much is still desired in the area of public health education because severe health implications like cholera and other gastrointestinal diseases outbreaks can occur and consumer protection measures on news media in the local languages spoken by the people, routine monthly sampling of all water samples before being injected into the market and finally the possible development of vaccine against cholera.
REFERENCES
- Federal Office Statistics (FOS), “Population of Ibadan,” 2009. http://www.wideopenaccess.net//WACREN
- P. H. Gleick, “Water and Terrorism,” Water Policy, Vol. 8, No. 6, 2006, pp. 481-503. doi:10.2166/wp.2006.035
- A. Godfree and J. Farrell, “Processes for Managing Pathogens,” Journal of Environmental Quality, Vol. 34, No. 1, 2005, pp. 105-113. doi:10.2134/jeq2005.0105
- H. J. Brass, “Status of the Drinking Water Standards Program in the United States,” Water, Air and Soil Pollution, Vol. 123, No. 1-4, 2000, pp. 1-9. doi:10.1023/A:1005294019383
- S. E. Smith, “What Is Potable Water,” 2012. http://www.wisegreek.com/what -is-potablewater.htm
- M. A. Flusche, G. Seltzer, D. Rodbell, D. Siegel and S. Samson, “Constraining Water Sources and Hydrologic Processes from the Isotopic Analysis of Water and Dissolved Strontium, Lake Junin, Peru,” Journal of Hydrology, Vol. 312, No. 1-4, 2005, pp. 1-13. doi:10.1016/j.jhydrol.2005.02.021
- P. A. G. M. Scheren, H. A. Zanting and A. M. C. Lemmens, “Estimation of Water Pollution Sources in Lake Victoria, East Africa: Application and Elaboration of Rapid Assessment Methodology,” Journal of Environmental Management, Vol. 58, No. 4, 2000, pp. 235-248. doi:10.1006/jema.2000.0322
- American Public Health Association (APHA), “Standard Methods for the Examination of Water and Waste Water,” American Public Health Association (APHA), Washington DC, 2002.
- C. Riemann, K. Bjorvatnb, B. Frengstand, Z. Melaku, R. Tarele-Haimanot and U. Siewers, “Drinking Water Quality in Ethiopia Section of the East African Rift Valley,” Science of The Total Environment, Vol. 311, No. 1-3, 2003, pp. 65-72. doi:10.1016/S0048-9697(03)00137-2
- T. Westrell, “Microbial Risk Assessment and Its Implications for Risk Management in Urban Water System,” Linköping University Electronic Press, Linköping, 2004.
- A. Y. Sangodoyin, “Consideration on Contamination of Ground Water by Waste Disposal System in Nigeria,” Environmental Technology, Vol. 14, No. 10, 1993, pp. 957- 964. doi:10.1080/09593339309385370
- T. Clasen, W.-P. Schmidt, T. Rabie, I. Roberts and S. Caincross, “Interventions to Improve Water Quality for Preventing Diarrhoea: Systematic Review and MetaAnalysis,” British Medical Journal, Vol. 334, No. 7597, 2007, pp. 782-785.
- L. Agard, C. Alexander, S. Green, M. Jackson, S. Patel and A. Adesiyun, “Microbial Quality of Water Supply to an Urban Community in Trinidad,” Journal of Food Protection, Vol. 65, No. 8, 2002, pp. 1297-1303.
- M. A. Borchardt, P. D. Bertz, S. K. Spencer and D. A. Battigelli, “Incidence of Enteric Viruses in Groundwater from Household Wells in Wisconsin,” Applied Environmental Microbiology, Vol. 69, No. 2, 2003, pp. 1172- 1180. doi:10.1128/AEM.69.2.1172-1180.2003
- D. Banks, A. K. Midtgard, G. Morland, C. Riemann, T. Strand, K. Bjorvatn and U. Siewers, “Is Pure Groundwater Safe to Drink?” Geology Today, Vol. 14, No. 3, 1998, pp. 104-113. doi:10.1046/j.1365-2451.1998.014003104.x
- M. M. Alghatani and M. H. Alghatani, “Environmental Situation in the Region of Assir—A Survey of the Current Conditions,” King Khalid University, Abha, 2000.
- Health Canada, “Guidelines for Canadian Drinking Water Quality: Guideline Technical Document—Escherichia coli,” Water Quality and Health Bureau, Healthy Environment and Consumer Safety Branch, Ottawa, 2000.
- D. Cabral and P. Fernández, “Fungal Spoilage of Bottled Mineral Water,” International Journal of Food Microbiology, Vol. 72, No. 1-2, 2002, pp. 73-76. doi:10.1016/S0168-1605(01)00628-6
- P. O. Olutiola, O. Famurewa and H. G. Suntay, “An Introduction to General Microbiology: A Practical Approach,” Hygiene Institut der Universitat Heidelberg, Heidelberg, 1991.
- World Health Organization, “Guidelines for Drinking Water Quality. Addendum: Microbiological Agents in Drink Water,” WHO, Geneva, 2001.
- World Health Organization, “Guidelines for Drinking Water,” WHO, Geneva, 2005.
- Health Canada, “Environmental and Workplace Health,” 2009. http://www.hc-sc.gc.ca/ewh-semt/pubs/water-eau-/ph/index-eng.php
- World Health Organization, “Guidelines for Drinking Water Quality,” WHO, Geneva, 2004.
- WHO/SDE/WSH, “Chemical Hazards in Drinking-Water—Total Dissolved Solids,” 2003. http://www.who.int/water_sanitation_health/dwq/chemicals/tds
- O. A. Olaoye and A. A. Onilude “Assessment of Microbiological Quality of Sachet-Packaged Drinking Water in Western Nigeria and Its Public Health Significance,” Public Health, Vol. 123, No. 11, 2009, pp. 729-734. doi:10.1016/j.puhe.2009.09.015
- K. Aria, E. Tris and S. Dewi, “Esherichia coli Contamination of Babies’ Food-Serving Utensils in a District of West Sumatra, Indonesia,” WHO South-East Asia Journal of Public Health, Vol. 1, No. 1, 2012, pp. 20-27.
- T. A. Edge and S. Hill, “Occurrence of Antibiotic Resistance in Escherichia coli from Surface Waters and Fecal Pollution Sources near Hamilton, Ontario,” Canadian Journal of Microbiology, Vol. 51, No. 6, 2005, pp. 501- 505. doi:10.1139/w05-028
- N. J. Ashbolt, “Microbial Contamination of Drinking Water and Disease Outcome in Developing Regions,” Toxicology, Vol. 198, No. 1-3, 2004, pp. 229-238. doi:10.1016/j.tox.2004.01.030
- K. Obiri-Danso, A. Olore-Hanson and K. Jones, “The Microbiological Quality of Drinking Water Sold on the Streets in Kumasi, Ghana,” Letters in Applied Microbiology, Vol. 37, No. 4, 2005, pp. 334-339. doi:10.1046/j.1472-765X.2003.01403.x
- M. M. Yassin, S. S. Amr and H. M. Al-Najar, “Assessment of Microbiological Water Quality and Its Relation to Human Health in Gaza Governorates, Gaza Strip,” Public Health, Vol. 120, No. 12, 2006, pp. 1177-1187. doi:10.1016/j.puhe.2006.07.026
- A. C. Dada, “Sachet Water Phenomenon in Nigeria: Assessment of the Potential Health Impacts,” African Journal of Microbiology Research, Vol. 3, No. 1, 2009, pp. 15-21.
- P. Tallon, B. Magajna, C. Lofranco and K. T. Leung, “Microbial Indicators of Faecal Contamination in Water: A Current Perspective,” Water, Air and Soil Pollution, Vol. 166, No. 1-4, 2005, pp. 139-166. doi:10.1007/s11270-005-7905-4
- M. R. Adams and M. O. Moss, “Food Microbiology,” The Royal Society of Chemistry, Cambridge, 2008.
- The Nation, “Ibadan Cholera Outbreak,” 2011. http://www.thenationonlineng.net/2011/16905-Ibadan-cholera-outbreak-under-control-says-oyo-govt.html
- T. O. Lawoyin, N. A. Ogunbodede, E. A. Olumide and M. O. Onadeko, “Outbreak of Cholera in Ibadan, Nigeria,” European Journal of Epidemiology, Vol. 15, No. 4, 1999, pp. 367-370.
NOTES
*Corresponding author.

