Pythagorean Self-Awareness Serves Successfully as a New Cognitive Behavioral-Based Technique in Multiple Sclerosis Physical and Psychosocial Well-Being and Quality of Life ()
Received 16 February 2016; accepted 19 April 2016; published 22 April 2016

1. Introduction
Multiple sclerosis (MS) is a chronic autoimmune demyelinating disease of the central nervous system (CNS) affecting mainly young people during their 30s. The cardinal neurological manifestations of the disease are motor and sensory symptoms that contribute to the physical disability accumulated in relapses or progression over time ( Compston & Coles, 2002 ). Immuno-modulatory drugs are the mainstay of pharmaceutical therapy aiming at halting the disease course ( Compston & Coles, 2002 ). There is now apt evidence showing that cognitive function and psychosocial well-being are also affected in MS and are important counterparts of both the disease course and the patients’ quality of life ( Lovera & Konver, 2012 ; José, 2008 ). Although challenging, there are numerous published interventions that hold promise for the successful management of these aspects of MS.
With respect to cognitive function, 40% - 60% of MS patients show impairments in domains such as information processing speed, memory, language, executive functions and theory of mind (i.e., the ability to deduce others’ thoughts and emotions based on verbal and non-verbal cues) ( Lovera & Konver, 2012 ). Cognitive dysfunction has been attributed to the ongoing pathogenetic process of cortical and white matter demyelination and axonal degeneration, which interrupts strategic neural circuits that subserve cognition ( Shi et al., 2014 ). Thus, cognitive dysfunction is directly related to the pathogenetic processes of the disease. Fortunately, there are reports supporting the existence of compensational brain processes that alleviate cognitive dysfunction in MS. Functional magnetic resonance imaging (fMRI) studies show several brain regions (such as the default-mode- network, DMN), and the altered function of these regions denotes adequate cognitive reserve and compensation for the intellectual dysfunction ( Bonavita et al., 2011 ; Sumowski & Leavitt, 2013 ).
Cognitive rehabilitation is still in its infancy, but the results of studies in the field are quite promising. In a recent meta-analytic review of twenty studies (follow-up of several weeks to months) by Cochrane, cognitive training alone (computer-assisted or paper-pencil tasks with or without memory help such as keeping a diary) was found to improve memory span and working memory; however, more benefits with attention, immediate verbal memory and delayed memory were added when this was done in conjunction with neuropsychological rehabilitation methods (for example, those based on cognitive behavioral therapy and stress management) ( Rosti-Otajärvi & Hämäläinen, 2014 ). Neurorehabilitation in MS seems to be accompanied by brain activation changes, implying that neuroplasticity could be the major culprit ( Penner et al., 2007 ). Interestingly, these changes follow a U-shaped frequency, meaning that MS patients in neurorehabilitation with too little or too much cognitive dysfunction are less likely to benefit from the compensation ( Penner et al., 2007 ).
More than half of MS patients suffer from anxiety and/or depression as a result of the cumulative effect of chronic stress that MS causes ( José, 2008 ). Stress, in conjunction with maladaptive coping, can also lead to disease worsening, e.g., accrual of disability and more relapses ( Artemiadis et al., 2001 ). The unpredictability of the disease, the social stigma, the physical restrictions, and the side effects of the prescribed drugs are just a few of the stressors that these people face in their daily lives with MS. Moreover, maladaptive stress is also heralded by the adoption of an unhealthy lifestyle (e.g., smoking) with putative detrimental consequences both for the course of MS and for the overall health of the individual ( McEwen, 2008 ; Pugliatti et al., 2008 ).
Interventions that strengthen patients’ self-efficacy, promote a healthy lifestyle and reduce stress have shown benefits both for disease course and psychosocial adaptation to the disease. So far, there are numerous and diverse published interventions for MS patients, the full description of which is beyond the scope of this paper (for reviews see Simpson et al., 2014 ; Plow et al., 2011 ; Olsen, 2009 ). Overall, interventions that promote self-em- powerment and self-efficacy through cognitive behavioral-based methods and/or stress management improve lifestyle, psychosocial well-being and quality of life. Interestingly, stress management can also reduce the formation of new lesions as evidenced by MRI scanning ( Mohr et al., 2012 ).
It is thus obvious that MS requires a holistic therapeutic approach that takes into account drug therapy, cognitive function, lifestyle behaviors and psychosocial factors (i.e., stress, coping, anxiety, depression, and self- efficacy). Such multidisciplinary approaches are subject to limitations, including time, personnel needed, and cost.
Pythagoras bequeathed to the people of Hellenic origin and to the whole of mankind a timeless philosophy that was not only theoretical in its content but had a series of daily mental and physical exercises, a holistic approach, and a clear impact on the daily lives of trainees. Introspection and practice of memory were two of the strongest weapons in the efforts of self-knowledge and self-mastery.
Under these premises, we have been inspired to develop and introduce a multifaceted intervention based on the Pythagorean philosophy. Our main goal was to implement a technique named Pythagorean Self-Awareness Intervention (PSAI) that can easily be taught and, more importantly, can be practiced systematically by the patient on his/her own. To test the effectiveness of this new technique, we conducted the present pilot study. The primary endpoints of the study were healthy lifestyle, stress, anxiety, depression, coping, fatigue and cognitive function.
2. Material and Methods
This is a non-blinded, randomized, two-armed parallel group clinical trial with a follow-up of twelve weeks. No protocol change was made after study commencement.
The study was conducted at the outpatient neurological clinic of NIMTS hospital in Athens, Greece from January to July 2014. The study protocol was approved by the hospital’s Scientific and Ethics Committee and was consistent with the Declaration of Helsinki. All eligible participants gave their written informed consent before study entry. All patients had the diagnosis of MS according to the McDonald criteria and were on immunomodulatory treatment ( McDonald et al., 2001 ). Inclusion criteria were age between 21 and 65 years, residency in Athens, relapsing-remitting MS and low physical disability as determined by an Expanded Disability Status Scale (EDSS) score of below 4.0 ( Kurtzke, 1983 ). Exclusion criteria were relapse during the last month, co- morbidity with a major psychiatric disease (i.e., psychosis, major depression, or substance abuse), participating in psychotherapeutic or other stress management therapies and inability to read or write. Eligible patients were randomized to two groups, the intervention and the control groups, using random numbers generated by an online generator (www.random.org). The follow-up period was twelve weeks, and both the patients and the researchers remained non-blinded to assignment and measurements.
At baseline, both groups received verbal and written information about the value of cognitive training, healthy lifestyle, stress management and self-efficacy in MS. The patients in the intervention group were administered the PSAI comprising 8 sessions. During the first individualized session (day 0), the patients were assessed by standardized questionnaires (see below) and a detailed discussion about cognitive training, healthy lifestyle (issues on smoking, diet, physical exercise and sleep), stress management and self-efficacy was had with experienced psychologists who were certified in PSAI by the Postgraduate Program “The Science of Stress and Health Promotion” of the Medical School of Athens in collaboration with the Scientific Corporation of Stress Management and Health promotion. This certification was given after one year of training and practice. Pedometers were also given as an incentive for exercising. In the second session (day 3) 3 - 5 patients participated in a biofeedback-assisted diaphragmatic breathing training. Additionally, guidance on diet, physical exercise and sleep was delivered. The third session (day 7) was evaluative, and the patients participated in group discussions of practical issues or ideas that might have emerged during the previous days. In the fourth group session (day 10) the participants were instructed on the PSAI technique. All participants were asked to perform the technique two times per day (morning and bedtime) after 5 minutes of diaphragmatic breathing. In the next three group sessions (days 30, 50 and 70) lectures (1 hr and discussion) about memory, lifestyle and intrapersonal relationships, respectively, were given, along with proper expatiation on the Pythagorean philosophy. During the final visit (day 84) discussion about the technique and final assessments were held.
The patients in the control group were contacted by telephone on days 3, 7, 10, 30, 50 and 70 after study entry. In each communication, the patients were asked about their physical and psychological status, with no intention to give in-depth counseling or intervention. On day 84 the controls had their final evaluations.
Pythagorean Self-Awareness Intervention―PSAI
The PSAI was practiced twice per day (in the morning and at bedtime) in a quiet place while sitting comfortably in a chair. The content of the technique is based on the golden verses of Pythagoras (http://en.wikipedia.org/wiki/The_golden_verses_of_Pythagoras), which serve as a frame of reference for one’s actions. At night, each individual had to follow three cognitive processes. First, the individual had to recall, from a 3rd person perspective, every event through the day in the exact time sequence that it happened, as if he/she could see his/herself in a “movie”. First, the individual had to recall every event through the day in the exact time sequence that it happened. To facilitate recall, events were categorized as follows: diet (e.g., “What did I eat or drink for breakfast?”), exercise (scheduled or not), sleep (timing, hours of sleep, etc.) and personal contacts. In the second step, the individual was asked to choose the events that seemed important to him/her and remember all the details accompanying them (e.g., the exact quantity of food at breakfast or all the words used in a discussion). For the categories of diet, exercise and sleep, the details were straightforward. However, for personal contacts, the individual had to choose those that seemed to bear any personal or emotional significance. During the last step, each selected event was subjected to critical appraisal using three questions: “Is what I have done wrong? Is what I have done right? What have I omitted that I ought to have done?” In this step, the individual tried to remain detached from the emotional burden of the event and contemplate on the performed actions as if he/she were a “judge” of him-/herself. With regards to diet, exercise and sleep, guidance had been given during session two. Events or choices pertinent to personal relationships were judged freely by the individual because the primary goal was to enhance self-awareness and not to criticize. After this cognitive process, in other words through positive (rejoice) and negative (reprimand) self-reinforcement, the individual was asked to set, when possible and applicable, specific goals for the day to come. In the morning, each participant was instructed to recapitulate the results of the previous night’s practice without repeating the procedure.
2.1. Measurements
Sociodemographical and disease-related characteristics: gender, age, marital status, educational level, disease duration.
Healthy Lifestyle assessment: This is a score reflecting the degree to which an individual follows a healthy daily lifestyle. The score was derived by taking into account smoking, exercise and dietary habits using the following questions and scoring: 1) “Do you smoke?” Answers: no or past smoking = 2, occasionally = 1, at least 20 cigarettes per day = 0; 2) “Do you exercise regularly i.e., at least 30 min each time?” Answers: No = 0, once or twice per week = 1, at least twice per week = 2; and 3) “Please indicate the frequency that you eat each food category during a regular week”, answers: for fish/fruits/vegetables/legumes are scores as No = 0, once per week = 1, at least once per week = 2, whereas meat is reversely scored. Higher scores indicated healthier lifestyle (min = 0, max = 12).
Depression Anxiety Stress Scale (DASS-21): Depression, anxiety and stress were measured using the corresponding 7 items of the DASS-21 ( Lovibond & Lobivond, 1995 ). The respondents indicated the frequency of symptoms in a Likert-type scale (from 0 = did not apply to me at all to 3 = applied to me very much or most of the time) during the past week. Scores are produced by summing all items. Higher scores indicate higher levels of depression, anxiety or stress. The scale has been adapted to the Greek population ( Lyrakos et al., 2011 ). Cronbach’s alphas coefficients for depression, anxiety and stress in this study were 0.902, 0.850 and 0.891, respectively.
Ways of Coping questionnaire (WCQ): Ways of coping were measured using the Greek version is a 38-item questionnaire originally developed by Lazarus and Folkman to assess the ways that a person reacts in the face of stress ( Folkman & Lazarus, 1988 ; Karademas, 1998 ). Individuals are asked to indicate the frequency of adopting each of the presented ways of coping in a Likert-type scale (from 0 = “does not apply and/or not used” to 3 = “used a great deal”). We used four subscales of the Greek version of the WCQ: confrontive coping, seeking social support, escape-avoidance, and positive approach (corresponding to the originally described subscales of problem solving and positive reappraisal).
Fatigue assessment: Fatigue was divided into three subscales: physical, mental and cognitive. Assessment was made using a visual analog scale of a 10-centimeter (cm) long straight line numbered from 0 (no fatigue) to 10 cm (excessive fatigue). Each individual indicated the level of his/her fatigue during the past week by marking these lines. Measurement from point 0 was expressed in millimeters (mm). Higher scores indicated higher levels of fatigue.
Symbol Digit Modalities Test (SDMT): This test is widely used for the evaluation of information processing speed ( Langdon et al., 2012 ; Sheridan et al., 2006 ). It consists of nine symbols that correspond to nine numbers (from 1 to 9). The responder was presented with a set of pseudo-randomized sequences of symbols and asked to verbally indicate the corresponding numbers in 90 seconds. The score indicates the number of correct responses during this time period.
California Verbal Learning Test -II (CVLT-II): this test evaluates immediate verbal learning and memory by asking the individuals to recall as many words as possible of a total of sixteen words (conceptually belonging in four categories; four words in each category) which are read by the examiner ( Langdon et al., 2012 ; Stegen et al., 2010 ). The process is repeated five times, and the total score is determined by the total number of correct recalls (maximum 80).
Brief Visuospatial Memory Test-Revised (BVMT-R): This test evaluates visuospatial memory ( Langdon et al., 2012 ; Benedict, 1997 ). The individual was presented with a matrix of six items in two columns and three rows for ten seconds, and he/she was asked to replicate the matrix unaided using pencil and paper while taking as much time as needed. The process was repeated three times. Each drawing was evaluated for both its placement (1 point) and its accuracy (1 point). Thus, the maximum score yielded by the three trials was 36, indicating unimpaired visuospatial direct memory recall.
2.2. Statistical Analyses
Descriptive statistics were used for categorical (i.e., frequencies) and interval characteristics (i.e., means; standard deviation, SD; and minimum values, Min; and maximum values, Max). The homogeneity of the study groups was assessed with Student’s t-tests and Pearson’s chi-square tests. The test of normality included inspection of Q-Q plots and the Kolmogorov-Smirnov test. Group comparisons for the main study endpoints were performed with the analysis of covariance test (ANCOVA) after adjusting for age, disease duration and baseline values of the outcomes. The assumption of the homogeneity of regression slope was evaluated by inspecting the graphs of the putative confounder relative to the outcome for the different study groups and by exploring the significance of the group × confounder interaction in the models. The effect size was calculated according to the formula: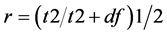 , where r = 0.1, 0.3 and 0.5 represent a mild, moderate and large effect, respectively. The level of significance was set at p = 0.05. Analyses were conducted with SPSS 20.0 (Chicago IL).
, where r = 0.1, 0.3 and 0.5 represent a mild, moderate and large effect, respectively. The level of significance was set at p = 0.05. Analyses were conducted with SPSS 20.0 (Chicago IL).
3. Results
In total, 149 patients were assessed for study entry, and 64% of these patients were found eligible according to the inclusion/exclusion criteria (Figure 1). Of the 96 eligible patients, 21 (22%) refused to participate. The main reasons for refusal were the long follow-up period and the disbelief in non-pharmaceutical interventions for treating MS. As a result, 75 patients were equally randomized to the two study groups. The drop-out rate was significantly higher in the intervention group than in the control group (37.8% vs 15.8%, respectively). Loss to follow-up for unknown reasons was larger in the intervention group (8 patients) than in the control group (3 patients). In the intervention group, five patients discontinued for reasons that were declared to be not pertinent to the program (e.g., 2 patients reported death of a relative, 1 patient lost his job and 2 patients reported family problems). As a result, two unequal groups emerged for analyses (23 patients in the intervention group and 32 patients in the control group).
Table 1 presents the baseline group comparisons. The majority of the patients were women, mostly married, with tertiary education and a mean disease duration of approximately ten years. All patients had an EDSS score below 4.0 and were on immunomodulatory treatment (not showed). No significant group differences were noted, except for the mean BVMT score, which was larger in the intervention group than in the control group.
Table 2 presents the group comparisons for the main study endpoints after adjusting for age, disease duration and baseline measurements for each outcome. Beneficial outcomes were found for nearly all outcomes except for confrontative coping, escape-avoidance coping and BVMT scores. Specifically, large beneficial effect sizes (effect sizes r > 0.45) of the intervention were recorded for healthy lifestyle, stress, depression, positive approach, physical, mental and cognitive fatigue scores. Medium beneficial effect sizes (0.25 < r < 0.45) were re-
![]()
Figure 1. Flowchart of process of selecting participants.
trieved for anxiety, seeking social support, SDMT and CVLT scores.
Finally, no side effects or serious practical issues during the intervention were reported.
4. Discussion
In this study, PSAI had beneficial effects on physical, mental and psychological wellbeing of the MS patients of our sample. Loss to follow-up was larger in the intervention group than in the control group and was for unknown reasons for eight intervention patients and three control patients. All patients who received the intervention and completed follow-up liked the technique and reported no side effects or negative thoughts related to practicing it. This is a newly introduced intervention; thus, direct comparison with other non-pharmaceutical interventions is cumbersome. The recorded benefits could be explained only by heuristic interpretations made on the basis of available evidence and putative analogies with other well-established interventions, such as cognitive behavioral therapy (CBT).
A central feature of PSAI was stress management. We believe that stress management was accomplished by both the diaphragmatic breathing and the cognitive appraisal of the daily events. Combining emotional- and problem-focused coping was an important asset of this intervention because both have been shown to improve physical and mental well-being, self-efficacy and adaptation to the disease ( Plow et al., 2011 ; Graziano et al., 2014 ). More importantly, stress tackling through problem-focused coping, along with seeking social support and positive thinking which were found significantly increased in this study, has been suggested to enhance psychological adjustment to the disease ( McCabe et al., 2004 ). Similarly, in a randomized controlled trial (RCT) both CBT and relaxation training improved fatigue as in our study, although the effect of CBT which combines
![]()
Table 1. Baseline characteristic and study group comparisons.
SD: Standard deviation, Min-Max: Minimum-Maximum values, SDMT: Symbol Digit Modalities Test, CVLT: California Verbal Learning Test, BVMT: Brief Visuospatial Memory Test, *Level of significance p < 0.05.
problem- and emotional-focused stress coping, was greater ( van Kessel et al., 2008 ). To our knowledge, there is no direct evidence that stress management can improve cognitive function in MS. We hypothesize that stress alleviation could reverse the inflammatory process and the ensuing neurodegeneration implicated in the cognitive decline of MS patients ( Lovera & Reza, 2013 ). However, our study found significant differences for information processing speed and verbal learning and not for visuospatial memory, which indicates that certain domains of cognition may be more amenable to change through stress management.
Another central characteristic of PSAI was memory recall and cognitive appraisal of daily events. There is scarce evidence attesting that memory training interventions may enhance memory function in MS patients ( Sumowski et al., 2010 ; Goverover et al., 2009 ; Allen et al., 1998 ). As stated above, it is speculated that cognitive rehabilitation in MS activates brain networks (e.g., DMN) representing cognitive reserve ( Bonavita et al., 2011 ; Sumowski & Leavitt, 2013 ; Rosti-Otajärv & Hämäläinen, 2014 ; Penner et al., 2007 ; Bonavita et al., 2015 ). Interestingly, DMN is also implicated in meta-cognitive functions, the mental process of internal consciousness and contemplation (“knowing about knowing”) ( Li et al., 2014 ). PSAI has a strong resemblance to
![]()
Table 2. Adjusted mean values for the main study endpoints and group comparisons after 12 weeks of follow-up.
SD: Standard deviation, CI: Confidence Interval, SDMT: Symbol Digit Modalities Test, CVLT: California Verbal Learning Test, BVMT: Brief Visuospatial Memory Test; 1Analysis of Covariance (ANCOVA), adjustment for age, duration of disease and baseline scores; 2Analysis of Covariance (ANCOVA), adjustment for age, duration of disease, baseline BVMT and group × baseline BVMT. Adjusted means were calculated for a BVMT score of 21.87; *Level of significance p < 0.05.
this meta-cognitive process; as such, there are many implications for mental and cognitive health based on the available evidence. Collectively, the meta-cognitive process has been found to enhance healthy lifestyle and self-awareness and to improve decision making, empathy, relaxation, psychological status and cognitive functions ( Slagter et al., 2011 ; Metcalfe & Shimamura; 1994 ). As such, the lifestyle, psychological and cognitive benefits ascertained in this study could be explained by this process of meta-cognition. In particular, self-awareness and self-regulation, which are interwoven in meta-cognition, might mediate these personal improvements noted in PSAI.
As far as depression is concerned, it is well-established that depression is associated both with stress and MS via neurohormonal (e.g., dysregulation of the HPA axis), physical (e.g., fatigue) and psychosocial factors (fear and/or frustration deriving from the progressive nature and the unpredictable course of this disease, quality of life, etc.) ( Heesen et al., 2003 ). The results derived from the implementation of the PSAI seem encouraging in the amelioration of depressive symptomatology. We believe that this fact could be interpreted both on a direct and an indirect level. The direct explanation could include immune and neurohormonal changes as well as amelioration in cognitive impairment ( Janssens et al., 2003 ). Several studies have shed light on the emotional burden that cognitive deficits induce in the patient’s life. On the other hand, the indirect level could elucidate the detrimental role of quality of life (QoL), self-esteem and fatigue. In fact, there seems to be a reciprocal relationship between depressive symptomatology and quality of life. Hence, individuals experiencing more depressive symptoms have poorer QoL and vice versa.
The current literature reports that MS patients with ongoing depressive symptoms perform poorly on cognitive tasks assessing information processing speed, attention, etc. ( Arnett et al., 1999 ) Cognitive impairment is dominant in depressed MS patients, affecting effortful but not automatic information processing. This may mean that the individual might perform well in standardized actions and tasks but might face difficulties in those tasks that require attention (e.g., information processing, working memory, etc.) and planning. Moreover, the existing literature states that negative mood and self-evaluations are closely associated with cognitive impairment. It still remains unclear whether depression precipitates cognitive deficits or whether it emerges as an aftermath of the cognitive function loss. PSAI, on one hand, fosters a more “realistic” view of the individual’s actions and thoughts (3rd person narrative perspective) through cognitive appraisal and thus could contribute to a positive self-image; on the other hand, the element of setting specific goals every day could be beneficial for detaining or even ameliorating the individual’s cognitive deficits ( Beiske et al., 2008 ). Moreover, effortful recall is another essential element of the PSAI, which in turn, could explain the statistically significant reduction in depressive symptomatology and the observed improvement in the post-intervention memory tests.
Furthermore, self-esteem and social support appear to have a buffering effect on stress and depressive symptomatology because they are implicated in stress perception and management. Self-esteem and social support are closely associated with life and self-satisfaction and thus are affected by the perceived level of function in everyday life (it is common for patients with MS to report feeling like a burden to their family and loved ones). Additionally, self-esteem is associated with treatment compliance, implementation of effective coping strategies, positive self-image and perceived control over one’s health ( Foote et al., 1990 ). Those parameters could be summarized as self-management, which includes psychological, instrumental, cognitive behavioral and social factors. According to current literature, those elements serve primarily as stress buffers; they mitigate the uncertainty and ambiguity deriving from stressful. Coping with the uncertainty and unpredictability of symptoms and the progression of MS helps the individual maintain a positive self-image and increase his/hers perception of control over his/her disease, thus having an impact on depressive symptomology and fatigue levels. The PSAI is guided by the golden verses, whose primary aim is to empower responsibility over one’s life, (e.g., dietary counselling, mood regulation, anger management etc.), especially through positive and negative reinforcement. Thus, the PSAI fosters the development and enhancement of self-management, (e.g., problem solving, decision making, active entanglement etc.), which could explain the statistically significant increase in social support seeking and the reduction in stress, depression, anxiety and fatigue ( Feicke et al., 2014 ).
Fatigue in MS appears to be multifactorial and constitutes a crucial factor in the emotional and physical burden that MS has on the patient’s life. Fatigue is usually the first symptom of MS, is present in the majority (75% - 95%) of MS patients and is related to disability, depression and quality of life ( Rieckmann et al., 2015 ; Pittion-Vouyovitch et al., 2006 ) quality of life is related to matters of mental health, physical strength-ability, vocational life, etc. Fatigue in multiple sclerosis is related to disability, depression and quality of life. According to studies, fatigue experienced by MS patients differs from that of healthy individuals because it imposes great physical and emotional burden on the individual. Furthermore, there is a well-known relationship between fatigue in MS and dysregulation of the HPA axis, a relationship that could explain the reduction observed in our study in all three aspects of fatigue. More specifically, the levels of mental, physical and emotional fatigue were significantly improved, thus revealing the direct impact of the PSAI on the mitigation of the deleterious effects of stress and depressive symptomatology ( Pittion-Vouyovitch et al., 2006 ).
Anxiety manifests with emotional and behavioral changes that emerge as an extreme or aberrant stress response. Thus, stress management could prove beneficial in alleviating anxiety symptomatology ( Johnson et al., 1992 ). Studies in patients with MS show that high levels of anxiety could be associated and interplay with chronic pain and disability status. Furthermore, anxiety is associated with poorer quality of life and general health ( Janssens et al., 2003 ; Beiske et al., 2008 ). The results of our study reveal a statistically significant reduction in anxiety levels post-intervention. One possible explanation could be that PSAI, via cognitive appraisal, may strengthen the perception of self-management and self-awareness, thus resulting in more effective stress management and mood regulation ( Beiske et al., 2008 ; Janssens et al., 2003 ).
Moreover, we note some qualitative comments recorded during the extra session, which took place after 3 months. The majority of the participants reported: a) maintaining the changes introduced by the intervention program in their lifestyle and daily routine (diet, exercise and sleep); b) having better interpersonal relationships, specifically in setting boundaries and defending their needs/wants; c) being more effective coping in cases of stressful events; and d) experiencing an improvement in memory (recall and planning).
Admittedly, this study suffers some limitations. First, the loss to follow-up was increased in the intervention group and remained mostly unexplained, which could raise some skepticism about the attractiveness of PSAI to certain individuals or personality types. Future studies will clarify this still nebulous issue. Second, we did not choose any intention-to-treat methods primarily because this was a concept of thought study, which meant that our goal was to ascertain any possible benefit of this new technique. We admit that this could result in type I errors for our results. However, the low power of our study, due to both the small sample and the randomization process for allocation, might compensate for this unwanted possibility. Third, the follow-up period of twelve weeks might be considered too short for significant changes to occur. Moreover, the patients were not evaluated for the time period after intervention. Finally, no classical MRI or clinical endpoints for MS were used.
Despite these limitations, PSAI holds promise for the lifestyle, cognitive and psychological aspects of MS. PSAI could be considered an inclusive, meta-cognitive process of stress management and self-empowerment that has close resemblance to CBT but, in our view, is accompanied by a deeper philosophical reflection. In the absence of previous evidence, speculations could be made only about the mediators of the accomplished benefits in this study. The strong advantages of PSAI include that it is easily taught; is time- and money-saving; and, after training is finished, it could be practiced by the participant for a lifetime. Future RCT studies with larger samples and more robust MS clinical endpoints are strongly encouraged.
Acknowledgements
We would like to thank the philosopher Dr. Altani for inspiring us to develop and design PSAI in adherence to the basic principles of the Pythagorean philosophy.
NOTES

*Corresponding author.
#These authors contributed equally and shared last authorship.