Open Journal of Ophthalmology
Vol.4 No.2(2014), Article ID:45871,5 pages DOI:10.4236/ojoph.2014.42006
Surgical Correction for Paralytic Strabismus Using T-Plate Anchor
Anwar Ramadhan1*, Raed Behbehani2, Mishari Dahrab2, Haitham Murad1
1Department of Oral and Maxillofacial Surgery, Amiri Hospital, Kuwait City, Kuwait
2Al-Bahar Ophthalmology Center, Kuwait City, Kuwait
Email: *dr.anwarramadhan@hotmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 16 January 2014; revised 15 March 2014; accepted 4 April 2014
ABSTRACT
External or internal ophthalmoloplegia will result in a complete or a partial ocular dysmotility leading to a debilitating and variable manifest binocular diplopia for a majority of the patients. Complete third, forth and sixth nerve cranial nerve palsies are among the many number of etiologies appearing as paralytic strabismus. Successful clinical management, elimination of symptomatic diplopia in the primary field of gaze and increased binocular field of motor and sensory fusion as a result of the oculomotor nerve (III) palsy are challenging tasks for physicians facing this difficult clinical entity. Here we report a novel surgical technique in the clinical management of this disease through suture-fixation of medial rectus muscle onto Titanium plate (T-plate) already anchored into the nasal orbital wall.
Keywords
T-Plate, Paralytic Strabismus, Anchor

1. Introduction
External or internal ophthalmoloplegia can cause complete or a partial ocular dysmotility leading to a debilitating and variable manifest binocular diplopia [1] [2] . The multiple extra-ocular muscle involvement in partial or complete paralysis of the oculomotor nerve can render the surgical correction challenging. Variety of surgical technique is available for treatment of this type of strabismus ranging from recession/resection to transposition of the extraocular muscles [1] -[5] . Surgical correction of Ptosis requires large resection of the levator muscule or the use of a Frontalis sling technique [6] [7] .
Recently, techniques of fixation of the effected muscles to the periosteum or directly onto bone have been reported [8] -[11] . With the use of non-absorbable suture or any autologous vascularized or non-vascularized tissue, the paralytic muscle can be fixed onto the periosteum to neutralize the force generated by the opposing non-affected muscle [8] -[14] .
Herein, we report a case of strabismus as a result of oculmotor nerve palsy in which we utilize a T-plate anchored to the medial orbital wall of the orbit to be a fixation site for the paralytic medical rectus muscle.
2. Case Report
A 26-year-old male presented with a gradual onset of right upper lid ptosis (Figure 1(A)) and a outward drifting of his right eye for the past year. His past ocular history includes history of deep amblyopia in right eye and exotropia since childhood, requiring 2 strabismus surgeries for correction of the exotropia at the ages of 6 and 17 years both of which were done in the right eye.
3. Clinical Course and Findings
At the presentation, his best-corrected visual acuity was 20/300 right and 20/20 left at distance. He had a moderate right upper lid ptosis and a semi-dilated noneactive right pupil with no relative afferent pupillary defect. Extraocular motility examination revealed a significant limitation of elevation and depression as well as complete lack of adduction in the right eye (Figures 1(B)-(D)). Active force generation was absent for the medial rectus in the right eye on adduction. Forced duction test was not performed and saccades were slow in all gaze directions with normal pursuits. Fundus examination was normal with no detectable significant torsion noticed on fundus examination. We diagnosed the patient with a pupillary involving oculomotor nerve pals. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the brain and orbit showed a right cavernous sinus meningioma. He was referred to the neurosurgery service and was treated with gamma knife radiosurgery. He presented to the ophthalmology clinic a year later complaining of binocular diplopia and worsening of the right upper lid ptosis. He had a large exotropia and absent elevation, depression and adduction. (Figure 1(B)) He had large angle exotropia of the right eye measuring at least 90 prism diopters using the Hirschberg method. His right marginal reflex distance (MRD1) was −1 mm right and 5 mm left. Right levator muscle function was zero and was normal (18 mm) in the left. Due to the complete paresis of the supeior, inferior and medial recti and 2 previous strabismus surgery involving recession of the lateral restus and resection of the medial rectus, a T-plate globe fixation was discussed with the patient as an alternative treatment option. Moreover, performing surgery on multiple muscles would have increased the probability of anterior segment ischemia. Risks, benefits, alternatives and potential complications of surgery including complete lack of eye motility in the right eye following this surgery was also discussed with the patient.
Our target surgical outcome was to have the patient orthophoric in the primary position. In the same surgery, a concomitant frontalis sling procedure would be performed to correct the right ptosis.
4. Surgical Technique
Following general anesthesia induction, the medial canthal area was infiltrated 2 ml solution of 2% xylocaine and 1:100,000 epinephrine solution. In order to identify medial canthal ligament, we made a 1.5 cm lynch incision between medical canthus and nasal dorsum (Figure 2(A)).

Figure 1. Preoperative photos show severe exotropia in the right eye with complete blepharoptosis in the right upper eyelid and severly limited right eye motility (A)-(D).
The dissection was extended posteriorly under the periosteum onto the medial orbital wall with care to avoid injury of anterior and posterior ethmoid arteries.
A T-plate (3 holes crossbar 1 mm × 4 holes shaft 20 mm, Synthes CMF system, Switzerland) was inserted with the crossbar on the anterior lacrimal crest and secured over the anterior lacrimal crest with screws. A 5.0-prolene (Ethicon, USA) suture that would later secure the globe to the plate was sutured into the last hole of the T-plate (Figure 2(B)).
Through a limbal conjunctival peritomy, both the medial and lateral recti muscles were identified. The lateral rectus was identified and in this case it was found to be 20 mm posterior to the limbus. Following disinsertion, it was allowed to fall back freely. The 5.0 non-absorbable suture was passed from the medial peri-orbita at which point it was secured into the sclera of the globe (Figure 2(A)). Adjustment to obtain orthotropic alignment of the right eye was made before we tied the final knot. The conjunctiva was closed with an 8-0 vicryl (Ethicon, USA) The Lynch incision was closed with 6.0 prolene sutures.
We used Ptose up 2 mm (FCI Ophthalmic Inc., France) to form a pentagonal frontalis sling for the correction of ptosis.
5. Postoperative
On day #1, the patient exhibited mild or sever signs of exposure keratopathy, which resolved over the next week. His alignment showed a small right exotropia with no ocular motility in the right eye. At the last follow-up examination months later, he had 10-prism diopter of exotropia at near and distance. He reported no subjective diplopia in the primary gaze position (Figure 3).
6. Discussion
We report a case of a paralytic strabismus due to an oculomotor nerve palsy from a cavernous sinus meningioma

Figure 2. (A) Suture 5.0 Nylon being passed to the scelera; (B) T-plate fixed on the nasal bone.
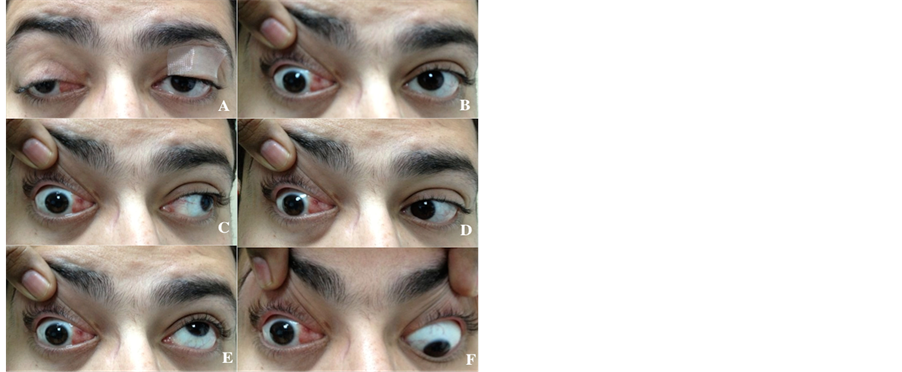
Figure 3. Postoperative photos 18 months, show mild recurrent exotropia in the right eye and limited eye motility in the right (A)-(F).
which was successfully managed by periosteal fixation of the sclera to an anchored T-plate in the medial orbital periosteum. In this patient, the diagnosis was probably delayed because of his pre-existing exotropia from childhood as this may have masked the clinical presentation of progressive exotropia resulting from oculomotor nerve palsy resulting from a cavernous sinus lesion. After using T-plate fixation technique described herein, the patient achieved good initial alignment in primary position with some residual exotropia after 18 month follow up (Figure 3). Numerous surgical approaches have been described in the literature based on the etiologys [1] -[5] [8] -[14] . The use of screw as anchor points to the extraocular muscles to bone was initially described in 2006 [11] . Later, Tse et al. reported the first approach for the corrections of seven cases of paralytic strabismus (III and VI cranial nerves) by using T-Plate fixation out of a particular extraocular muscle for aligning the eye in primary position.
He showed no relapse of alignment or plate infection after almost 60 months follow up [8] . We think that the technique we used has more longevity compared to direct fixation of the extraocular muscles to the periosteum. Moreover, many of those patients would have had many strabismus surgeries on multiple extraocular muscles and using the sclera as anchor point, the risk of anterior segment ischemia would be less. The titanium plate is not a magnetic metal and thus its placement would not preclude magnetic resonance imaging in the future should it be needed.
Recently, many reports were published on non-exraocular method for correcting severe or paralytic strabismus [8] -[14] . Kuldeep et al. performed a technique for globe fixation on 5 cases with paralytic strabismus due to oculomotor nerve palsy with the use of non-absorbable suture with fixation the medial rectus muscle to the medial palpebral ligament and periosteum. He reported successful alignment in four patients, and one patient with relapse (extropia) in after 6 months to 9 months of follow-up [9] . Possible complications arising from our procedure can include a medial scar from the incision an inadvertent injury to the lacrimal sac, all of which can be avoided by meticulous surgical technique.
Similarly, Rohit et al. described a technique anchoring 14 globes into medial wall of the orbit through the periosteum, and the alignment satisfaction was 92.8% [10] .
T-plate anchor is a safe technique and spares the need to operate on multiple extraocular muscles with minimal to no risk of anterior segment ischemia. Moreover, it may be ideal for the case of previously operated eye for strabismus in which scars and adhesions may limit the amount of recession, or resection of the muscles.
7. Conclusion
The T-plate method is an easy technique with good satisfactory result for alignment severe and complete paralytic strabismus. However, larger series of patients with longer follow up are needed in the assessment of this technique in correcting severe paralytic strabismus.
Conflict of Interest
This research received no specific grant from any funding agency in the public, commercial or not for-profit sectors. The authors have no financial interest in any aspect of this paper or any conflict of interest.
References
- Prasad, S. and Volpe, N.J. (2010) Paralytic Strabismus: Third, Fourth, and Sixth Nerve Palsy. Neurologic Clinics, 28, 803-833. http://dx.doi.org/10.1016/j.ncl.2010.04.001
- Buckley, E.G. (2008) General Principles in the Surgical Treatment of Paralytic Strabismus. American Orthoptic Journal, 58, 49-59. http://dx.doi.org/10.3368/aoj.58.1.49
- Yonghong, J., Kanxing, Z., Wei, L., et al. (2008) Surgical Management of Large-Angle Incomitant Strabismus in Patients with Oculomotor Nerve Palsy. JAAPOS, 12, 49-53. http://dx.doi.org/10.1016/j.jaapos.2007.07.008
- Kushner, B.J. (1999) Surgical Treatment of Paralysis of the Inferior Division of the Oculomotor Nerve. Archives of Ophthalmology, 117, 485-489. http://dx.doi.org/10.1001/archopht.117.4.485
- Maruo, T., Iwashige, H., Kubota, N., et al. (1996) Results of Surgery for Paralytic Exotropia Due to Oculomotor Palsy. Ophthalmologica, 210, 163-167. http://dx.doi.org/10.1159/000310699
- Sokol, J.A., Thornton, I.L., Lee, H.B., et al. (2011) Modified Frontalis Suspension Technique with Review of Large Series. Ophthalmic Plastic & Reconstructive Surgery, 27, 211-215.
- Park, D.H., Choi, W.S., Yoon, S.H., et al. (2007) Comparison of Levator Resection and Frontalis Muscle Transfer in the Treatment of Severe Blepharoptosis. Annals of Plastic Surgery, 59, 388-392. http://dx.doi.org/10.1097/01.sap.0000258456.24810.c8
- Tse, D.T., Shriver, E.M., Krantz, K.B., et al. (2010) The Use of Titanium T-Plate as Platform for Globe Alignment in Severe Paralytic and Restrictive Strabismus. American Journal of Ophthalmology, 150, 404-411. http://dx.doi.org/10.1016/j.ajo.2010.03.029
- Srivastava, K.K., Sundaresh, K. and Vijayalakshmi, P. (2004) A New Surgical Technique for Ocular Fixation in Congenital Third Nerve Palsy. JAAPOS, 8, 371-377. http://dx.doi.org/10.1016/j.jaapos.2004.01.015
- Saxena, R., Sinha, A., Sharma, P., et al. (2009) Precaruncular Approach for Medial Orbital Wall Periosteal Anchoring of the Globe in Oculomotor Nerve Palsy. JAAPOS, 13, 578-582. http://dx.doi.org/10.1016/j.jaapos.2009.11.003
- Ela-Dalman, N., Schwarcz, R.M. and Velez, F.G. (2006) Suture Fixation System as Globe Tethers in Severe Paralytic Strabismus. JAAPOS, 10, 371-372. http://dx.doi.org/10.1016/j.jaapos.2006.02.012
- Goldberg, R.A., Rosenbaum, A.L. and Tong, J.T. (2000) Use of Apically Based Periosteal Flaps as Globe Tethers in Severe Paretic Strabismus. Archives of Ophthalmology, 118, 431-437. http://dx.doi.org/10.1001/archopht.118.3.431
- Awad, A.H., Shin, G.S., Rosenbaum, A.L., et al. (1997) Autogenous Fascia Augmentation of a Partially Extirpated Muscle with a Subperiosteal Medial Orbitotomy Approach. JAAPOS, 1, 138-142. http://dx.doi.org/10.1016/S1091-8531(97)90054-9
NOTES

*Corresponding author.

