Female infertility and laparoscopic surgery: A series of 415 operations at the Yaounde Gyneco-Obstetric and Pediatric Hospital, Cameroon ()
1. INTRODUCTION
Since gynecological laparoscopic surgery was introduced in Cameroon [1], several studies have been dedicated to this new surgical approach in our setting [1-7]. Even though laparoscopic operations in gynecology now include a variety of surgeries previously done only by laparotomy such as the cure of uterine prolapse, simple or radical hysterectomy and pelvic or para-aortic lymphadenectomy [8], it remains mainly limited to tuboadnexal surgery in Cameroon. Raiga et al. have reported a series of 735 gynecological laparoscopic surgeries after five years of practice in Cameroun, most of which were indicted for tubal infertility [2]. In the same hospital, Kasia et al. have documented 194 tubal surgeries by laparoscopy with a pregnancy rate of 27.3% [3]. Afterwards, the laparoscopic surgical rate of tubal surgery of 91.3% has been reported in the same setting [4]. At the same time, advanced laparoscopic surgeries have only been documented by Belley Priso et al. in Douala and Kasia et al. in Yaoundé [5-6].
The Yaoundé Gyneco-Obstetric and Pediatric Hospital was created in 2002 and a study by Foumane et al. has stated a laparoscopic rate of 6.7% for the management of ectopic pregnancy [7]. Thus, little is known concerning the practice of laparoscopic surgery for tubal surgery in this hospital, especially when female infertility is suspected.
The objective of this study was to describe the practice of laparoscopic surgery in the management of female infertility at the Yaoundé Gyneco-Obstetric and Pediatric Hospital, Cameroon. This study would determine the role of tubal surgery for infertility in our surgical activity and provide data on surgical findings as well as complications observed.
2. METHODOLOGY
It was an observational study with a retrolective data collection, carried out at the Yaoundé Gyneco-Obstetric and Pediatric Hospital, Cameroon. After the authorization of the hospital authorities was obtained, all the female patients laparoscopically operated for infertility from January 1st 2004 to November 30th 2011 were included. Patients with incomplete files were excluded. The studied variables were: age, parity, type of infertility, hysterosalpingography results, operatory findings, operatory gestures, quality of the best tube accordingly to Mage’s tubal score [9], complications observed. Data were analyzed using Microsoft Excel 2007.
3. RESULTS
During the study period, 9194 gynecological surgeries were carried out at the Yaoundé Gyneco-Obstetric and Pediatric Hospital. Among these, 633 were done by laparoscopy, giving an endoscopic surgery rate of 6.9%. At the same time, 69.8% (442/633) of the laparoscopic operations performed were indicated for infertility. Twentyseven files were incomplete (27/442; 6.1%) and our analysis was done on the remaining 415 files (93.9%).
The mean age of our patients was 31.8 ± 4.9 years with a range from 17 to 47 years. Most of the women (349/415; 84.1%) were aged between 25 and 39 years. Nearly three quarters of the included patients were married (301/415; 72.5%), while 85.3% of them (354/415) had at least a secondary education level. Half of the operated women (209/415; 50.4%) had an income and 94.0% of them were living in an urban area (Table 1).
Even though 72.7% (202/415) of the infertile women have previously been pregnant in their life, only 37.6% (156/415) have experienced a delivery and 25.5% (106/ 415) have delivered once. Most of them (365/415; 87.9%) were pauciparous (Table 2). On the 415 recruited patients, 40 (9.6%) had a pelvic surgical history, ectopic pregnancy being encountered in 72.5% (29/40) of the cases (Figure 1).
Tubo-peritoneal adhesions were present in 71.6% (297/415) of the operated patients. Hydrosalpinx with distal tubal occlusion was encountered in 41.5% (172/ 415) of our patients while proximal tubal occlusion concerned 2.4% (10/415) of the cases. Tubal phimosis was described in 14.0% (58/415) cases. Peri-hepatic adhesions and fibroid were respectively discovered during
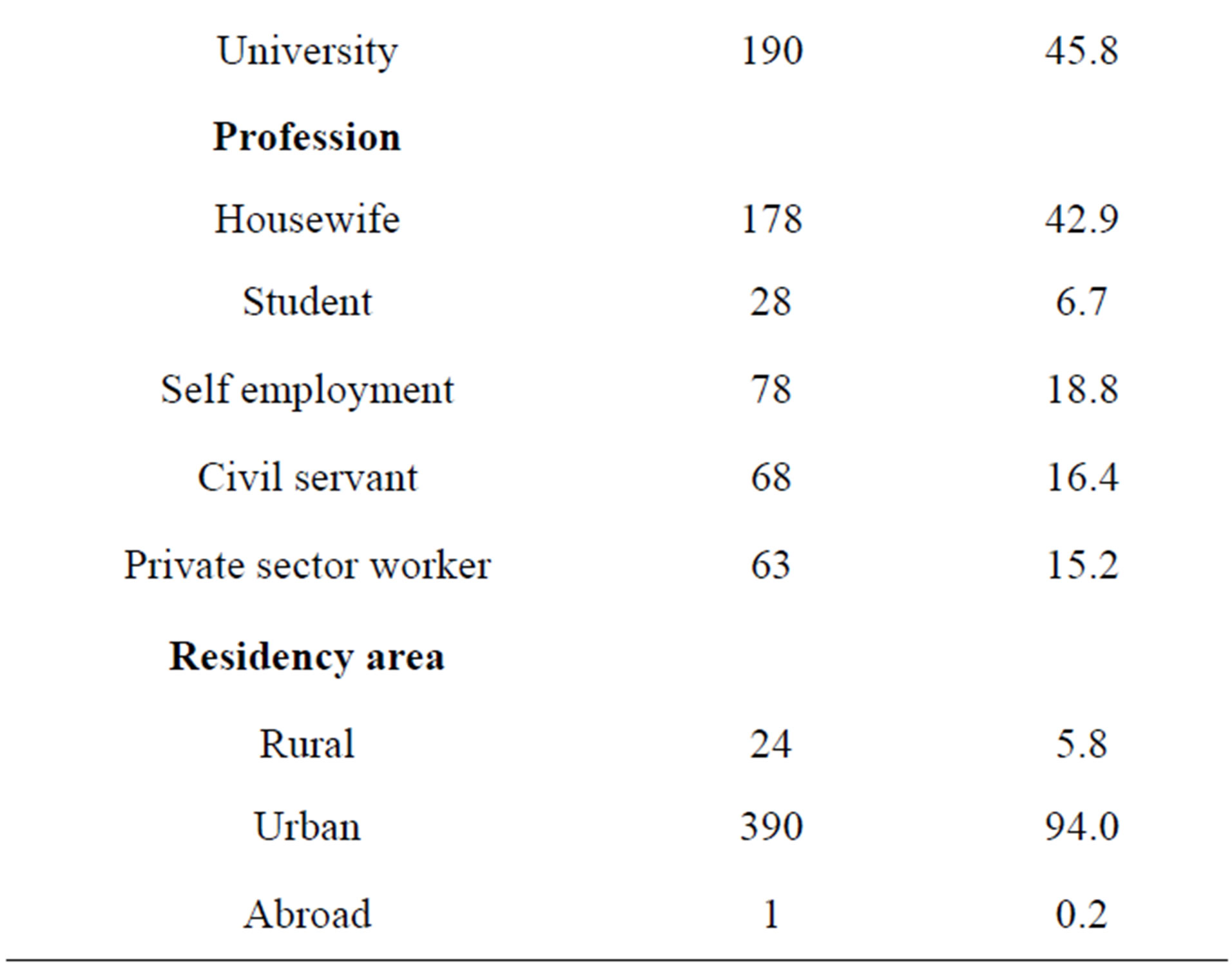
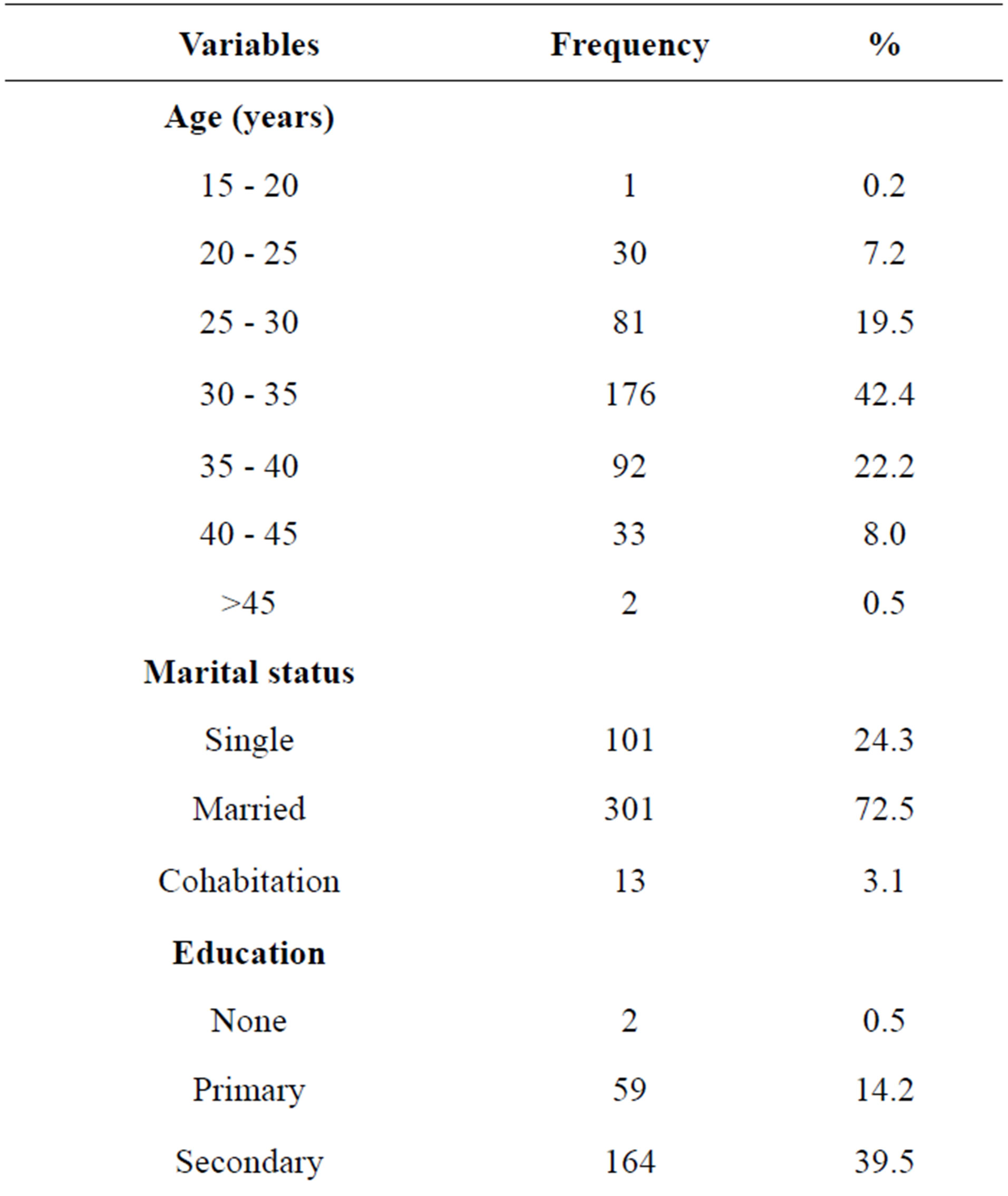
Table 1. Socio-demographic variables of women operated for infertility (n = 415).
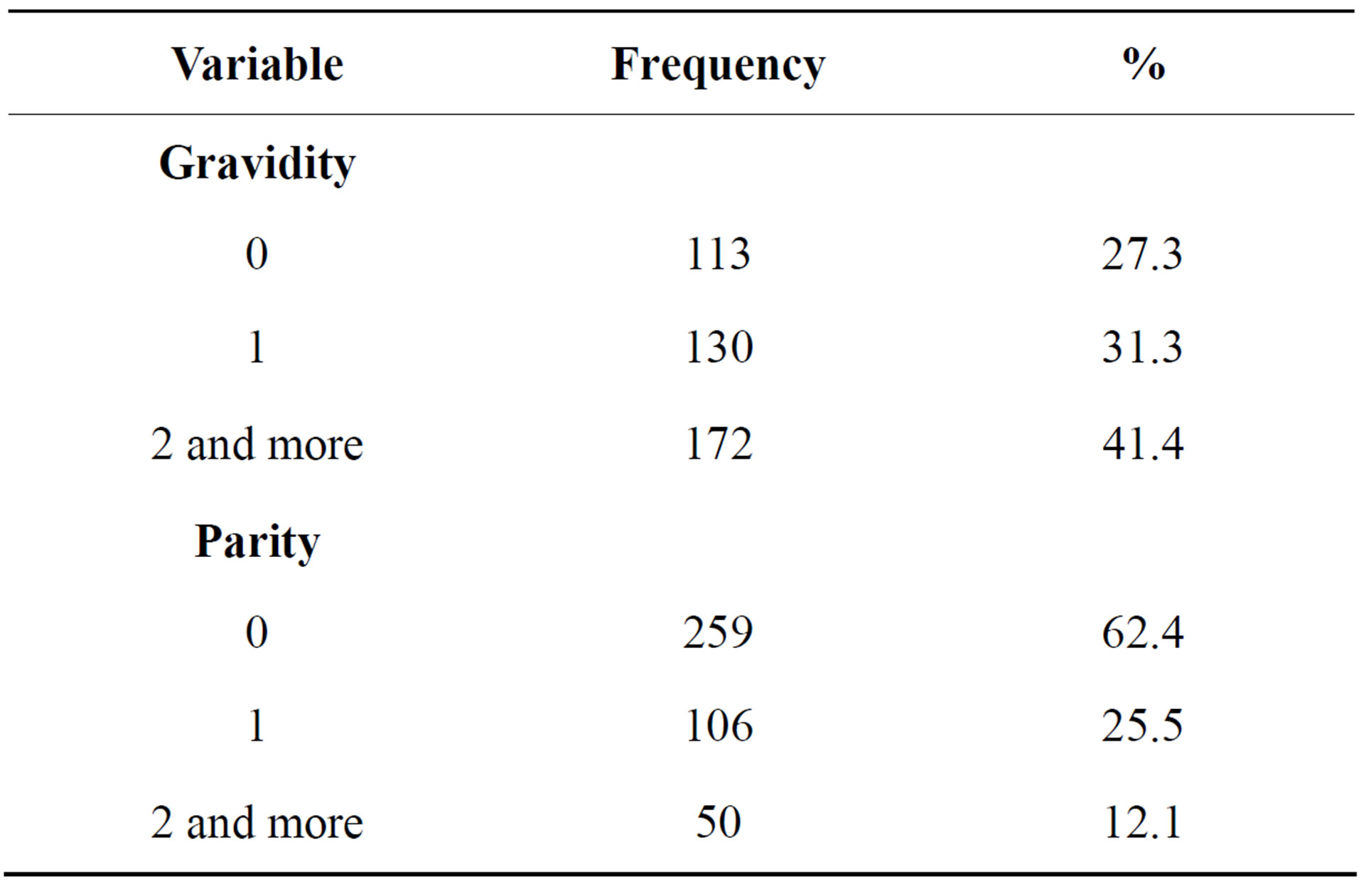
Table 2. Gravidity and parity of operated patients (n=415)
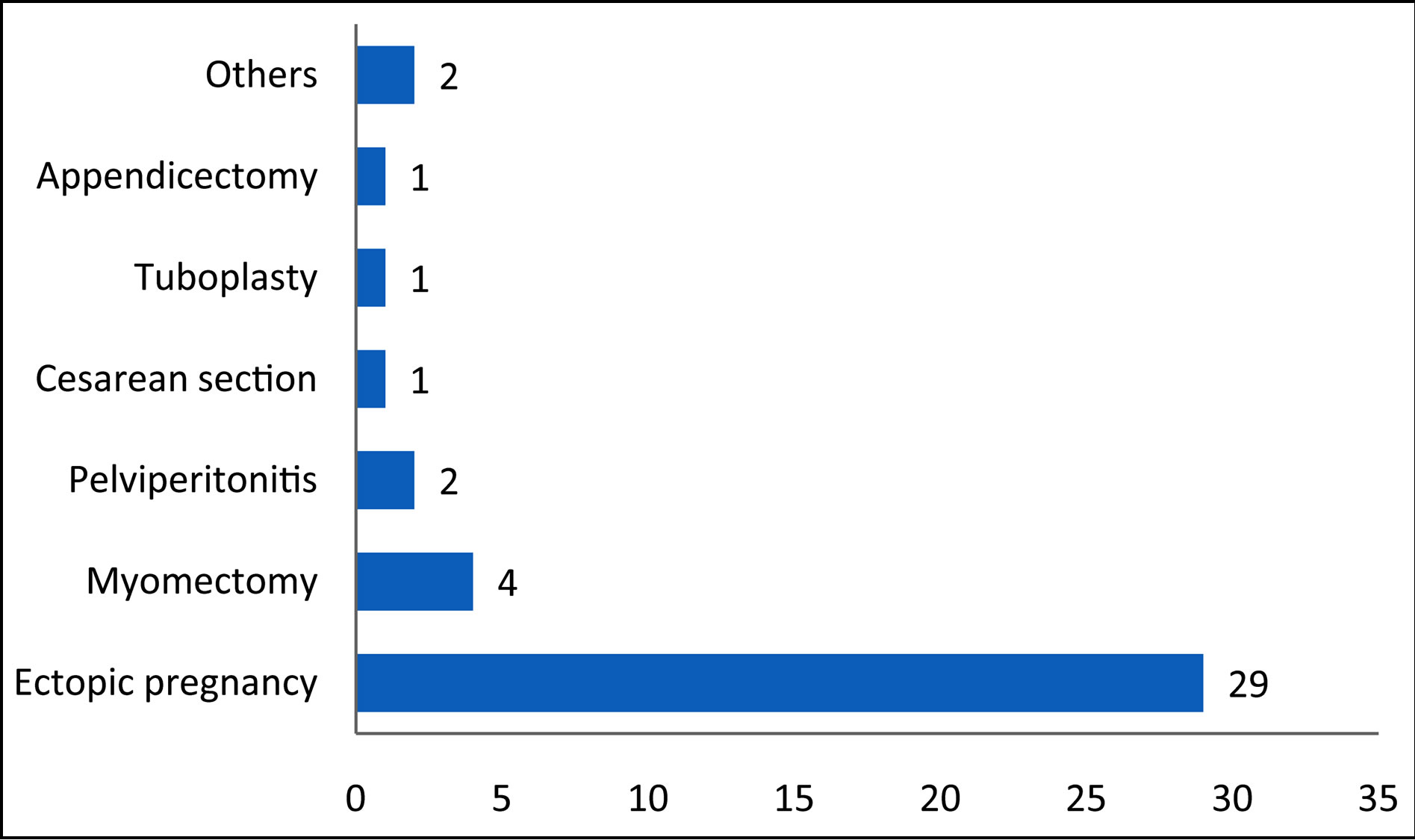
Figure 1. Past pelvic surgical events reported (n = 40).
laparoscopy in 22.4% (93/415) and 20.2% (84/415) of the patients (Table 3).
The commonest operatory gestures during laparoscopic surgery included adhesiolysis (297/415; 71.6%), neosalpingostomy with fimbriae eversion (172/415; 41.5) and fimbrioplasty (58/415; 14.0%). Tubal scores 1 and 2 were reported in 57.6% (239/415) patients, while 42.4% (176/415) of them had a tubal score 3 or 4 for the best tube at the end of surgery (Table 4).
According to the analyzed files, 18 patients (4.3%) presented operatory complications, the commonest described being uterine perforation (Table 5).
4. DISCUSSION
The 6.9% rate of endoscopic surgery in gynecology found in this setting remains below the figures published by well trained and equipped teams like that of Takacs et al. who reported a laparoscopically treatment rate of 86.3% for ectopic pregnancy since 2004 in Miami, USA [10]. This rate usually depends on socio-cultural, economic and structural conditions, explaining similar figures in similar settings. In the same department, a 6.7% rate of ectopic pregnancy management by laparoscopy has been reported [7]. Though a closer figure of 10% has been documented in the neighboring Gabon by Pither et al. [11], Sanogo et al. have published a surprising 19% rate of endoscopic surgery in Bamako [12], suggesting that the figures could be improved, even in a Sub-Saharan Africa setting.
Most of our laparoscopic surgeries are indicated for infertility (69.8%). This figure is similar to the 76.3% of laparoscopic operations for infertility reported in 2007 by Mboudou et al. at the Yaoundé General Hospital [13], and remains beyond the rates observed in western countries where the prevalence of pelvic infections is low and access to assisted reproduction therapy easier [14].
The sociodemographic characteristics of our patients are similar to those of infertile women reported in the same setting. We found a mean age of 31.8 years in our patients while Belley Priso et al. in the Douala General
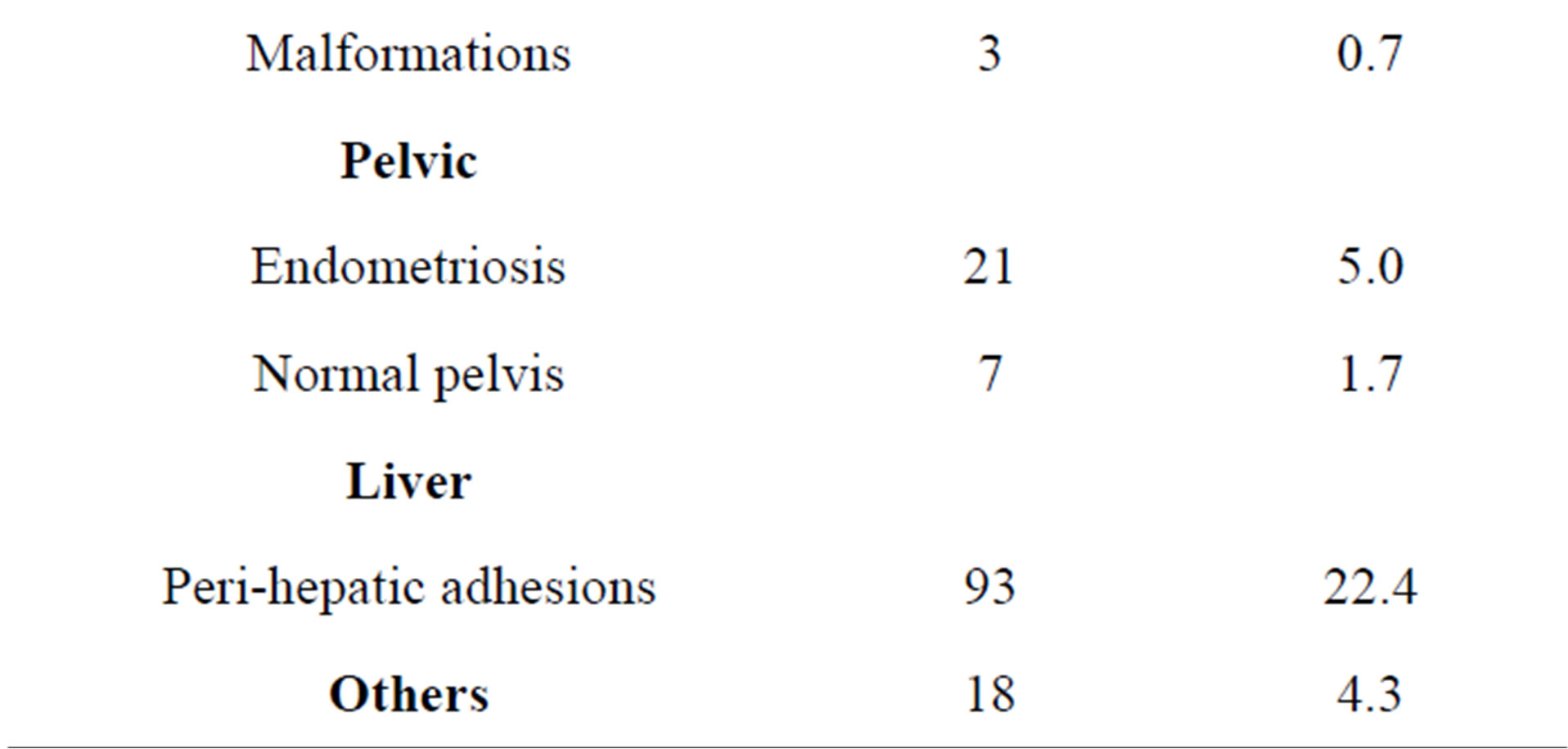
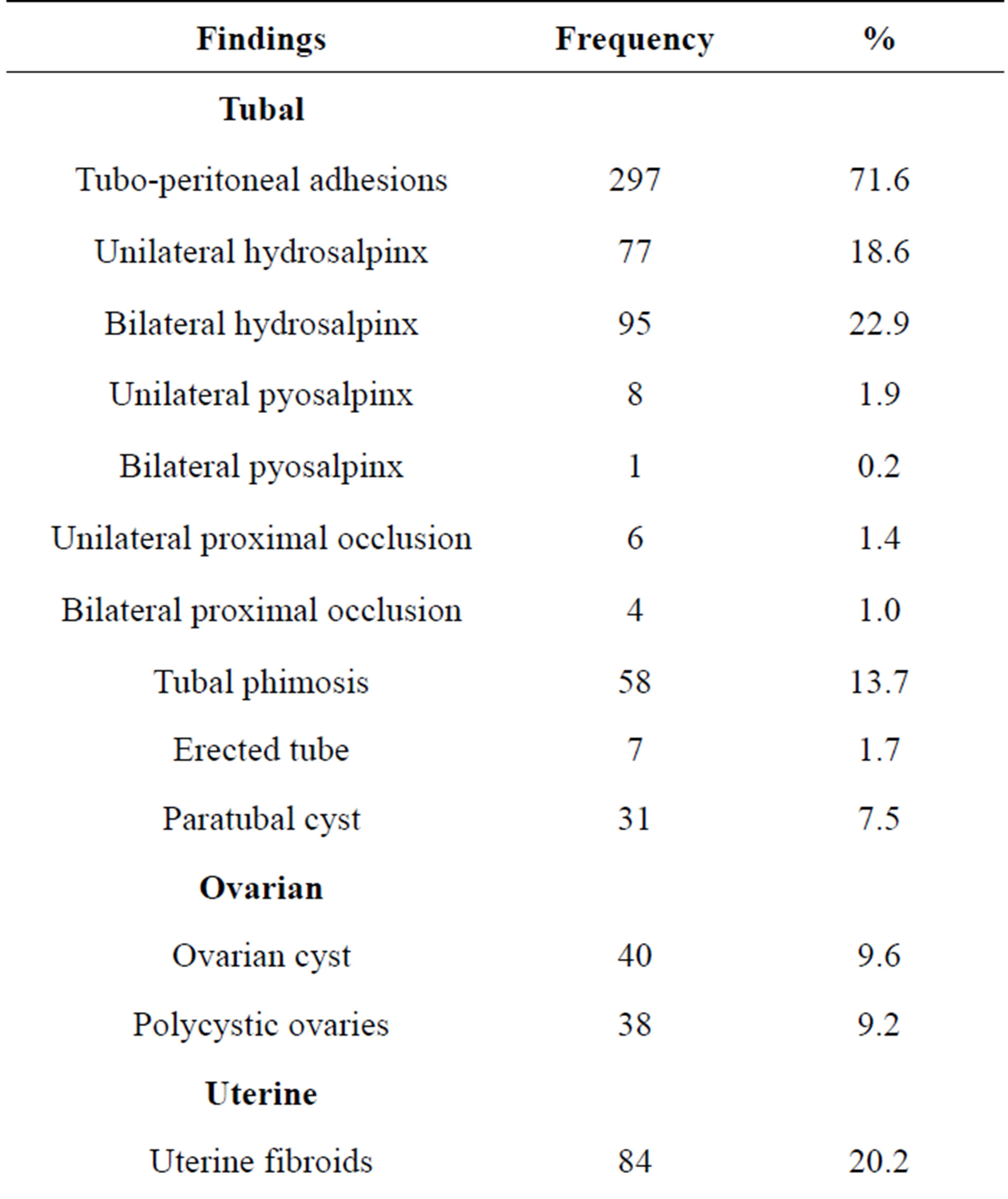
Table 3. Laparoscopic findings in operated patients (n = 415).
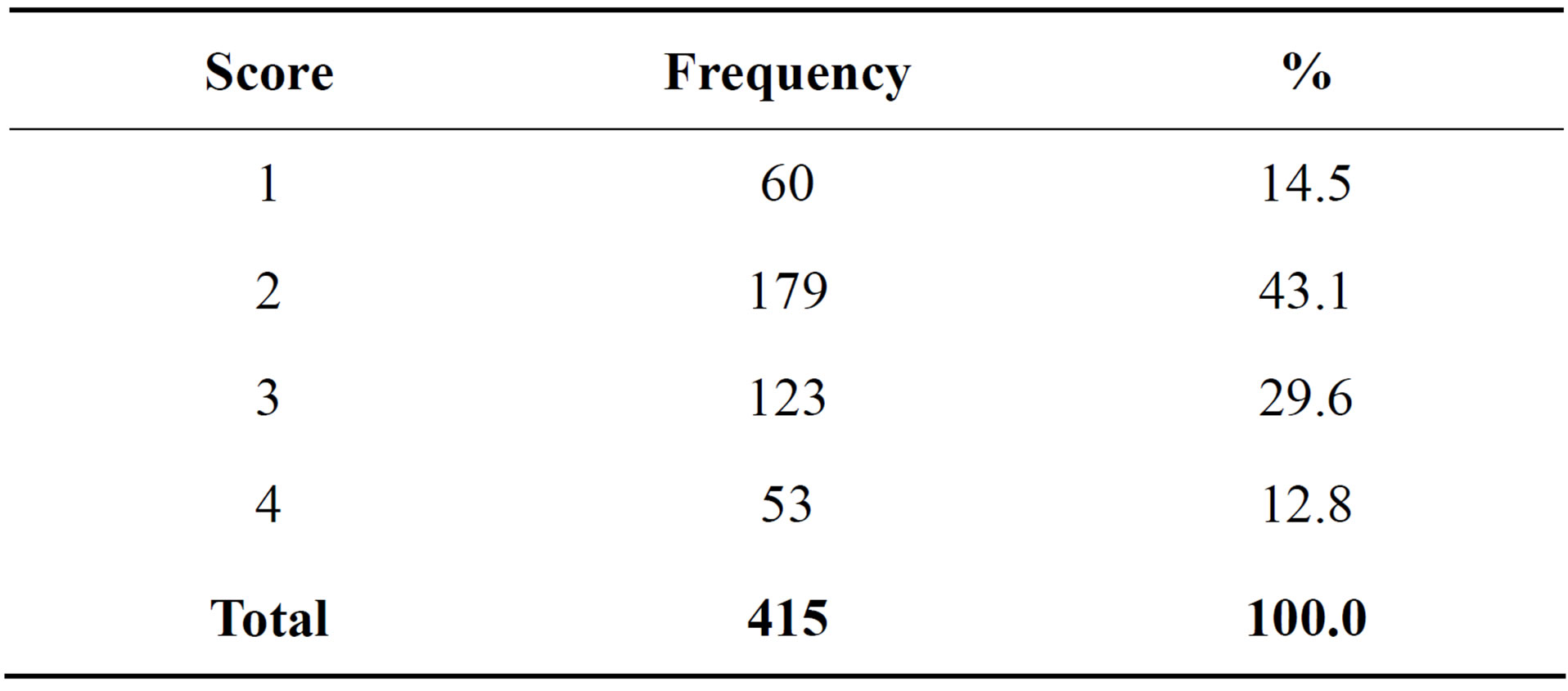
Table 4. Mage’s score of the best tube following surgery (n = 415).
Hospital [15] and Nana et al. in the Yaoundé Central Hospital [16] respectively published a mean age of 32 and 32.7 years. At the same time, 87.9% of the operated women in our series were pauciparous. This figure is similar to the 93.5% pauciparous women found by Mboudou et al. at the Yaoundé General Hospital [13].
Nearly three quarters of women with a pelvic surgical history had been operated for ectopic pregnancy. This is different from the findings of Nzintcheu et al. [17] who
Table 5. Complications observed following surgery (n = 415).
reported myomectomy as the commonest pelvic surgical past event encountered in infertile women undergoing laparoscopy. This difference can find an explanation in the fact that Nzintcheu et al. did a prolective data collection, while we collected our data retrolectively. A past history of myomectomy could be under-reported in the patients files. On the other hand, ectopic pregnancy and infertility share several risk factors and are commonly associated.
Tubo-peritoneal adhesions, hydrosalpinx, fibroids and peri-hepatic adhesions are the commonest laparoscopic findings in our series. The role of tubo-peritoneal adhesions and hydrosalpinx in female infertility is well documented [18,19]. Apart from pelvic infections due to Chlamydiae trachomatis and others pathogens [19], adhesions may arise following pelvic surgery or unsafe abortion which are common in our setting [15]. As well as pelvic adhesions, peri-hepatic adhesions result from pelvic inflammatory diseases. They have been found in 40% of infertile women in the same setting and their findings were correlated to the presence of severe tubal lesions [17].
According to the Mage's classification, the tubal score was favorable in 57.6% of our patients. This figure is not far from the 46.1% reported by Nzintcheu et al. in the same hospital in 2009 following a prolective data collection on 130 infertile women [17]. The scoring of the best tube at the end of laparoscopic surgery for infertility remains an important step in low-resource settings with low access to assisted reproductive therapy [3].
Our complications rate of 4.3% is beyond the rate found by Mboudou et al. at the Yaoundé General Hospital in a group of 609 patients operated by laparoscopy [13]. However, they faced a set of diversified indications, including two cases of laparoscopic hysterectomies.
Our results should be considered with some limitations inherent to a study with rétrolective data collection. Twenty-seven patients with incomplete files were excluded. At the same time, the collection of data such as complications could have been non exhaustive, serious complications tending to be more reported than minor. All these might have given some bias to our results.
5. CONCLUSIONS
Infertility is the main indication for laparoscopic surgery in our setting. The main operative findings are tuboperitoneal adhesions and hydrosalpinx. Ectopic pregnancy is the most common past pelvic surgical event reported. The most practiced surgical gestures are adhesiolysis, neosalpingostomy and fimbrioplasty. Half of the recruited women have a favorable stage for the best tube. The complication rate is low.
We recommend a strengthening of endoscopic surgical skills of the gynecologists engaged in the practice of laparoscopic surgery in advanced techniques, as well as the update of the available equipments at the Yaoundé Gyneco-Obstetric and Pediatric Hospital.
NOTES