1. Introduction
The Pneumocystis jiroveci pneumonia is an opportunistic infection in which the infectious agent is Pneumocystis jiroveci, eukaryote belonging to the family of fungi. This opportunistic infection often occurs in the context of congenital or acquired immunodeficiency [1] [2] . We report the case of Pneumocystis jiroveci pneumonia in an immunocompetent female patient.
2. Clinical Observation
We report the case of Mrs Z.J. aged of 30 years, treated for smear-positive pulmonary tuberculosis 6 months ago, admitted to the department of pneumology for acute respiratory failure. The symptoms have appeared a week before with a productive cough with purulent sputum and right chest pain and dyspnea.
Clinique examination objectified cyanosis of the lips and extremitis, blood pressure of 120/70 mmHg, a heart rate of 70 beats per minute, a temperature of 38˚C and SaO2 to 82% in air. The examination showed polypnea with 32 cycles per minute with crackles at the right chest and left aeric effusion syndrome.
The chest radiograph found reticulo-micro-nodular opacities on the right with lesions of emphysemaon the left (Figure 1).
Chest CT scan confirmed the presence of bullous emphysema with air-fluid level in left and nodular opacities with bronchiectasis in right (Figure 2).
NFS objectified leukocytosis of 14,430 per mm3 with neutrophil granulocytes of 11,080 per mm3 and lymphocytes to 2080 per mm3. CRP was at 140.7 mg/l. Serum electrolytes objectified mild hyponatremia at 130 mmol/L, the BNP level was normal and fasting bloud sugar was at 1.09 g/l.
The patient was put under amoxicillin clavulanic acid (3 g/day) and macrolide (500 mg/day for 3 days) and oxygen 6 L/min, without improvement.
A comprehensive assessment was performed including three sputum AFB smears and culture which are negative. The search for Pneumocystis jiroveci in induced sputum returned positive 2 times.
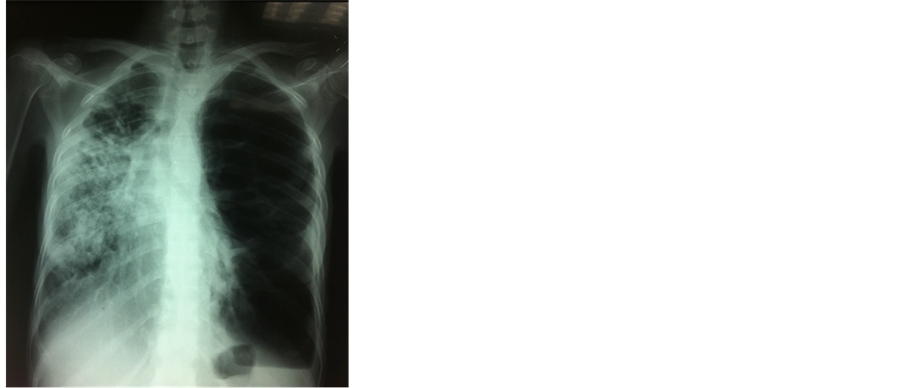
Figure 1. Chest radiograph showing reticulonodular opacities heterogeneous micro-interesting all the right hemithorax, with presence of air bubbles left with air-fluid level and distortion tracheobronchial.
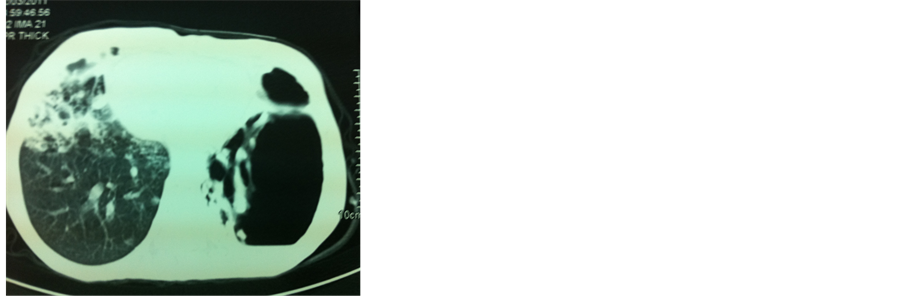
Figure 2. Chest CT objectifying bullous emphysema with total air-fluid level on the left, nodular opacities and dilated bronchi in the right.
The patient was put under trimethoprim sulfamethoxazole orally (4 tablets per day) for 3 weeks and oral corticosteroids with good clinical outcome. The search of an immunosuppression was performed. The rapid HIV test and HIV serology were negative. The rates of CD4 and CD8 were normal. They were respectively 1880/mm3 and 732/mm3. The serum total protein was 67 g/l. The serum protein electrophoresis and immunoeletrophoresis were normal.
The diagnosis of Pneumocystis carinii pneumonia in an immunocompetent patient was made.
3. Discussion
The Pneumocystis jiroveci pneumonia is generally an opportunistic infection. It is exceptional in the immunocompetent [3] . For many years, Pneumocystis jiroveci pneumonia was considered as a result of reactivation of latent infection acquired in childhood [4] [5] . However, several factors have shown that reactivation of chronic infection is probably not the only cause and probably also a result of environmental exposure or interpersonal contamination. Moreover, the acquisition of Pneumocystis jiroveci is sometimes linked to airborne transmission from asymptomatic carrier or patients with Pneumocystis carinii pneumonia [4] . The Pneumocystis jiroveci pneumonia in patients without predisposing factors, like that described in the immune deficits other than AIDS [6] [7] . The main reported symptoms are hyperthermia in 60% - 90% of cases, dyspnea in 75% - 90% of cases and cough in 50% - 80% of cases. The time between onset of symptoms and diagnosis is relatively short, ranging from 1 to 14 days. Clinical examination reveals tachypnea and diffuse crackles at pulmonary auscultation. PaO2 in ambient air is generally very decreased between 50 and 70 mm Hg. The Pneumocystis jiroveci pneumonia is more acute and severe in patients without HIV, with an array of acute respiratory failure often require the use of mechanical ventilation [4] , which is consistent with the case of our patient. But evolution can be more insidious with a frustrated and slowly progressive symptoms, as reported in HIV infection [4] [8] .
The x-ray findings of Pneumocystis jiroveci pneumonia are similar in HIV positive and negative patients. Typically, pulmonary involvement is often bilateral [4] . The X ray chest shows bilateral and diffuse interstitial opacities at the hilum. The radiography may be normal at a very early stage [3] . Classical elementary lesion objectified by CT scan is diffuse ground glass appearance whose distribution is heterogeneous sparing the cortex. Less obvious lesions as nodular opacities or cavity may be present. These atypical lesions may reflect a granulomatous reaction, but should evoke a cancer or other concomitant infection. This was the case in our patient.
Unlike HIV patients, cystic lesions are not described in HIV-negative patients with Pneumocystis carinii pneumonia [4] .
The diagnosis requires the detection of Pneumocystis carinii by appropriate coloring on respiratory samples (Gomori-Grocott, Giemsa, toluidine blue, specific immunofluorescence) [9] , or molecular biology with the identification of Pneumocystis jiroveci DNA by polymerase chain reaction [6] .
These samples are often obtained by bronchoalveolar lavage wich this is the reference method [9] . In specialized department, induced sputum by inhalation of hypertonic saline may be substituted bronchoalveolar lavage on first intention. This simple and noninvasive examination requires great rigor [9] .
The first-line treatment of PCP is trimethoprim-sulfamethoxazole (TMP-SMZ) administered orally or intravenously to the respective doses of 15 to 20 mg/kg/d (TMP) and 75 to 100 mg/kg/day (SMZ), a total of 21 days [9] . When it cannot be used or has to be interrupted due to significant side effects, Pentamidine isethionate is an alternative [10] . Oxygen therapy should be adapted to hypoxemia and corticosteroids are indicated in pneumonia with moderate to severe hypoxia (PaO2 less than 70 mmHg). Corticosteroids have more interest in pneumocystoses unrelated to HIV. That said, the risk of an associated latent viral infection is important [6] . The prognosis of this affection remains conditioned by the severity of lung damage and early effective treatment.
4. Conclusion
Through this observation, we insist on the importance of searching for Pneumocystis jiroveci in patients with febrile pneumonia with hypoxia, even in an immunocompetent patient.