The Effects of Low Dose Sertraline on Blood Pressure in Patients with Hypertension and Panic Disorder: A Pilot Study ()
1. Introduction
This pilot study proposed to meet the objectives as listed below; however due to difficulty with recruitment, only 2 out of 4 participants will be discussed in the analysis.
Objectives
1) To determine whether Selective Serotonin Re-uptake Inhibitors (SSRI) are a successful adjunct therapy in lowering blood pressure in hypertensive patients with panic disorder.
2) To explore the role of the serotonergic system in regulating systemic blood pressure and panic symptoms.
3) To produce pilot data for submission to the NHMRC/Australian Heart Foundation project grant and to perform a sample size calculation for a larger trial.
Hypothesis: There will be a significant improvement in 1) systolic and 2) diastolic blood pressure in patients with essential hypertension and panic disorder after 28 days of adjunct therapy with an SSRI therapy compared with baseline values.
Literature Review
The heart foundation defines hypertension as blood pressure (BP) ≥ 140/90 mmHg [1] . Hypertension affects approximately 32% of Australians aged 18 years and above and is the greatest contributor (42.1%) to the burden of cardiovascular disease [2] . A quarter of the burden of disease in mental illness is accounted for by anxiety disorders [3] . The lifetime prevalence of panic disorder is between 1.4% and 2.9% with a higher incidence of females experiencing agoraphobia [3] ; a large number of people suffering from panic disorder do not seek treatment resulting in indirect economic and social consequences e.g. work disability and difficulties within the family [3] [4] [5] .
Since the discovery of serotonin (5HT) in 1948, the effects it has on the cardiovascular system have been well known, especially in the mediation of vascular tone [6] . At present, the Selective Serotonin Reuptake Inhibitors (SSRIs) are first line in the treatment of major depressive disorders and anxiety disorders. SSRIs are preferred by clinicians for their relative safety in overdose, tolerability with limited adverse effects and broad clinical efficacy. Despite the well-established correlation between depression and cardiovascular disease [7] , there is only limited and relatively recent literature suggesting that hypertension and anxiety/panic disorders are linked [8] .
Previously, research focused on the correlation between major depression and hypertension, with less literature focusing on the role of panic disorders in hypertension [9] [10] ; especially with hypertension being a significant risk factor for cardiovascular disease [7] .
The study by Davies et al. [11] was of particular interest. Their aim was to determine if there was a relation between panic attacks and panic disorder to hypertension. The authors divided 891 patients into three groups: 1) Hypertensive patients in primary care, 2) Matching normotensive controls from the same primary care practice, and 3) Hypertensive patients attending hospital clinics. They found a significant difference between the groups (p < 0.001) with 37% of hypertensive patients experiencing panic attacks compared to 21% of normotensives. Moreover, panic disorder was significantly more common in hypertensive patients studied in primary care then in matched normotensives. Prospective studies have also reported this association, although none of these studies have combined a robust method for diagnosing anxiety disorders or for diagnosing cardiovascular endpoints.
In a separate study, Davies et al. [12] attempted to account for “White Coat Hypertension” i.e. people with anxiety are more likely to be anxious in a health related situation, which is an important variable that may explain why hypertension and anxiety co-occur. Nonetheless, Davies et al. found no significant difference in the white coat effect between hypertensive patients with panic and those without [12] , hence suggesting that sustained rises in BP may be more relevant in anxious patients rather than acute rises in BP found in the “white coat effect”.
Patients with anxiety disorders responsive to SSRIs have an increased cardiovascular [13] and psychological response [14] to stressors when depleted of tryptophan in comparison with patients who are not depleted of tryptophan as shown in acute tryptophan depletion where synaptic serotonin is transiently reduced via a non-invasive dietary technique [15] [16] .
The above is in comparison to healthy volunteers who had a more robust 5-HT system and hence did not show an increased cardiovascular or psychological response to stress when tryptophan depleted [17] . The integrity of the serotonin system in patients with BP regulation difficulties, as determined by the ability to buffer the stress response under tryptophan depleted conditions compared with the non-depleted condition, has yet to be studied.
The susceptibility of patients with hypertension and panic disorder to a pressor effect via the acute depletion of central serotonin may shed light on the possibility of the use of additional SSRI to improve the management of their BP.
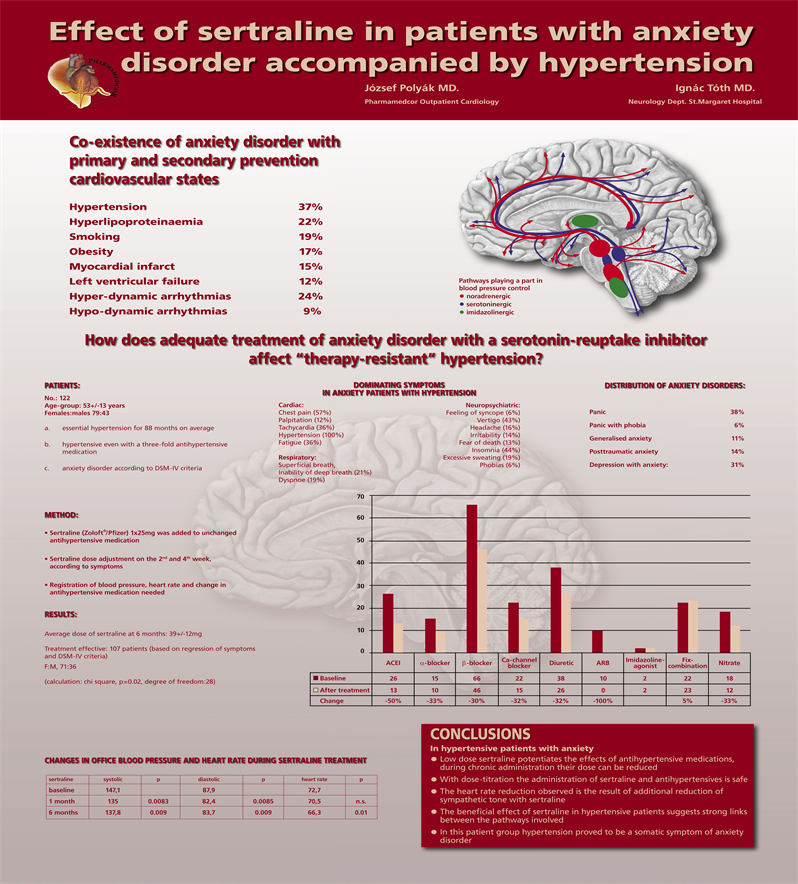
A study with unpublished data conducted by Polyak and Toth studied adult patients with both hypertension, on a range of antihypertensives, and anxiety disorders (Appendix 2) [18] . They have prescribed a low dose of sertraline (mean 39 mg daily) in addition to their regular antihypertensives and their BP measured at 1 and 6 month periods (Appendix 2) [18] . A significant improvement in systolic and diastolic BP (DBP) of 10 mmHg and 5 mmHg respectively was observed [18] .
The efficacy of escitalopram, was studied in the treatment of generalised anxiety disorder in the elderly and had a promising antihypertensive effect [19] . There was significant improvement in BP observed in the participants, as a secondary outcome, with a mean improvement of 23.3 mmHg as compared to the placebo (12.4 mmHg) in the top quartile for systolic BP (SBP).
The BP lowering effects of the SSRIs described in the studies above fared quite well as compared to common antihypertensives e.g. the ACE-inhibitor ramipril had a mean BP lowering of 3/2 mmHg in a large cardiovascular trial, demonstrating significant reduction in major cardiovascular events in the treatment group [20] . Such small degrees of BP lowering are associated with significant long term benefits among those at risk of cardiovascular events [21] [22] —a BP reduction of 10 mmHg systolic or 5 mmHg diastolic was observed to have a 22% reduction in coronary heart disease events and a 41% reduction in stroke [21] . Hence, even if small BP lowering effects of SSRI drugs are confirmed, the potential for favourable long term cardiovascular outcomes would also require evaluation.
In this pilot study, given the prevalence of hypertension and panic disorder as described in the literature, we proposed to fill the gaps in the literature on the possible utility of SSRI medication as an adjunct treatment in individuals with panic disorder and hypertension. We planned to only recruit patients with panic disorder who fit the criteria independently for treatment with SSRI i.e. treatment would be given based on clinical need and currently accepted Pharmaceutical Benefits Scheme (PBS) criteria. Thereafter, we would monitor their BP at baseline, 14 days and 28 days to determine if there has been an effect on the individual’s BP.
2. Methods
2.1. Participants and Recruitment
Ethics approval was granted by the Human Research Ethics Committee (HREC) at Sir Charles Gairdner Hospital and Fremantle Hospital for recruitment of up to 35 (n = 35) male and female adult patients via the hospital’s outpatient cardiology clinic. Patients were referred by the cardiologists and cardiology registrars at the clinic and then these patients were seen by the clinical investigators to outline the general principles of the study, screen for eligibility to ensure they met the inclusion and exclusion criteria and gain written informed consent for those wishing to participate. Patients were provided with an information sheet detailing the project with contact numbers and a copy of their consent form.
Inclusion Criteria:
· Age > 40;
· Male or Female;
· Diagnosed panic disorder suitable for SSRI therapy;
· Diagnosed hypertension and on at least one medication for hypertension;
· Access and availability to attend at least three hospital sessions;
· Able and willing to provide written informed consent;
Exclusion Criteria:
· Cardiovascular instability;
· Hypotension;
· Current active malignancy;
· Pregnancy or breast-feeding;
· Involvement in another clinical trial;
· Current or recent (within 90 days) DSM-IV Major Depressive Disorder;
· Hypersensitivity to, or currently using, any serotonergic medication;
· Contraindication to serotonergic medication;
· Rural or remote location, or unable to attend for at least three hospital sessions.
Patients who fit the eligibility criteria for the study were invited to attend an appointment with the principal investigator for assessment of panic disorder. Panic disorder was diagnosed according to the Mini International Neuropsychiatric Inventory (MINI) v5 [23] .
When panic disorder was diagnosed, the patient was then invited to attend a baseline formal assessment of their BP via a 24-hour ambulatory blood pressure monitor (ABPM). This test was requested through the cardiology department of the same tertiary hospital. The BP was measured at the brachial artery of the non-dominant arm using an automatic battery-powered electronic sphygmomanometer, and recorded on the on-board memory device. BP was measured every 30 minutes during the day and hourly at night. ABPM reflects not only the diurnal variation in BP, but also reflects real-life situations that vary throughout the day [24] [25] . After the 24 hour recording was completed, the BP monitor was returned and data downloaded to automated software and stored on a secure server. The data was then deleted from the recording device.
Panic symptoms were measured by the Commonwealth Panic Symptom Inventory (CPSI) v1.0 (Appendix 1), which assessed autonomic and non-autonomic panic symptoms and changes in those symptoms, and the Spielberger State-Trait Anxiety Inventory-State (STAI-State) [26] . These screening questionnaires were performed by the principal investigator and participant respectively at baseline, 14 days and 28 days.
Patients diagnosed with panic disorder were suitable for treatment with SSRI medications based on the current Australian PBS criteria.
2.2. Intervention
If the patient’s average BP reading was greater or equal to 130/80 mmHg [27] [28] [29] using the above technique and they had a diagnosis of panic disorder, they were prescribed sertraline in a non-randomised open label fashion with their consent. According to routine clinical practice, patients started on 25 mg mane orally for the first week and then increased to 50 mg mane in the second week. Thereafter, dosing was naturalistic and was determined by the prescriber according to routine clinical assessment.
Patients were informed that sertraline was indicated as a standard treatment for panic disorder in Australia and thus administered using PBS criteria on routine clinical grounds.
Patients were given a list of emergency contact numbers if the patient or their family had immediate concerns regarding treatment.
2.3. Outcome of Interest
The primary outcome of interest was the difference between the changes in systolic and diastolic BP in subjects over the course of 14 and 28 days. After commencing sertraline, patients attended a clinical review with the principal investigator at 14 and at 28 days. Patients were assessed for possible therapeutic benefit of sertraline using the CPSI and STAI-State at baseline, 14 and 28 days.
At 14 and 28 days of treatment, the patient had another 24-hour ABPM fitted and the principle investigator assessed and discussed the clinical need, or otherwise, of ongoing treatment with sertraline. Referral to a Psychiatrist or to their General Practitioner (GP) was recommended depending on the participant’s clinical needs.
2.4. Data Analysis and Power Calculation
Using data from Polyak [18] [30] and Lenze et al., [19] a minimum sample size of 35 was estimated to be necessary in order to detect a difference of 12 mmHg assuming a standard deviation of 12 using an independent, 2-tailed t-test with power = 0.8 and alpha = 0.05.
Thereafter, exploratory analysis considered 1) any differences in BP response as a function of existing anti-hypertensive treatments, 2) any differences in 24 hour ambulatory blood pressure, and 3) the relationship between changes in panic attacks and BP improvement using regression analysis.
Due to the current sample size and after discussion with the project supervisor, we decided to present our pilot data as naturalistic and observational. Only descriptive statistics are presented here.
3. Results
Case 1 This 67-year-old male (Patient 1) had been attending the outpatient cardiology clinic for the past 4 years for management of resistant hypertension. He had a strong family history of cardiovascular disease and was on amlodipine 10 mg daily, ramipril 10 mg daily, atorvastatin 20 mg and aspirin 100 mg. He was a non-smoker and did not drink alcohol. He had modified his diet i.e. low salt and had been exercising regularly i.e. walking 3 - 4 times a week for the past year. He was averaging BP of 165/100 mmHg during his outpatient appointments for the past 7 months.
He had worked as a technician in an operating theatre for the past 30 years and did not find his job stressful. His chief concern was fear of another panic attack, especially whilst at work or in public. He had experienced 2 panic attacks over the last week and had been struggling with spontaneous panic attacks over the past ten years but did not feel comfortable discussing this with his GP as he felt it would make him look “weak”. He had no history of previously diagnosed mental illness, thus has not had psychotropics or benzodiazepines previously. He had no family history of mental illness.
He initially expressed concerns regarding the questions on the mini v5, but responded well to reassurance. We discussed his diagnosis of panic disorder and he found that it was an accurate description of his condition that he had been struggling with for the past decade.
At the first follow-up appointment 14 days after commencing sertraline, he reported a three day history of mild nausea, which subsided. There were no other side/adverse effects reported. He experienced 1 panic attack of similar intensity to his previous panic attacks since our last review.
At our final appointment 28 days after commencing sertraline, he reported no side/adverse effects. He reported 1 panic attack since our last review; nonetheless, he was pleased at the reduction in the intensity of symptoms he experienced during the panic attack. He wanted to continue sertraline 75 mg and said he would consider increasing the dose of the medication at his GP’s discretion. We advised him to attend regular appointments with his GP to monitor his medications and mental state.
Case 2 This 64-year-old male (Patient 2) had been attending the outpatient cardiology clinic for the past 2 years for management of resistant hypertension and unstable angina. He had a strong family history of cardiovascular disease and was on perindopril 5 mg/indapamide 1.25 mg, atenolol 100 mg, aspirin 100 mg and rosuvastatin 20 mg. He had no history of previously diagnosed mental illness.
He struggled with exercise due to his angina and shortness of breath. He had been experiencing spontaneous panic attacks for the past 18 months however did not seek medical attention as he thought it was related to his worsening cardiac health. He had been averaging 4 spontaneous panic attacks per fortnight.
He owned his own business and found his job physically and mentally demanding. He had quit smoking 8 years ago and was a pack a day smoker for 20 years previously. He had 2 - 3 standard drinks of red wine per week, he had no prior history of alcohol abuse or dependence.
Similarly, he found the symptoms described on the mini v5 an accurate description of his experience over the past 18 months. He expressed his frustration at the difficulty controlling his BP and the multiple previous cardiac medication combinations he has tried to no avail.
He attended our first follow-up appointment 14 days after commencing sertraline. He reported 4 panic attacks since our last review with slightly reduced intensity. He reported no medication side effects or adverse effects.
At our final appointment 28 days after commencing sertraline, he reported no side/adverse effects. He reported 1 spontaneous panic attack since our last review; however he was pleased with the reduced intensity of the panic attacks since commencement of sertraline. He was keen to continue sertraline at 75 mg and we encouraged him to have regular appointments with his GP to titrate his medication and monitor his mental state.
Cases 3 and 4 did not meet the inclusion criteria or enrolled in the study; they illustrated some specific challenges we faced in this pilot study.
Case 3 This 65-year-old female, living in the country had been attending the outpatient cardiology clinic for the past 5 years for monitoring of her cardiac health after a myocardial infarction 2 years previously which resulted in 2 cardiac stents. She was managed for hypertension and hypercholesterolaemia. She had no family history of mental illness or cardiovascular disease and was on rosuvastatin 20 mg daily, irbesartan 300 mg daily and aspirin 100 mg.
She had quit smoking approximately 35 years ago and had smoked half a pack of cigarettes per day for 6 years prior to quitting. She had 1 - 2 standard drinks fortnightly and had no history of previously diagnosed mental illness, alcohol abuse or dependence.
She started going on daily walks after her myocardial infarction. Approximately 8 months ago, she developed spontaneous panic attacks and stopped going for her walks as she feared experiencing a panic attack whilst in public. She also stopped going to the shops on her own as she was fearful of a spontaneous panic attack without her husband around. She had been driving down to the hospital for her appointments in the company of her husband. She had no previous or family history of mental illness.
She did not seek medical attention at her GP as she was afraid of people in the community finding out about her condition. She was keen on participating in the trial however could not commit to the follow-up appointments due to residing 5 hours away in the country. We advised her to speak to her GP about her concerns, reassured her about confidentiality and offered our contact details.
Case 4 This is a 47 year old male who was an IT technician at a telecommunications company. He had been attending the cardiology clinic for the past 3 months for management of resistant hypertension. He was managed by his GP previously however his GP found it challenging when the patient developed metabolic syndrome. He was on candesartan 12 mg, atorvastatin 40 mg and had impaired glucose tolerance which was diet controlled.
He had a strong family history of cardiovascular disease, type II diabetes, and mental illness i.e. depression and anxiety. He was a non-smoker and had 3 - 4 standard drinks of beer per week. He did not have a personal history of previously diagnosed mental illness, alcohol abuse or dependence. He had a poor diet of mainly fast food and led a sedentary lifestyle.
Due to the short consultations with his GP, he briefly brought up his concerns regarding his spontaneous panic attacks, which were occurring 3 - 4 times monthly, however he said that his GP was dismissive of his concerns. After our interview with the mini v5, he said that he thought he may have had panic disorder in his teenage years as well. However, he was unable to commit to the follow-up appointments due to work commitments and difficulty with transport. We offered taxi vouchers however he declined. We encouraged him to speak to his GP to discuss this further and offered our contact details.
Analysis
With reference to Table 1, both patients had similar demographics apart from Patient 2 having 2 - 3 standard drinks of red wine per week.
Based on the results from the ABPM, Patient 1’s systolic BP decreased by 6 mmHg 28 days after the commencement of sertraline (Figure 1). Similarly, Patient 2’s systolic BP decreased by 4 mmHg in the same time period (Figure 1).
Patient 1’s diastolic BP decreased by 3 mmHg and Patient 2’s diastolic BP decreased by 5 mmHg 28 days after the commencement of sertraline (Figure 2).
There were no changes made to their respective anti-hypertensive medications during the study period.
The results from the Commonwealth Panic Symptoms Inventory (CPSI) showed that the number of panic attacks halved in both patients 28 days after commencement of sertraline (Figure 3). The intensity of panic attacks in both Patient 1 and 2 also decreased from baseline, at day 14 and day 28 (Figure 4).
With reference to Figure 5 and Figure 6, the degree of intensity of most symptoms decreased considerably from day 14 - 28 in both Patient 1 and 2 except “Nausea or abdominal stress” in Patient 2. The “Fear of dying” appeared to have the most considerable decrease in intensity in both patients.
There was an overall improvement in reported symptoms in both patients as reflected in the STAI-State scores over the course of 28 days (Figure 7).
Due to the small sample size, no statistical test could be performed. Nonetheless, based on the observation above, there may be a trend of a reduction in systolic and diastolic BP after the commencement of sertraline. In order to confirm this observation, a larger sample size is required in the future.
![]()
Figure 1. Systolic blood pressure (mmHg).
![]()
Figure 2. Diastolic blood pressure (mmHg).
CPSI
![]()
Figure 3. CPSI—Number of panic attacks in the past week.
4. Discussion
This project produced promising pilot data in support of a larger trial in the future. The two participants showed a reduction in systolic and diastolic BP after treatment with sertraline. In addition, they both experienced a decrease in the frequency and intensity of panic symptoms whilst tolerating the sertraline without incident.
The study clearly has a number of limitations. We had a very small sample size and therefore were unable to conduct a formal statistical analysis nor could we make broad statistical conclusions. However, the observations in this study were in line with our objectives for further recruitment in the future to increase our sample size. Through road testing this study, we were able to identify challenges in the study design which would lead to further changes in the study design for a larger study.
There was significant difficultly recruiting patients for this pilot study due to our strict inclusion and exclusion criteria. In our attempt to improve recruitment, we invited elective medical students who were on 6 week placements to help screen patients at the cardiology clinic. After which, the principal investigator contacted the patient to determine if they were suitable for the project. Over the last 3 years, we have had 4 groups of elective medical students, which contributed to their awareness of the challenge of clinical research.
We also increased the awareness of our project at the cardiology clinics with fliers, presentations at the cardiology journal club and direct communication with the cardiology treating team. We also held regular meetings with the cardiology consultant to brainstorm ideas to improve recruitment.
For the past 4 out of 36 months, we also had a research officer with a nursing background and PhD in the field of cardiovascular mental health, available once a week onsite to attend these weekly clinics with the medical students and help liaise with the cardiology technicians. She had a good working relationship with the cardiology department and was also well-known to the local nursing staff which contributed in making this process more seamless and convenient for patients to get their 24-hour ABPM fitted in a timely manner.
Professor Hood (Head of School at a local university, Psychiatrist and Scholarly Project Supervisor) also had a good working relationship with Dr McQuillan (Dean of UWA Medical School and Cardiologist) as they worked collaboratively in other projects and held related university appointments, hence helped the organisations work together.
Whilst all these measures were largely unsuccessful in improving recruitment for this pilot study, they do hold promise for enhancing recruitment into a larger, adequately powered, placebo-controlled randomised controlled trial.
Interestingly, the literature published by Davies et al. suggested that panic disorder was seen in approximately 37% of patients with hypertension [11] . The likely reasons underlying this dissonance between our experience and the literature could have been an overestimate from the literature regarding the prevalence of panic disorder in patients with hypertension, and/or there may have also been difficulty working across the interface of psychiatry and cardiology despite our attempts as described above.
One could also speculate that Polyak’s data [18] presented in poster form may not have reached publication due to problems with the initial dataset that they presented or there may have been issues with quality control. Hence, the results from his study may have been overly optimistic. There was also a sense of stigma associated with mental health amongst patients, especially given our experience with the patient in Case 3. This may be tackled in our future project via continuous patient and staff education regarding mental health and the importance of research in this area in the hope of stigma reduction and improvement in compliance rates in participants.
Funding constraints also limited our ability to increase participation and compliance with the study. Due to financial constraints, there was significant difficulty in organising transport if participants required assistance, which was the case in Case 4, however despite efforts. He decided not to participate in the project. Other participants were also reluctant to participate due to the lack of remuneration for participation in the project.
In view of our experience, we have considered the possibility that we were looking at the wrong patient group at the cardiology clinic. We may consider recruitment at GP practices as panic disorder was significantly more common in hypertensive patients studied in primary care then in matched normotensives [11] [31] however GPs may be reluctant as they may be over serviced and have busy practices [32] . However it may remain an option in our future project for GPs to be active partners in research rather than solely in service delivery. Expanding and refining our inclusion criteria may also be another aspect to look at for our future project, given the difficulties for recruitment with a narrow criterion, we may consider expanding the criteria for patients diagnosed with Generalised Anxiety Disorder.
There may have also been certain confounding factors that may have led to the observed improvement in BP for our 2 patients. Firstly, interviewing patients and engaging them in an empathic way by clinicians may have an added effect to the reduction of their anxiety levels. Moreover, one cannot discount that when dealing with patients in mental health, there may be unknown variables in those who were willing to stay in this research trial and those who were unwilling.
5. Conclusions
This project managed to produce some preliminary data which showed that a serotonergic drug might improve systolic and diastolic BP in patients with hypertension and panic disorder, in keeping with the data that Polyak described [18] [30] .
The promising findings in this project may allow future exploration of the use of SSRIs in anxious individuals with hypertension thus making this a stepping stone for a pivotal project, as otherwise such a therapeutic option will remain largely a theoretical research interest. This project also has the possibility of contributing to defining a population of patients with hypertension who achieve cardiovascular benefit from the prescription of a previously overlooked class of medication for treatment of hypertension.
Appendix 1
CPSI (Commonwealth Panic Symptoms Inventory)
1) How many Panic Attacks have you had during the past week? _______
2) Overall, how intense have your Panic Symptoms been over the past week? (0 - 100).
3) How intense have the following panic symptoms been for you over the past week?
v 1.0 (14/1/13) © university 2013.
Appendix 2