1. Introduction
Tooth discoloration is a possible side effect of endodontic treatment of anterior teeth [1] . Hemorrhage inside the pulp cavity, residual pulpal tissue as well as materials used during root canal treatment are the most usual causes for discoloration [2] . In addition obturating materials, intracanal medicaments and temporary filling materials may cause also of internal tooth staining [1] -[3] . As far as the intracanal medicaments concerns, their role in the success of the endodontic treatment is important, since they maintain the root canals disinfected for the time interval between instrumentation and final root canal obturation [4] .
Calcium hydroxide (Ca(OH)2) plays an important role in endodontics due to its ability to induce hard tissue formation, its antibacterial effect and its ability to act as a physical barrier to prevent root canal reinfection [4] [5] . These properties derive from its high pH (up to 12.5), which neutralises lactic acid from the osteoclasts, thus preventing a dissolution of the mineral components of dentin. Moreover, it could also activate alkaline phosphatases which play an important role in hard tissue formation [5] [6] . However, due to the existence of Ca(OH)2- resistant micro-organisms (especially E. faecalis), many antimicrobial agents have been proposed for use, in combination with Ca(OH)2 [4] [5] [7] .
One of the most important antimicrobial agents in dentistry is chlorexidine (CHX). The most significant properties that justify the use of CHX as an intracanal medicament are its antimicrobial activity against Grampositive and Gram-negative microorganisms, as well as its residual antimicrobial ability on the dentin surface after remaining for at least one week within the root canal (substantivity) [4] [8] . Moreover, CHX is effective against bacteria that are resistant to Ca(OH)2 and mainly E. faecalis; this property justifies the use of CHX in retreatments, where such bacteria are usually found [9] . However, clinical studies have recorded tooth staining by CHX, especially when it is used as a mouthrinse for periodontal treatment [8] [10] . The most possible staining mechanisms of tooth discolorations due to CHX application seem to be non-enzymatic browning (Maillard reactions) and formation of pigmented black metal sulfides [10] . Nevertheless, the corresponding phenomenon has not been investigated in cases when CHX is used for endodontic purposes. On the contrary, the staining potential of Ca(OH)2 has not been clearly defined, as its discoloration ability may depend on its chemical composition (pure Ca(OH)2 powder, or commercial Ca(OH)2 pastes whose some contents may be able to discolor teeth). Nevertheless, some latest studies have concluded that Ca(OH)2 has indeed a discoloration potential, which might not have been extensively taken into account up to date [1] -[3] . The exact staining mechanism of Ca(OH)2 is not clearly known; it has been implied that it is more likely due to any additional components, i.e. bismuth carbonate, that usually exist in many commercially-prepared Ca(OH)2 pastes [3] , while as regards pure Ca(OH)2 powder, there has not been a convincing explanation.
The aim of this study was an ex vivo assessment of the discoloration potential of two different intracanal medicaments: (A) Ca(OH)2, (B) Ca(OH)2 combined with aquatic solution of CHX, both evaluated over a 3-month period. The hypothesis tested was that Ca(OH)2 and the combination of Ca(OH)2 with CHX as single intracanal medicaments did not present differences neither between nor in relation to the absence of any medicament as regards tooth color changes induced within 3-month post-treatment.
2. Materials and Methods
Thirty one intact human anterior mature teeth extracted for periodontal reasons were initially stored in 10% formalin. The teeth were free of caries, restorations and coronal staining. The teeth were cleaned with ultrasonics to disclose gross debris, followed by brushing with a rubber cup and pumice in order to remove remaining debris and stains from the coronal crown surface. Thereafter, the teeth were kept in distilled water until use.
To monitor the color changes of the teeth the method described by Koursoumis et al. was used [11] . Briefly, on a black rectangular piece of adhesive tape, a round opening of 4 mm in diameter was cut so as to match the size of the window of the colorimeter apparatus. The black tape was applied on the facial aspect of the crown in such a way that the round opening was positioned on the cervical third of the crown (Figure 1).
After the preparation of an access cavity of each tooth, the canal was negotiated with a stainless steel size #10 K-file (Dentsply Maillefer, Baillaigues, Switzerland) and the working length was determined by subtracting 1mm of the file length when the tip was visible on the apical foramen. Then, a glide path was confirmed using stainless steel size #15 and #20 K-files (Dentsply Maillefer, Baillaigues, Switzerland) in conjunction with copious amounts of irrigation. 2.5% NaOCl was used as irrigant in all teeth. Canal shaping was performed with a WaveOne large Ni-Ti rotary instrument (Tulsa Dentsply, Tulsa, OK, USA) used in a reciprocating movement
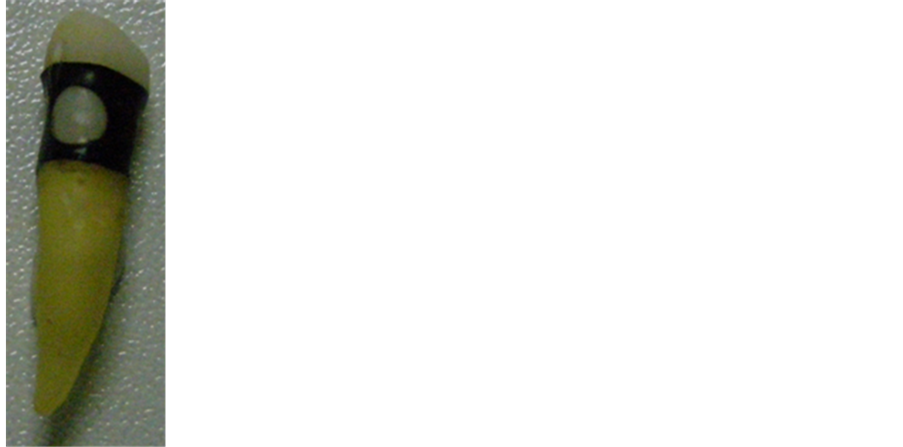
Figure 1. One of the specimens with its black rectangular piece of adhesive tape and the round opening on it to match the size of the colorimeter aparatus; the black tape was applied on the facial aspect of the crown in such a way that the round opening was positioned on the cervical third of the crown.
under copious irrigation. The large WaveOne instrument has similar conicity with the F2 ProTaper instrument. All instruments were used in conjunction with a 16:1 reduction ratio contra-angle connected to an ATR Vision (ATR, Pistoia, Italy) motor which allows the reciprocating movement. The clockwise and the counter-clockwise rotations are set on the motor at four-tenth and two-tenth of a circle. The rotational speed was set at 400 rpm.
After cleaning and shaping, one tooth was irrigated with 2.5% NaOCl, dried with air and paper points and its pulp chamber was sealed with a sterile cotton pellet, without any intracanal medicament (pilot tooth). The rest thirty teeth were randomly divided into two groups (n = 15), each according to the intracanal medicament used; (A) Ca(OH)2 paste (UltraCal™ XS™ Ultradent Products, Inc. USA), (B) 2% chlorhexidine aquatic solution combined with pure Ca(OH)2 powder. In group A, after copious irrigations with NaOCl, the pulp chamber and the root canals were slightly dried with air and the excess of the irrigant was removed with paper points, followed by the placement of the Ca(OH)2 paste and the removal of any excess of the medicaments in the access cavity. In group B, after copious irrigations with chlorexidine, the pulp chamber and the root canals were slightly dried with air and the excess of the irrigant was removed with paper points. After that, the combination of Ca(OH)2 with CHX was placed as follows: the CHX aquatic solution was prepared by a chemist by mixing chemically pure CHX with distilled water. Then, pure Ca(OH)2 powder was mixed with a few drops of the solution—with the exactly same way as Ca(OH)2 powder is mixed with saline—resulting in a thick mixture and applied to the root canals with a Lentulo spiral. Any excess of the medicaments were removed from the pulp chamber with a small cotton pellet and distilled water; afterwards, a sterile cotton pellet was enclosed in the pulp chamber in order to seal the access opening. All thirty one specimens were stored individually in a moist environment with 100% humidity in plastic airtight pouches, at a constant temperature of 37˚C. This methodology was studied thoroughly by other authors in the past [11] [12] .
Τhe color of the exposed enamel window through the tape hole was evaluated by a colorimeter apparatus (Microcolor, Data Station, DrLange, Braiveinstuments, Liege, Belgium) according to CIE Lab system (CIE L*, a*, b*) employing a repeated measurements design (n = 3). In order to establish an accurate positioning system for consistent assessments during color measurements, the specimens were mounted on silicon templates. Tooth color was measured before the application of medicaments (reference color), immediately after their application (baseline), and 1 week, 1 month, 2 months and 3 months post-treatment. The ΔL*, Δa* and Δb* values were calculated by subtracting the reference value from the values of each time post-treatment. The ΔΕ values, which were used to measure the color changes, were calculated by the equation ΔΕ = [ΔL*2 + Δa*2 + Δb*2]1/2 (Bureau Central de la Commision Internationale de l’Eclairage, 1978). According to the CIE system, L* contributes to the black-to-white hue of the tooth, a* contributes to the red-to-green hue, b* to the yellow-to-blue hue, while ΔE determines whether there is an overall color alteration [13] .
The ΔE values at the four post-treatment times were statistically analyzed by two-way ANOVA repeated test with endodontic intracanal medicament and post-treatment time as discriminating variables, following by Scheffé test (p < 0.05). Two-way ANOVA repeated test was also applied to identify the changes in L*, a*, b* by means of post-treatment time followed by Scheffé test (p < 0.05). Statistical analysis was performed using SPSS Statistics 17.0 software (SPSS, Inc., Chicago, IL, USA).
3. Results
Table 1 depicts the ΔΕ values measured for the two medicaments (Ca(OH)2, Ca(OH)2-CHX) as well as the pilot tooth, at the four post-treatment times. Table 2 presents the L*, a* and b* values for the two medicaments and the pilot tooth, both at the four post-treatment times and the reference color before the application of the medicaments. A gradual reduction of the mean ΔΕ values was recorded after the 1st week. Furthermore, ΔΕ values at the end of the observation period were above 3.3 for both groups, hence there was a color alteration probably perceivable even by a patient, as described above; on the contrary, the ΔΕ values of the pilot tooth remained below 3.3 throughout the 3-month observation period.
Statistical analysis of ΔΕ values showed that only time intervals have a significant effect on the ΔΕ values; the type of medicament did not have a statistically significant effect on the color changes recorded (Table 3). Thus, Scheffé test was applied only to figure out any statistically significant differences in the ΔΕ, L*, a* and b* values. Indeed, significant changes of ΔΕ values were recorded after the 1st week and after the 3rd month (Table 4). Statistical analysis of L*, a*, b* values showed that time intervals were again the only significant factor and interestingly, they affected only L* and a* parameters (Table 3). L* showed a significant change in the first week, while a* showed a significant change in the 2nd and 3rd month, both compared to the reference color (Table 4).
4. Discussion
According to the results of the present study, no significant difference was noted between the two intracanal medicaments as concerns color alterations. However, both medicaments provided a significant color change compared to the pilot tooth in which no medicament was applied.
It is a common knowledge that many intracanal medicaments may result in tooth discoloration, but as regards Ca(OH)2, its possible impact on color alterations remains unclear [1] -[3] . Some in vitro studies showed that

Table 1 . ΔE values of the two endodontic medicaments (Ca(OH)2, Ca(OH)2-CHX) at the four post-treatment times. The ΔΕ values of the pilot tooth are also depicted.

Table 2. L*, a* & b* values of the two endodontic medicaments and the pilot tooth at the four post-treatment times.

Table 3. Results of the two-way ANOVA analysis with reference to the statistical significance (if any) of the ΔΕ, L*, a*, and b* values amongst the two groups with the respective intracanal medicament and the pilot tooth. The first row compares the effect of the medicament, the second one the effect of time at the four-times period and the third one the combined effect of medicament and time. Statistically significant differences are marked in bold.

Table 4. Results of the Scheffé test analysis with reference to the statistical significance (if any) of the ΔΕ, L*, a*, and b* values amongst the two groups with the respective intracanal medicament according to the four post-treatment times (each value is compared at each time point to the reference color). Statistically significant differences are marked in bold.
Ca(OH)2 has a truly discolorating potential, which is more apparent in cases of immature rather than mature teeth [14] [15] . According to these studies the immature teeth had been extracted for orthodontic reasons and all mature teeth for periodontal reasons, and all teeth used were anterior, free of cracks, caries, restorations or cervical abrasions, thus it is more likely that color alterations are due exclusively to the effect of the medicaments used. These studies bear some resemblance to the present one. First, the specimens were measured with a spectrophotometer, with each measurement being expressed in the CIE L*a*b* system (as in the present study). Second, their time intervals were similar to the present study (before and after placing the medicaments, and 1, 2, 4, 8 and 12 weeks after their placement). However, an important difference is that all teeth used in our study were mature. Day et al. (2011) recorded discoloration of replanted teeth after avulsion, which had been treated with Ca(OH)2 [16] . However, in contrast to the present study, the researchers did not mention whether the excess of the medicament in the access cavity was removed, which could have affected the crown color, while time intervals were also somewhat different (10, 60 and 90 days after placement) [16] . Furthermore, avulsed teeth probably show a degree of dentin dehydration which may enhance discoloration of such teeth; such a color alteration potential has also been reported in cases of crown fractures treated with fragment reattachment [17] . The influence of Ca(OH)2 on discoloration may be more severe in teeth with vital pulpal tissue, possibly because of the existence of erythrocytes which contribute to color changes after Ca(OH)2-induced haemolysis [18] , although hemorrhage inside the pulp cavity during endodontic treatment of teeth with vital pulp is by itself sufficient to cause haemolysis [2] . However, more investigation is required in order this view to be confirmed. On the contrary, Lehnerr et al. (2012) recorded no staining neither after the use of pure Ca(OH)2 nor Ca(OH)2 pastes (both observed for a 1-year period) [3] . In this in vitro study, two hundred and ten bovine incisors were used, with color alterations being measured with a spectrophotometer and with each measurement being expressed in the CIE L*a*b* system (as in the present study). Their conclusion might be more safely taken into account, due to the larger number of specimens used, as well as the existence of more time intervals (prior to the placement of the medicaments, immediately after the placement, after 1 week, after 1, 2, 3, 6 and 12 months post-treatment). These intervals were exactly the same with the present study, with the exception of the last two ones (6 and 12 months post-treatment). Last but not least, researchers used standardized bovine tooth pieces with a similar shape and thickness (compared to human teeth), in order their results to be comparable to those of studies with human teeth.
Chlorexidine (CHX) is a really useful antimicrobial agent both for endodontic and periodontic reasons [8] [19] . It is really effective against Ca(OH)2-resistent bacteria (especially E. faecalis) [7] [8] . The substantivity property of CHX can last up to 12 weeks, which makes it appropriate for irrigation prior to obturation or even as an irrigant and medicament (at the same time) during retreatments [20] -[22] . However, it is highly associated with tooth staining as a side effect [10] . This is more apparent when CHX is used for periodontal reasons, and even more when dental plaque is present on the surfaces of the teeth (compared to plaque-free surfaces) [10] . Addy & Roberts (1981) had proposed the application of alexidine instead of CHX to avoid discoloration but unfortunately they found that alexidine has a discoloring effect similar to CHX [19] .
In order to combine greater antimicrobial activity with less staining effect, some researchers suggested the combination of Ca(OH)2 with CHX [4] -[6] [8] [9] [22] -[24] , as this combination provides extensive antimicrobial effect, especially against E. faecalis [9] . This assumption is not widely accepted, as some researchers found that mixing CHX with Ca(OH)2 results in decreasing the effectiveness of CHX (while the properties of Ca(OH)2 remain unchanged) [4] -[6] [23] . However, these results are not without controversy, as all studies that have suggested a decreased antimicrobial effect of the combination chlorexidine-Ca(OH)2 have used chlorexidine gluconate; thus this assumption cannot be equally applied to aquatic solution of chlorexidine that it was used in the present study. This is why an aquatic solution of CHX (2%) was selected to be combined with Ca(OH)2 in this study. Furthermore, CHX cannot remain alone within the root canal in vivo for a prolonged period of time, as it does not act as a physical barrier to bacteria and it does not present radiopacity [9] ; thus, CHX cannot be applied as a sole intracanal medicament for such a long period of time as in the present study, and this is why the combination of Ca(OH)2 with CHX is more appropriate for long-standing use. Taken together, it seems that the combination of aquatic solution of CHX with Ca(OH)2 may indeed be a useful medicament in order to provide sufficient antimicrobial effect against E. faecalis, especially in retreatments [9] ; thus, it is equally important to consider whether such a medicament may induce tooth discoloration.
The methodology used in the present study could be considered satisfactory in terms of preservation of the specimens. It has been applied by other authors in the past, too [11] [12] who found that both in the pilot group of teeth and the specimens examined that had been stored in the suggested way, tooth color alterations during time were minimal and the color remained rather stable; a similar finding was also observed in the present study. This was the reason why a larger number of teeth with no medicament was not selected for control group.
The analysis of the CIE parameters (L*, a*, b* and ΔΕ) supplied the study with some interesting conclusions. Αs mentioned above, L* contributes to the black-to-white hue of the tooth, a* contributes to the red-to-green hue and b* to the yellow-to-blue hue [12] . L* showed a continuous increase between the four time intervals for both groups A and B, which means a higher lightness of the crown of the teeth, and statistical analysis proved that this finding is statistically significant. In group A, a* exhibited a general decrease overtime, while b* a general increase. However, these alterations did not turn out to be statistically significant for the entire post-treatmenttime. In group B, both a* and b* parameters remained at about the same levels at all four post-treatment times. The ΔΕ values showed a general decrease in both groups between time intervals, with the final ΔΕ values ranging between 1 and 3.3. Taking into account that ΔE values below 1 concern color alterations that are not perceivable by the human eye, values between 1 and 3.3 concern alterations visually perceptible by skilled operators, and values above 3.3 concern alterations that are regarded as clinically “not acceptable”, since they are probably perceivable by the patient, the values found in the present study are as clinically acceptable [13] . The fact that the type of medicament did not have a significant effect on color alteration might be explained by Lenherr et al. (2012), who showed, among others, that no significant difference was recorded between pure Ca(OH)2 powder and UltraCal XS, both of which were also used in the present study [3] . Nevertheless, this does not seem to be a complete explanation, as in the present study UltraCal XS was combined with CHX, but as regards CHX, an explicit answer is not found in the literature; hence, further investigation is required.
5. Conclusion
Ca(OH)2 (either combined with CHX or not) has a discoloration potential. There is no significant difference between Ca(OH)2 and Ca(OH)2 combined with CHX. Nevertheless, the period of time these medicaments remain in the root canal significantly affects their discoloration ability. Therefore, clinicians should always take esthetic considerations along with biological aspects into account before the selection of an intracanal medicament, and regard time as an important factor before the application of such medicaments.
Acknowledgements
The authors wish to thank the Department of Biomaterials of the School of Dentistry of the University of Athens for the support and the equipment provided in order the present study to be completed. They also deny any conflicts of interest related to this study.
NOTES
*Corresponding author.