Epidemiology of Renal Failure in Children at the Pediatric University Hospital Charles De-Gaulle of Ouagadougou (Burkina Faso) ()
Received 20 February 2016; accepted 17 March 2016; published 21 March 2016

1. Introduction
The incidence of acute renal failure (ARF) in the general population is about 2000 to 3000 per million persons per year for mild and moderate ARF and 200 to 300 per million persons for ARF requiring renal replacement therapy [1] . Pediatric data on the epidemiology of ARF are rare; they vary depending on the country. Overall, the prevalence of ARF is growing all over the world [2] . The situation in tropical Africa seems to be more alarming. Indeed, some environmental factors (infectious, acute dehydration) and socio-cultural factors (traditional, over-the-counter products use) in this region of the world contribute to increasing the risk of ARF [3] . CRF, which may be a complication, is a major public health issue because of its increasing prevalence, severity and the high cost related to the treatment. In Burkina Faso, renal failure (RF) data are particularly rare in children. The hospital incidence of ARF was 19.6 cases per year [Kiendrebeogo; personal data] in the Department of Pediatrics of University Hospital Center Yalgado Ouedraogo in Ouagadougou, and a prevalence of 1.79% over six months was noted in the Department of Pediatrics of CHU-SS [Nebie; personal data]. RF cases are frequently treated at the Pediatric University Hospital Center Charles De-Gaulle (PUHC-CDG) despite difficulties related to the lack medical equipment and the absence of specialist in pediatric nephrology, among others. It is in such context that we conducted this study in order to know the epidemiology of RF in the Department of Pediatrics of the PUHC-CDG.
2. Patients and Methods
We conducted a retrospective study, over a period of three years, of medical records of in-patients from January 1, 2011 to December 31, 2013. It took place in the department of Pediatrics at the PUHC-CDG in Ouagadougou, Burkina Faso. In this department, which has no nephrologist, pediatric blood pressure monitors and urine test strips are not consistently available. These activities were disturbed for moments by repair works from 2011 to 2013. The paraclinic workup was done in another UHC or in a private health structure whenever it was not possible at the PUHC-CDG.
We included in the study all children between three and fifteen years during the study period, who were diagnosed with RF at the admission or during hospitalization. During the period covered by the study, there wasn’t a treatment protocol for renal failure. We retained the operational definitions below:
・ Renal failure (RF): glomerular filtration rate (GFR) less than 80 mL/min/1.73m2. GFR was estimated using the formula of Pottel et al. [4] :
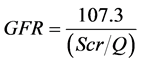
GFR: glomerular filtration rate expressed in mL/min/1.73m2. SCR: serum creatinine expressed in mg/dL (μmol/L: 88.4). Q = (00.0270 × Age) + 0.2329
ü The renal failure was acute (ARF) in the event of normalization of the GFR before three months. This ARF was considered functional [5] in the situations that can cause renal hypoperfusion: fluid and blood loss (acute hemorrhage, dehydration, the third sector), shock. The ARF was organic [6] in case of presumed glomerular, tubular, or interstitial vascular injury. Obstructive ARF was confirmed by highlighting bilateral dilation (or on single kidney) of pyelocaliceal cavities on renal ultrasound.
ü The Renal failure was considered chronic (CRF) in cases of already known CRF or persistence of RF beyond three months.
ü For other cases of RF, we did not have enough data to categorize them as ARF or CRF. Therefore, theywereconsideredunclassifiable (URF).
・ Hypertension (HTN): we used the formulas developed by Somu et al. [7] , which allow to estimate the 95th percentile (in mm Hg) simply on the basis of the age in years, regardless of the gender:
ü Systolic value (95th percentile): 1 - 17 years = 100 + (age × 2)
ü Diastolic value (95th percentile): 1 - 10 years = 60 + (age × 2); 11 - 17 years old = 70 + age.
We collected sociodemographic data, the mode and reasons of admission into the department, personal and family medical history, clinical and paraclinical data at admission time, treatment modalities, and outcome of patients. The mode of admission was a “reference” If the patient came from a lower level in the health pyramid of Burkina Faso, and “transfer” if the patient came from another department of the UPHC-CDG or another UHC.
Presumed etiologies were identified. The elements of their diagnosis were those commonly accepted. For example, the diagnosis of severe malaria was based on the WHO definition. We didn’t have any results of dengue fever serology or assay of glucose-6-phosphate dehydrogenase activity.
The data was introduced and processed in a computer using Epi Info software 3.5.1. The comparison of qualitative variables was done by using the khi2 test and that of quantitative variables by using the analysis of variance test. The statistical significance of these tests was reached for p < 0.05.
3. Results
3.1. Sociodemographic Data
One hundred nineteen patients admitted into the department during the study period had renal failure, a hospital incidence rate of 3.3%. The type of renal failure was ARF (34 cases or 28.6%), CRF (3 cases or 2.5%); and undetermined (82 cases or 68.9%). We found 10 patients in 2011, 29 patients in 2012 and 80 patients in 2013. The annual incidence of RF was 39.7 cases. It was 11.3 and 1 respectively for ARF and CRF.
The patients were divided into 70 boys (58.8%) and 49 girls (41.2%). Their average age was 6.7 ± 3.4 years old. They were divided into age-classes of [3 - 5[, [5 - 10[ and [10 - 15 [years old, which were respectively 45 (37.8%), 48 (40.3%) and 26 (21.8%). The residence places of patients were rural (33 cases or 28.7%), semiurban (15 cases or 13%) and urban (67 cases or 58.3%).
3.2. Mode and Reasons for Admission
In 71.8% of the cases, patients were referred from peripheral health facilities. The other patients were admitted either directly (20.5% of cases) or after being transferred from another department (7.7% of cases). The main reasons for consultation were fever (39 cases or 32.8%), vomiting (33 cases; 27.7%), anemia (27 cases; 22.7%), abdominal pain (25 cases; 21%) and edema of the lower limbs with or without swelling of the face (15 cases; 12.6%).
3.3. Clinical Signs
The clinical signs at the admission were dominated by fever (49.5%), jaundice (19.3%), edema of the lower limbs (16%), swelling of the face (15.1%), hemoglobinuria (16.8%), ascites (7.6%), and pharyngitis (5.9%). The blood pressure at the admission was measured for 33 patients (27.7% of patients). The average blood pressure readings were 123.9 ± 40.3 mm Hg (extremes: 80 and 230) and 77.6 ± 28.8 mm Hg (extremes: 35 and 150) respectively for the systolic blood pressure (SBP) and diastolic blood pressure (DBP).
3.4. Paraclinical Signs
The urea was measured for 112 patients (94.1%) at the admission. It was in average 16.6 ± 17.1 mmol/L (extremes: 1.2 and 80.1).
The Serum creatinine was available for 114 patients at the admission time. It was in average 251.5 ± 330.7 μmol/L (extremes: 40 and 1992). The estimated GFR of patients was 35.2 ± 22.2 mL/min/1.73m2 (extremes: 2 and 74.8).
During hospitalization, five patients or 4.2% of patients, showing normal renal function at the admission, had a decline in the estimated GFR. Their average serum creatinine that led to the diagnosis of RF was 224.7 ± 242.6 μmol/L (extremes: 45 and 595) and the estimated GFR was 46.9 ± 34.4 mL/min/1.73m2 (extremes: 5.9 and 78.7).
The other biochemical and hematological parameters measured at the admission are summarized in Table 1 and Table 2. The cytobacteriological analysis of the urine was done for 19 patients. Five patients had a urinary
![]()
Table 1. Mean serum creatinine and glomerular filtration rate (GFR) of patients at admission.
ARF: acute renal failure; CRF: chronic renal failure; URF: Unclassifiablerenalfailure. *: serum creatinine (expressed as μmol/L).
![]()
Table 2. Mean of biochemical and hematological parameters values depending on the type of kidney failure.
CRP: C Reactiv Protein; ARF: Acute renal failure; CRF: Chronicrenal failure; URF: Unclassifiable renal failure; n: number; %: percentage; m ± SD: mean ± standard deviation; PU: proteinuria; *: complet blood count parameters.
tract infection with urinary symptoms. The following germs have been isolated: Escherichia coli, Enterococcus sp, Staphylococcus aureus and Staphylococcus saprophyticus.
The abdominal and/or pelvic ultrasound was ordered for 44 patients or 37% of the patients. It has allowed us to find:
・ A normal ultrasound for seven patients or 15.9% of the 44 patients;
・ In the other cases we found the following anomalies:
ü kidneys: dedifferentiated kidneys (26 cases), hyperechogenicity (seven cases), irregular borders of the kidneys (one case);
ü ureters: bilateral stenosis (one case);
3.5. Mechanism of Renal Failure and Presumed Etiologies
The presumed mechanism of ARF was identified in 33 cases out of 34. It was:
・ Organic ARF in 26 cases (76.5% of cases of ARF): the context was a hemoglobinuria (23 cases recorded before or during hospitalization), and an acute post-streptococcal glomerulonephritis. The hemoglobinuria was linked to a severe malaria (17 cases) treated or not with quinine, a viral hepatonephritis B or C (5 cases) or probably drug-related (1 case);
・ Functional ARF in six cases (7.6%) related to a severe hypovolemia seen in nephrotic syndrome (3 cases) or a severe gastroenteritis (3 cases);
・ One case (2.9%) of obstructive ARF due to bilateral ureteral stenosis of unspecified cause in the medical record.
The presumed etiological damage in the three cases of CRF was chronic glomerulonephritis associated with nephrotic syndrome. In the 82 cases of URF, the mechanism of the renal damage could not be clarified.
The main presumed etiologies found in our patients were: severe malaria (52 cases), acute infectious gastroenteritis (8 cases), nephrotic syndrome (7 cases), acute post-streptococcal glomerulonephritis (6 cases), sepsis (5 cases), and viral hepatitis B or C (5 cases). The other presumed etiologies were represented each with three cases: envenomation by scorpion or snake bite, hypertension and typhoid fever.
3.6. Evolution
The average length of hospital stay was 10.2 ± 10.1 days (extremes: 1 and 61). The clinical-biological improvement was observed in 90 patients (75.6%). Thirteen (10.9%) were lost to follow-up. The remaining four patients were transferred in the department of nephrology and hemodialysis at the University Hospital Center Yalgado Ouedraogo of Ouagadougou.
Twelve patients (10.1%) with an average age of 6.5 ± 4.3 years old (extremes: 3 and 13) died. The main causes of death were: severe malaria (five cases), septicemia (two cases), severe anemia (two cases). The time of occurrence of death was 8.7 ± 16.8 days old (extremes: 1 and 61).
4. Discussion
Because of the retrospective nature of the study, all medical files did not contain all of the information sought. In addition, data on patients’ height were missing in the folders. Therefore, using the Schwartz formula to estimate the creatinine clearance was not possible. However, this formula remains the best-known and oldest in the evaluation of renal function in children [8] . So, we used the formula developed by Pottel et al. in 2012, because it is simple to use, and has a performance close to that of Schwartz and independent of the height measurement [4] . It is a good alternative to the Schwartz formula, particularly in our context where the measurement of the height is not always available [9] .
The rate of URF in our series was very high. It showed the difficulties encountered by practitioners in the paraclinical exploration of patients in Burkina Faso. These problems are mostly related to ignorance and/or lack of financial resources of patients or their relatives, failure or malfunction of the equipment of healthcare centers. The incidence of ARF and CRF in our study should therefore be discussed taking into account the underestimate (much more for the ARF) induced by the high rate of URF.
The hospital incidence of ARF in our series (11.3 cases/year) is comparable to that reported by other African authors such as Ifeoma et al. in Nigeria (11.7 cases/year) [10] , Bourquia et al. in Morocco (7 cases/year) [11] and Nebie in Burkina Faso (10.6 cases/year) [personal data]. It is however lower than Kiendrebeogo [personal data] and Balaka et al’s series [12] which were respectively 19.6 and 30.6 cases per year. The incidence reported by Balaka et al. concerned only cases of post-hemolytic RF.
The incidence of CRF was one case per year in our series. It is lower than that of Kiendrebeogo [personal data] (4 cases per year), Nebie [personal data] (5 cases in six months). In Africa, Lagou et al [13] in Ivory Coast, Balaka et al. [12] in Togo found respectively four and five cases per year. For information, in Europe where there are efficient diagnostic means, data from dialysis records showed an incidence of 119 cases per year in Italy, 35.8 cases per year in Belgium [14] .
The incidence variability of ARF and CRF is described by several authors [15] - [18] . Indeed, it varies from developed countries to developing countries [16] and also between the different ethnic groups [19] . It could be explained by the lack of consensual definition on ARF, the type of study and the method for recruiting patients. This difficulty related to the particular case of ARF could be lessened with the RIFLE (pRIFLE) criteria adapted to Pediatrics [20] . The use of these criteria remains, however, difficult in our conditions of practice.
The average age of CRF patients was 9.3 ± 3.2 years old. It is close to the average age of children in the series of Lagou et al. [13] (12.91 ± 2.34 years old) but greater than that found in some European countries [14] like in Italy (6.9 years old), France (6.3 years old), Sweden (3.3 years old). This difference between European and African authors can be explained by the low activity of early screening of chronic kidney diseases and late consultations in our context, favored by the vague and non-specific symptomatology of CRF.
We found an important number of boys with RF compared to girls, just as in the study of Nebie [personal data] and in the literature [10] [12] . Kiendrebeogo [personal data] had found a parity between gender and females were predominantly found in Shaheen et al’s study [21] . We have no explanation for this observation.
The main reasons for admission found in acute renal failure patients were diarrhea (100%), anemia (29.4%), fever (26.5%). They correspond to the most frequent reasons for hospitalization in children. The ARF has no specific manifestations and often complicates the most frequent diseases of a child.
In patients with CRF, lower limbs edema or puffiness of the face were the most frequent reasons. Although not specific to CRF, their presence should prompt the search for a CRF and its complications by the clinicians of health structures at the lower levels of the health pyramid. We should therefore reinforce the continuing medical education and better equip these health structures.
The blood pressure measurement was done at the admission for only 27.7% of the patients. The main reason for the low measurement rate was the lack of pediatric blood pressure monitors in the department. This would contribute to a sub-screening of hypertension and, consequently, that of the CRF. Indeed, hypertension is the circumstance of diagnosis of CRF in some cases.
About two-thirds of our patients did not do an ultrasound. The latter has an important place in the exploration of kidney diseases. Its absence is a big impediment in the diagnostic process. The non-availability of this diagnostic test as well as some biological tests for the vast majority of our patients is mainly related to its financial inaccessibility for parents of affected patients.
Organic ARF was the most frequently presumed ARF mechanism in our study. The histological damage was probably an acute tubular necrosis in light of the context of occurrence of these ARFs. The presumed etiologies were dominated by infectious diseases such as severe malaria (50%), viral hepatitis (14.7%), acute post-strep- tococcal glomerulonephritis (8.8%). Other African authors ( [11] [22] , personal data of Kiendrebeogo and Nebie) made the same observation. Dengue fever, viral disease, too often unrecognized, can simulate a severe malaria; it is increasingly cited as an infectious cause of ARF [23] . Better prevention and good management of infectious diseases, especially malaria, would reduce the incidence of ARF.
Regarding CRF, the suspected etiology was chronic glomerular nephropathy with nephrotic syndrome. Similar results have been reported in most of the African series ( [11] , personal data of Kiendrebeogo and Nebie), while the obstructive uropathies were the most found in the European series [14] . The high frequency of presumed chronic glomerular nephropathy is probably related to that of infectious diseases in our context. These are still common causes of glomerular nephropathy.
The mortality rate of 10.1% was very high, even though it was lower than that reported by Ladapo et al. [24] . This supports not only the severity of the cases but also the difficulties related to the lack of equipment, qualified staff, and the poverty of a large number of parents.
5. Conclusion
The incidence of RF was high at the PUHC-CDG of Ouagadougou. Its symptomatology was not specific. In light of the difficulties encountered in most public healthcare structures of the country in general, and at the PUHC-CDG in particular, the diagnosis of RF was founded only on the estimation of the GFR by using the formula of Pottel et al. This formula is independent of the height and weight that are simple parameters but not always available in our context. These same difficulties explain the high frequency of URF and the under-diag- nosis of hypertension that is sometimes the circumstance of discovery of RF, especially chronic renal failure. The improvement of specialized human resources, and equipment of the PUHC-CDG (with simple tools like the blood pressure monitor, the measuring rod and urinary strips), as well as sufficient subvention of the health cost by the state would certainly contribute to a better screening, etiological research, and secondary prevention of RF in the Department of Medical Pediatrics of the PUHC-CDG.
Conflict of Interest
None.
NOTES

*Corresponding author.