The Role of Gallium (Ga-67) Scintigraphy in the Diagnosis of Sarcoidosis ()
1. Introduction
Sarcoidosis is a systemic auto-inflammatory disease of unknown aetiology in which a lymphocytic inflammatory infiltration, non-caseating granulomas and, oftentimes, fibrosis is seen histologically. It most commonly affects the lungs and skin but can affect any organ in the body including the central nervous system [1] -[3] .
Women tend to be more commonly affected than men and symptoms usually develop before 50 years with a peak age of onset between 30 - 40 years [4] . Rarely, it affects children and the pattern is similar to that seen in adults. In Scandinavian women, a bimodal pattern has been documented with peaks at 25 - 29 years and 65 - 69 years [5] . Northern European countries have the highest reported rates of Sarcoidosis ranging from 5 - 40 cases per 100,000 of the population. In the United States it is more common in African American than Caucasian populations [4] . It has been reported that the disease may be more severe in black populations whereas Caucasian populations are more likely to have a less severe disease course [2] [4] -[6] .
Study of the epidemiology of Sarcoidosis is complicated considerably by the facts not only that many of the cases are asymptomatic but also that symptoms are often so non-specific that there is overlap with symptoms of other diseases. One of these is tuberculosis (TB) and it has been suggested that the prevalence of Sarcoidosis may be grossly underestimated in countries in which TB is common [7] .
A diagnosis of Sarcoidosis is based on 1) a compatible clinical picture, 2) non-caseating granulomas identified on biopsy and 3) imaging compatible with the diagnosis. This must, obviously, all be in the absence of any other identifiable cause.
Gallium (Ga-67) scintigraphy is a nuclear imaging technique used to identify areas of active inflammation. Its use in relation to Sarcoidosis is both as an adjunct to the initial diagnostic process and as a monitor of disease activity. In the case of Sarcoidosis affecting the nervous system, a neurological biopsy may be hazardous and so Ga-67 scintigraphy may also help to identify potential biopsy sites outside the nervous system. Whilst there is great variability in the pattern of abnormal uptake seen, reflecting the various sites of involvement by the disease, the “panda pattern” shows salivary gland uptake, and mediastinal and hilar node uptake leads to the “lambda pattern” (Figure 1). Both of these are considered specific for Sarcoidosis in the absence of histological confirmation [8] . The problem is that this pattern, whilst highly specific, is not sensitive, leading potentially to an underreporting of patients who may nonetheless have the disease.
This study looks at a series of 75 patients scanned in the Nuclear Medicine Department at the Royal Free Hospital, London, and aims to identify the sensitivity and specificity of Ga-67 scintigraphy where the indication for the scan is suspected Sarcoidosis and to investigate further the potential of this investigation to identify areas of granulomatous inflammation that might be amenable to biopsy in the special context of Sarcoidosis affecting the central nervous system.
2. Methods
The request forms for 259 consecutive Ga-67 scans carried out at the Royal Free Hospital, London, from 1st January 2008 to 15th December 2009 were reviewed in order to identify patients whose indication for their scan was suspected Sarcoidosis. These patients were then entered into this retrospective study and their case notes were reviewed independently by two investigators (AA and DK).
Those patients who had known Sarcoidosis (44 patients) or were scanned for reasons other than suspected Sarcoidosis (140 patients) were excluded. In some cases the indication was unclear so all patients for whom the indication might have been suspected Sarcoidosis (75 patients) were put forward to have their case notes reviewed. This process is summarised in Figure 2.

Figure 1. Panda (A) and Lambda (B) patterns on gallium scan.
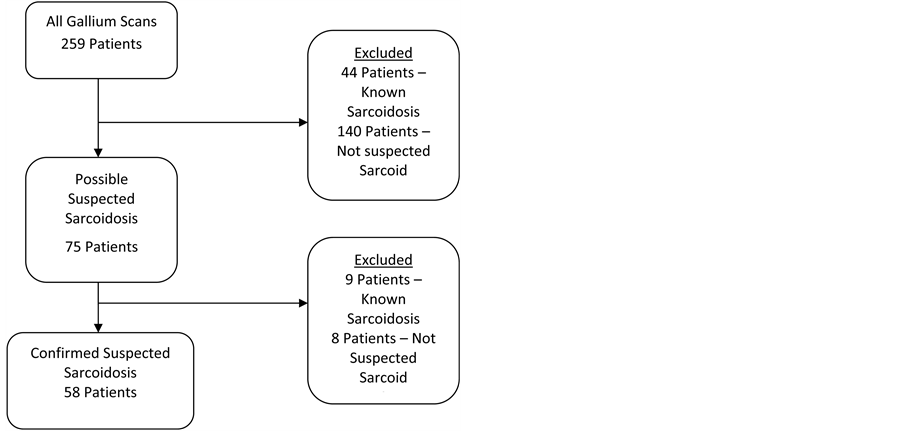
Figure 2. Flow chart of inclusion and exclusion criteria.
The following features were all specifically sought and noted; initial clinical presentation, indication for the scan, other investigations the patient had undergone prior to and after the scan, and the eventual diagnosis. 17 patients were subsequently withdrawn from the main body of the study because they were found either already to have biopsy confirmed Sarcoidosis (9 patients) or Sarcoidosis was not specifically suspected (8 patients). The patient’s diagnostic certainty for Sarcoidosis was then determined as being unlikely, possible, probable or definite according to the criteria described in Table1 Attention was then focussed on the patients that were determined to have a likely diagnosis of Sarcoidosis (the probable and definite diagnostic groups). For these patients a note was made as to whether there was systemic involvement and more specifically if there was neurological involvement. Special attention was paid as to whether potential biopsy sites were identified that had thus far been clinically silent.
The results of the investigations undertaken as part of the initial diagnostic workup were then analysed in the context of the proposed diagnostic category. The Ga-67 scan results were analysed for the combination of “panda” and “lambda” patterns. These patterns were further subdivided into “full” and “partial” patterns. Full patterns consist of bilateral lacrimal and parotid gland uptake (panda pattern) or bilateral hilar and right paratracheal uptake (lambda pattern). Partial patterns were defined as consisting of the presence of one aspect of the pattern only e.g. a part panda pattern would consist of either bilateral parotid uptake or bilateral lacrimal uptake (N.B. in the case of parotid, lacrimal and hilar uptake, the uptake must be bilateral to be counted as half a pattern). The patterns have been designated codes as follows: P—panda, L—lambda, pP—part panda, pL—part lambda. Whilst it is acknowledged that there are no accepted criteria for a valid diagnosis of Sarcoidosis using gallium scans, we used these criteria for the study.
The patients excluded from the study as they were scanned for reasons other than suspected Sarcoidosis (excluding those who were already known to have Sarcoidosis) were treated as a background population and their results of their Ga-67 scans were also analysed so that comparisons could be made with the study group.
3. Results
3.1. Patient Demographics
Of the 58 patients whose indication for their gallium scan was suspected Sarcoidosis 30 were female and 28 male. The age range was 17 - 75 years (M: 19 - 75 years; F: 17 - 73 years) and the average age was 45.1 years (M: 46.8 years; F: 43.6 years). The ethnicity where recorded of the patients is shown in Graph 1.
3.2. Clinical Syndromes
The 58 patients included in the study were subjected to the diagnostic criteria noted in table one and categorised

Table 1 . Criteria for diagnostic groups.
N.B. Definite, probable and possible groups are based on the premise that likely alternative diagnoses are excluded.
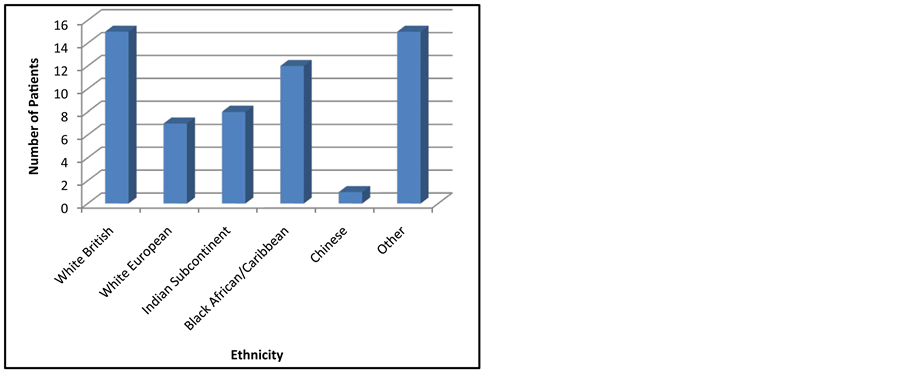
Graph 1. Ethnicity of the 58 patients included in the study.
as follows: unlikely—21; possible—12; probable—12; definite—13. Clinical sites of involvement in these 25 patients are summarised in Graph 2.
Asymptomatic patients were those who had no symptoms attributable to Sarcoidosis at the time of presentation. They underwent Ga-67 scanning as an anomaly consistent with Sarcoidosis had been found incidentally when the patient was undergoing tests for other reasons (e.g. a patient was found to have bilateral hilar lymphadenopathy on chest x-ray when he was admitted to A & E for acute coronary syndrome).
General systemic symptoms were considered to be those attributable to the disease process but not easily attributed to a specific locus in the body (e.g. fever, fatigue, night sweats and weight loss).
23/25 patients thought to have probable or definite Sarcoidosis had serum ACE levels measured as part of their diagnostic work up. 10 (43.5%) of these patients were found to have elevated serum ACE levels. 3/10 patients were noted to have markedly elevated levels of serum ACE. These patients all had systemic symptoms at presentation (with or without localised symptoms).
20 patients had a chest x-ray as part of the investigation of their initial presentation. 11 of these had x-rays that were interpreted to be abnormal; 8 of these patients (40%) had bilateral hilar lymphadenopathy (BHL), 1 patient had right hilar lymphadenopathy only, 1 patient had bronchial wall thickening only and 1 patient had nodular shadowing only. Of the 8 patients that were reported as having BHL, 1 patient was also reported as having lung nodules and 1 patient as having reticular shadowing.
22/25 patients underwent a thoracic CT scan. Only 2 had normal scans and these patients corresponded with 2 of the 9 patients who also had normal chest x-rays. Of the 20/22 patients who had some abnormality on their scans, 19 were found to have BHL; other relatively common features included parenchymal lung nodules (6/22), ground-glass shadowing (3/22) and atelectatic changes (2/22).
3.3. Ga-67 Scans
The method for analysing Ga-67 scintigraphy results has already been discussed and the patterns that were found in the 25 patients proposed to be likely to have Sarcoidosis are summarised in Graph 3.
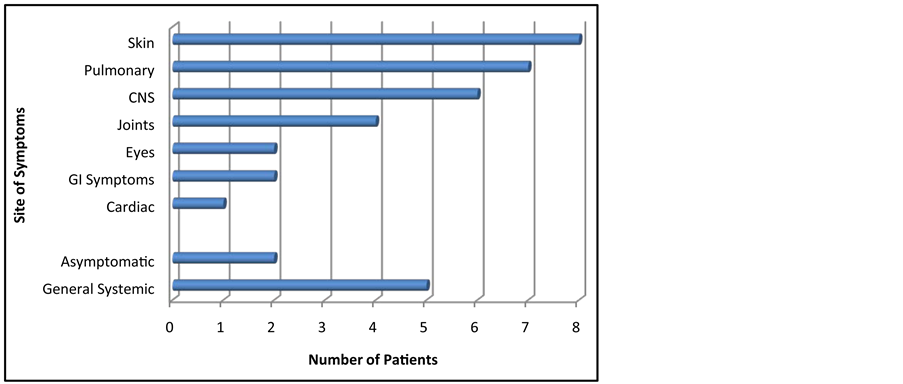
Graph 2. The systems involved in the presentation of the 25 patients thought likely to have Sarcoidosis (N.B. some patients had symptoms localising to more than one system or including systemic symptoms).
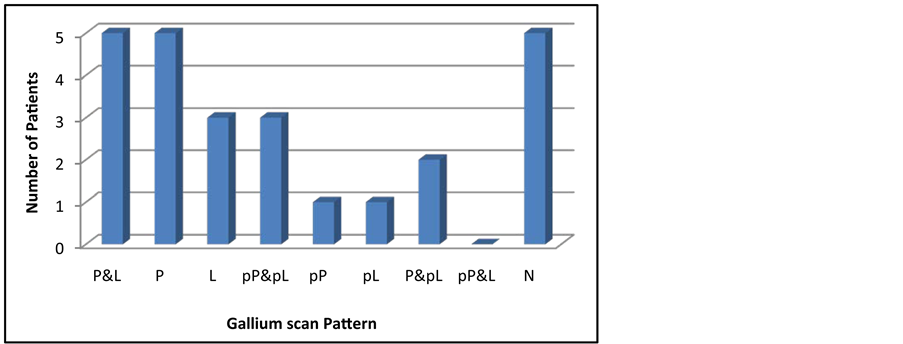
Graph 3. Ga-67 scan patterns for the probable and definite Sarcoidosis groups. P—panda; L—lambda; pP—part panda; pL—part lambda; N—normal.
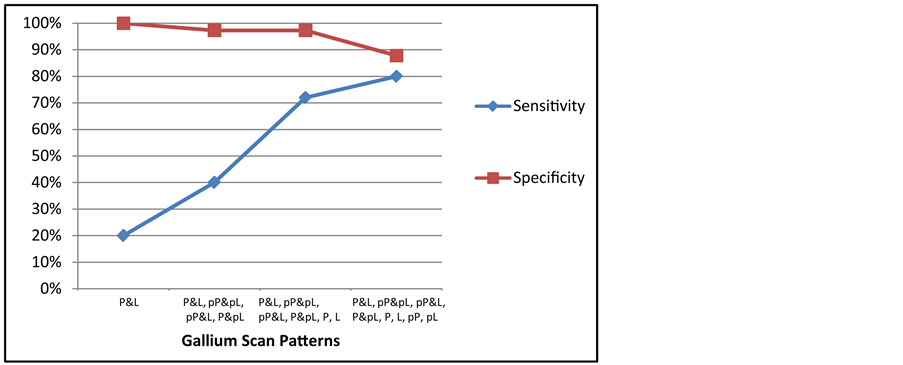
3.3.1. Sensitivity and Specificity
Of those patients thought likely to have Sarcoidosis (the probable and definite groups), 20% (5/25 patients) had both “panda” and “lambda” patterns on their gallium scintigraphy.
None of the 148 patients, who were excluded as the indication for their gallium scan was not suspected Sarcoidosis, showed full “panda” and “lambda” patterns. 11 showed a pP pattern, 3 pL, 2 pP & pL, and one each pP & L and P & pL. The remainder showed no abnormal uptake of Gallium.
If the threshold for a Ga-67 scan being positive for Sarcoidosis were raised from P & L to including pP & pL, pP & L and P & pL then a further 5 patients would be positive for Sarcoidosis by Ga-67 scan and the sensitivity would be raised to 40%. This increased sensitivity would, however, be at the expense of a decreased specificity as 4/148 would now be included—a false positive rate of 2.7%.
If the threshold were raised to include P, L, pP, pL, 20/25 patients thought likely to have Sarcoidosis would be positive for Sarcoidosis by gallium scan, raising the sensitivity to 80%. However 18/148 (12.2%) of the background population would now be included as being positive by gallium scan for the disease.
If P only and L only subgroups are included within the lowered threshold but not pP or pL (i.e. including P & L, pP & L, P & pL, pP & pL, P and L) then 18/25 (72%) likely Sarcoidosis patients are positive by gallium scan and 4/148 (2.7%) of the background population of patients test positive. Essentially, this means that by including the subgroups of patients who have full panda only or full lambda only patterns on their scan, the sensitivity of gallium scans for Sarcoidosis in this study increases with only a modest fall in specificity. These changes are summarised in Graph 4.
If these patterns (i.e. P & L, pP & L, P & pL, pP & pL, P, L) are considered to be positive for Sarcoidosis and are applied to the patients who were scanned for suspected Sarcoidosis but whose diagnostic certainty was determined as being unlikely or possible then 88% (29/33 patients) of the patients would have been gallium scan negative for Sarcoidosis. Of the 4 patients who would be considered to be positive, all 4 were part of the possible rather than unlikely group and the scans showed pP and pL in 3 cases and full panda pattern only in 1 case.
3.3.2. Role in Identification of Potential Biopsy Sites
Of the 25 patients in the probable and definite Sarcoidosis groups, 20 patients had sites identified on their gallium scans as having increased uptake in keeping with granulomatous inflammation in areas of the body that had so far been clinically silent. These sites could represent potential sites for biopsy that would not have been identified on clinical grounds alone.
17 out of these 20 patients showed increased activity that was not associated with identifiable abnormalities on their chest x-ray (or in the 4 cases that did not have a chest x-ray, would not have been identifiable even if they had one done as the sites were extra-thoracic).
16/20 patients showed increased activity that was not associated with abnormalities identified on their CT scans of the thorax (or in the 2 cases that did not have a CT scan, would not have been likely to have been identified had they had one as the sites were distant from those associated with their clinical symptoms).
The potential biopsy site most frequently identified on Ga-67 scanning that had not been identified by alternative methods of imaging was the parotid gland. The other sites are summarised in Graph 5.
 (a)
(a) 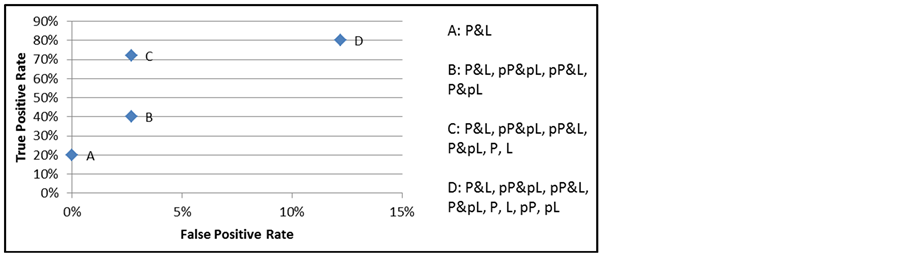 (b)
(b)
Graph 4. (a) Changes in sensitivity and specificity of Ga-67 scans for detecting Sarcoidosis with lowering the threshold for a “positive scan” by including incomplete combinations of panda and lambda patterns; (b) The same data represented as a receiver operating characteristic (ROC) curve.
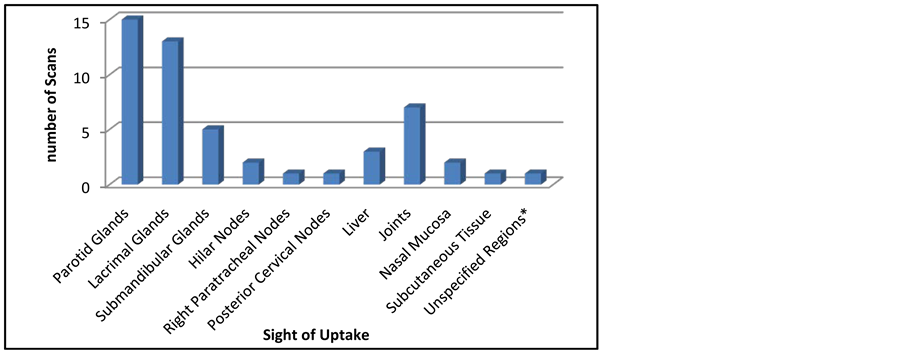
Graph 5. Sights of increased uptake in Ga-67 scans of probable and definite Sarcoidosis patients that were not identified by other methods of imaging.
*One report highlighted uptake in “axillary, femoral and inguinal regions”.
3.4. CNS Sarcoidosis
6 patients in this study were thought to have probable (3 patients) or definite (3 patients) Sarcoidosis affecting the central nervous system. 4 of the patients presented with neurological signs alone, of whom 3 showed abnormalities in keeping with Neurosarcoidosis on brain MRI. Of the 2 patients who presented with systemic and neurological symptoms, both had cutaneous involvement and one also had joint involvement.
Ga-67 scans of these 2 patients showed both panda and lambda patterns. In one case of seemingly isolated Neurosarcoidosis a panda pattern was seen. The remaining 3 were normal. Potential biopsy sites identified by gallium scanning that were not identified by other methods of imaging involved an increased uptake in parotid and lacrimal glands in all 3 abnormal scans. 1 scan also showed increased uptake in the submandibular glands, hilar nodes and right paratracheal nodes, 1 scan showed increased uptake in the liver and 1 scan showed increased uptake in the axillary, femoral and inguinal regions.
2/6 patients had raised levels of serum ACE. Chest x-ray was normal in 3 cases, not done in two cases and bronchial wall thickening was the only abnormality in the remaining patient’s case. CT scans revealed BHL in 4 cases and were not done in two cases. Other abnormalities in addition to the BHL were lung nodules in one patient and ground-glass shadowing and atelectic changes in another.
4. Discussion
4.1. Ga-67 Scintigraphy in the Diagnosis of Sarcoidosis
Ga-67 uptake represents areas of inflammation in Sarcoidosis and has the potential to play an important role in achieving a correct diagnosis of the disease and assessing how widespread the condition is. How great a role this is will dependent on the sensitivity and specificity of the criteria for interpreting the scans. It has been recommended that the diagnosis of Sarcoidosis should only be made with certainty when the presence of “panda” and to a lesser degree “lambda” patterns are seen. The point has been made, however, that whilst highly specific for the disease, requiring the presence of both these patterns makes gallium scintigraphy a relatively insensitive method for diagnosing Sarcoidosis. These statistics are supported by our findings in this study in which 20% of patients with probable or definite Sarcoidosis had full “panda” and “lambda “patterns and none of the background population had full “panda” and “lambda “patterns.
4.2. Patterns of Ga-67 Uptake Associated with Sarcoidosis
This study has shown that by altering the diagnostic criteria in Sarcoidosis Ga-67 scintigraphy may be more than 3.5 times more sensitive for detecting Sarcoidosis than was previously thought, with only a relatively small compromise in sensitivity. Our results suggest that accepting less complete combinations of “panda” and “lambda” patterns (i.e. pP & L, P & pL, pP & pL, P, L) as being more specific for Sarcoidosis than previously thought may increase the value of Ga-67 scintigraphy as a diagnostic tool in the context of suspected Sarcoidosis.
Accepting these incomplete pattern combinations as having greater diagnostic value for Sarcoidosis appears favourable when analysing their occurrence in patients who are thought to have the disease compared with the background population. However, it is worth noting that this study has found the apparent false positive rate to rise to 2.7% in patients with clinically suspected Sarcoidosis who have subsequently been determined to be unlikely to have the disease. That said, the diagnostic certainty for these patients having Sarcoidosis was deemed to be “possible”, despite their negative criteria by the standards set out at the beginning of this study. It is possible that these patients actually represent cases of Sarcoidosis that have been missed by the investigations performed to date. Indeed, they may represent patients with Sarcoidosis who would stand a greater chance of early diagnosis due to the emphasis placed on the link between incomplete “panda” and “lambda “patterns and Sarcoidosis suggested by this study.
Larger scale studies are required to confirm the value of incomplete combinations of “panda” and “lambda” patterns in diagnosing Sarcoidosis.
4.3. Ga-67 Scintigraphy in Neurosarcoidosis
It would be ideal if Ga-67 scanning could identify areas of active inflammation outside the CNS that would be amenable to biopsy in patients presenting solely with neurological symptoms. Our results on a limited number of patients with Sarcoidosis affecting the CNS show that although half of these patients had abnormal gallium scans providing alternative biopsy sites (largely lacrimal and parotid glands), only one of these had no identifying systemic involvement at the time of investigation. This is important as very few patients would have these sites identified by other forms of imaging. The results do not support previous observations that there is a role for Ga-67 scintigraphy in the evaluation of patients with Neurosarcoidosis when there is no evidence on clinical grounds for systemic involvement of identifying areas of sub-clinical disease that may provide a less hazardous site to biopsy. If a patient with systemic Sarcoidosis develops neurological involvement in keeping with neurosarcoidosis the diagnosis may be straightforward, but if a patient has isolated inflammatory disorder in keeping with Neurosarcoidosis but without evidence for systemic features, it is unlikely that Gallium scanning will provide an answer.
4.4. New Methods
Whilst Ga-67 scintigraphy appears to still be an adjunctive tool which has great accuracy and utility in Sarcoidosis and, though first described 40 years ago, there are disadvantages. The dosimetry of Ga-67 is not ideal and the fact that imaging is required over 48 hours means that this test does not fit in well with the modern rapid results regimes that now exist in modern health care.
F-18 FDG PET is quickly emerging as a new method with possibly greater sensitivity to Gallium especially where there is nodal, cardiac or CNS involvement [9] -[11] . The test can be completed with 3 hours of injection and radiation dose is half that of Ga-67. Inter observer agreement for positivity was greater with FDG PET than with Gallium in one study [12] .
NOTES
*Corresponding author.