A Functional Scoring System to Assess the Level of Impairment in Patients with Low Vision Impairment ()
1. Introduction
Visual impairment (VI) is an acute reduction in the visual acuity that cannot be rectified with medication, surgical operation, spectacles or contact lenses [1] [2] . VI is usually associated with major eye blinding diseases such as cataracts, diabetic retinopathy, glaucoma, and age-related macular degeneration (AMD) that crop up steadily deprived of warning signs [2] . Among these diseases, cataract is the primary cause of VI worldwide followed by glaucoma, AMD, diabetic retinopathy and trachoma [3] . According to the World Health Organization (WHO), globally there are 135 million people with low vision, 45 million are blind and this number is expected to reach up to 76 million by 2020 [4] . In India, it is estimated that the prevalence of blindness is about 1.1% in the major states and 1.38% in the north-eastern states [5] .
An individual experiences blindness and VI due to different causes as cataracts, glaucoma, macular degeneration and retinitis pigmentosa [6] . Numerous others have uncorrected refractive errors that might be improved without difficulty with glasses or contact lenses [7] [8] [9] . It is estimated that up to 5% of people with VI are totally blind [6] . VI is an incurable disease [10] but screening for disorders might help an individual in improving the quality of life or slow down progression of vision loss [11] .
There are two categories of VI in younger children: ocular visual impairment (OVI) and cortical visual impairment (CVI) [11] . In OVI, the eye building tissues are underdeveloped or get damaged due to an insult or infection that causes unclear or incomplete vision. While in CVI, the organization of tissues is healthy but the brain gets impaired due to damage to the visual centers of the brain [12] . However, ocular disorders are among the prominent cause of VI in young children [11] [13] .
There are various estimation practices and measures used to evaluate patients with VI. Visual acuity is the best variable that categorizes vision loss and is an established measure for describing VI by the WHO [14] . Snellen chart is the most common tool for assessing visual acuity [4] . Though readily available, easy to perform and universally accepted, Snellen chart has some disadvantages. The most significant difficulty faced with the design of the Snellen chart is uneven progression, variable letter size, no equal legibility and possesses greater crowding phenomenon [7] [15] [16] . Moreover, the diagnostic accurateness of Snellen chart is problematic because a clinically appropriate reference standard is not established [17] . Further, we cannot statistically assess parametric analysis with this decimal progression sequence, even if converted to another form. It fails to evaluate visual acuity statistically at the right distance and under suggested points of illumination [16] .
There are scoring systems for numerous other medical disorders such as cerebral palsy [8] , spinal cord injury [18] and multiple sclerosis [19] . Nonetheless, there is no such separate system to evaluate the patients with VI. We developed a numeric method, Nutech Functional Score (NFS), to measure the ailment of patients with VI based on observations and clinical symptoms. NFS for vision disorder is a 33-point positional and directional scoring system that can be used to assess or validate the diagnosis of low vision or VI.
2. Methodology
We have been treating patients with various eye diseases such as glaucoma, CVI, AMD, since 2000. Cases associated with ocular diseases admitted at our facility visited directly or were referred by other hospitals/institutions. These patients were previously diagnosed. We assess the event equally for common and rare symptoms, and record them in the diagnostic history. These patients provided written informed consent. An independent Institutional Ethics Committee (IEC) of Nutech Mediworld approved the current study. The study was conducted in compliance with the “Declaration of Helsinki” and good clinical practices (GCP).
Thus, over the years, a list of symptoms was prepared which contained all the possible symptoms and was used to diagnose patients with vision disorders. This list of symptoms is revised from time to time to maintain accuracy. Each symptom is evaluated on basis of five ordinal grades running in BAD → GOOD direction. The grades have been converted into numeric values for conducting probability based analysis. We used NFS scoring system for vision disorders to assess patients with low vision or VI who were previously assessed by the ophthalmology department or specialized clinics.
3. Results
The institute developed a 33-point positional (each symptom is sub-graded with a distinct score) and directional (bad to good) scoring system that authenticates the patients with VI. It measures the disorders through symptoms, namely, NFS grades which are grouped to determine the symptoms. These symptoms include anterior chamber depth (deep), anterior chamber depth (shallow), blurring of vision, burning sensation of eye, color blindness, double vision, fatigue (eye), floaters (colored halo), foreign body sensation etc. NFS scores for all the symptoms are presented in Appendix 1. If a patient is not associated with the symptom, then it is graded as not affected in affliction (NAA). These five ordinal scores (1, 2, 3, 4, 5) run in the direction of 1 → 5 i.e. BAD → GOOD. These five grades from 1 → 5 signify worst, bad, not so bad, good and normal, correspondingly. These five grades that lie in a range of (0.5, 5.5) are equidistant to each other and are continuous. The scores have been converted into numeric values to facilitate the conduct of probability based studies which require a range of (−1, 1) or (0, 1). This configuration can be used collectively for one symptom. The polynomial smoothing and graphical methods have been used to derive an equation for converting categorical scores into numeric scores. The equation is as follows:
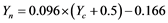
where,  = numeric score and
= numeric score and  = categorical score.
= categorical score.
Table 1 shows how five/three categorical grades (0.5 - 5.5) for symptoms can be converted to five/three numeric grades in the range (0, 1).
4. Discussion
Nutech Mediworld established NFS for vision to evaluate the ailment of patients with VI on the basis of observations and clinical indications. NFS designates its usefulness by detecting even the minor improvement in terms of grades associ-
![]()
Table 1. Conversion table from categorical grades to numeric range for NFS.
ated with symptoms and after clinical investigation. Various other scoring systems are also used for evaluating VI like rasch analysis. Like rasch analysis, NFS also places the items and the patients along a single ratio scale, the units being logits. For ease of interpretation and consistent with the idea, the higher scores represent better functioning.
Huo and colleagues in their study established a six level measure of functional vision. These six levels used were on the basis of symptoms such as light perception only, occasional fixation on large objects, faces or movement, occasional fixation on small objects (i.e., pennies or stickers) or reliable fixation on faces etc. They used this system as a method of enumerating functional vision and calculated the grades in terms of variations in the levels. But this system fails to explain how the patient really used vision in activities of average life and do not provide any information about the reliability or validity of the scale [20] .
Dutton in 2004 established an assessment tool for the children suffering from cortical visual impairment (CVI). The goal of this tool was to determine the vision accessible for communication, education, and movement in the environment. The recommended observations were on the basis of characteristic vision skills (acuity, contrast sensitivity, visual fields) and visual processing skills (simultaneous visual processing problems, recognition, problems with reading, problems with orientation, visual memory etc.). However, this assessment tool does not provide any directions for precise observations or direct valuation of these skills. Besides this, the assessment system is also not able to provide information for the use of findings from observations for educational interventions [9] .
NFS scoring system appears to be a simple and suitable method to confirm the diagnosis of patients with low vision based upon symptoms. This assessment system runs in 1 - 5 direction, i.e., BAD → GOOD which signifies worst, bad, not so bad, good and normal, respectively. This system has procured nearly all the possible symptoms that are connected with VI. NFS is a numeric system that has been authenticated statistically and can benefit in evaluating patients with low vision due to refractive errors or either due to diseases.
Let’s take an example to describe how NFS is used to grade a patient with low vision. We assume a female patient aged 21 years with low vision is graded with NFS.
Similarly, we have graded all the other symptoms included in NFS for this patient (Table 2). The total NFS score is calculated by counting the grades of the
![]()
Table 2. A hypothetical example showing NFS grades of a patient before and after therapy.
all symptoms. In this case, the patient scored 17 for both the eyes. Let’s suppose that this patient undergoes therapy for low vision. After the therapy, we found that the total NFS score for symptoms increased as the patient moved from grades 1 → 5 in BAD → GOOD direction showing improvement. The grades after the therapy were calculated as 41 for the right and 34 for the left eye. The NFS scoring system is numeric which means grades can be added by means of improvement either in “number of symptoms” or “all” and it can be subtracted if the patient symptoms “further deteriorated” or that “disease affects some other part of the body”. The other advantage is that the evaluation system is suitable for the patients of all ages with diminished complexities that would rise during evaluation process. Therefore, the information obtained with NFS is reliable, much more precise and reveals sustainable improvement in patients suffering from low vision.
5. Conclusion
Summarizing, there is a lack of discrete scoring system for patients with VI. The eye test and other ocular tests have low specificity and sensitivity. A numeric scoring system like NFS can be a useful tool that may help doctors globally to authenticate the diagnosis of low vision in patient.
Acknowledgements
The author acknowledges all the doctors, staff and patients of the Nutech Mediworld. The author also acknowledges Knowledge Isotopes Pvt. Ltd. (http://www.knowledgeisotopes.com) for the medical writing support.
Funding Sources
No funding sources were used to sponsor this study.
Disclosures and Ethics
The authors declare no conflict of interest associated with the publication of this manuscript.
Supplementary Data
Appendix 1. Nutech Functional Score for Vision Impairment.

Submit or recommend next manuscript to SCIRP and we will provide best service for you:
Accepting pre-submission inquiries through Email, Facebook, LinkedIn, Twitter, etc.
A wide selection of journals (inclusive of 9 subjects, more than 200 journals)
Providing 24-hour high-quality service
User-friendly online submission system
Fair and swift peer-review system
Efficient typesetting and proofreading procedure
Display of the result of downloads and visits, as well as the number of cited articles
Maximum dissemination of your research work
Submit your manuscript at: http://papersubmission.scirp.org/
Or contact ojoph@scirp.org