Morphological Measurements of Knee Joints in Indian Population: Comparison to Current Knee Prostheses ()
1. Introduction
The principal factors on which the long life and successful outcome of a total knee arthroplasty (TKA) implant depend are optimum bone resection and maximum coverage of the resected bone [1] [2] . These factors rely heavily on the size matching of the implant with the resected knee. Commercially available TKA implants do not cater to anthropometric differences observed across different ethnicities, as suggested by some recent studies [3] -[5] . Most of the existing commercial implants are designed to suit the knee anatomy of the Western population. Studies have shown that the smaller build and stature of the Asian-Pacific population gives rise to geometric mismatch between patient anatomy and implant components [6] . At present, owing to a shortage of data on the distal femur and proximal tibia in this population, implants designed for knees of the Western population are being used without modifications for the ethnic group [7] . Anthropometric studies have shown that there are striking variations in knee morphology between the Asian and Western population [8] . Research on implant mismatching carried out in various Asian countries has led to the conclusion that the Asian-Pacific population should have special designs of TKA implants [9] . It has become essential to compare the resected knees of the subject population with the existing Western implants and quantify the morphological differences so as to improve the performance of TKA. The aim of the present study is to investigate the morphology of the Indian arthritic knees using three dimensional knee models and evaluate them against commercially available TKA implants. We hypothesize that a distinct difference in size and shape between the Indian knees and Western knees leads to mismatch of sizes of Western TKA implants in Indian patients.
2. Materials and Methods
2.1. Subjects
66 knee joints from living subjects were analyzed in this study. These subjects were patients suffering from bilateral primary osteoarthritis undergoing TKA. The knee joint data included fourteen male knees and fifty-two female knees. This data was collected preoperatively using Computed Tomography (CT) imaging. Patients having other periarticular pathologies such as tumours, rheumatoid arthritis and post-traumatic fracture were excluded from this study. Since both knees of all patients were affected by osteoarthritis, both left and right knees were included in the database.
2.2. CT Scan Technique
For all subjects, a CT scan of the knee was obtained using a helical CT scanner (130 kV, 53 mA; Samsung Healthcare). The patients were informed about the procedure and a written approval was taken from them for the purpose of statistical study. During the scan, it was ensured that the subjects were supine with the knees in relaxed and extended position. This scanning procedure was performed to acquire CT slices of thickness 0.5mm with a resolution of 512 × 512 pixels. The raw data obtained from the scans was first copied in DICOM file format and then exported to a medical modelling software (Mimics 10.1, Materialise, Belgium). The images were segmented to construct 3D bone models of the knee. The approach mentioned above was similar to those reported in literature [3] . The 3D models of the knee were exported as a point cloud data to a CAD environment (SolidWorks 2008, Dassault Sys., USA), converted to a surface mesh and eventually knit to form solid models. Surgical resections were performed on these bone models, followed by measurements on resulting resected bones.
2.3. Surgical Procedure
In order to accurately quantify the difference between Indian arthritic knees and commercially available TKA implants, a resection study was performed by simulating the surgical procedure on the solid models of the knee. Conventional surgical cuts performed on the knee during the TKA surgery were virtually simulated.
Once the 3D model of the femur was obtained, the distal surgical cut was virtually performed on the femur [10] . The anatomical axis of the femur was defined as the line connecting the centre of the intramedullary canal at the proximal end and the centre point of the transepicondyleintrocession. The femur was oriented in the frontal plane with 60 valgus (angle between anatomical axis and mechanical axis). A transverse plane passing through the distal extremity of the medial condyle was drawn. Following the conventional surgical procedure, the distal femur was resected parallel to the transverse plane at 9 mm above the lower extremity (Figure 1(a)).
Once the 3D model of the tibia was obtained, the proximal surgical cut was virtually performed on the tibia [10] . The tibia was oriented in the sagittal plane. A transverse plane passing through the medial aspect of the tibial plateau was constructed perpendicular to the tibial mechanical axis. A reference plane was constructed with a 70 posterior slope. Following the conventional surgical procedure, the proximal tibia was resected parallel to the reference plane at 6 mm below the medial aspect of the tibial plateau (Figure 1(b)).

Figure 1. Virtual surgical resections (a) Distal femur (b) Proximal tibia.
2.4. Measurements
The resected femur was oriented perpendicular to the transverse plane and all measurements were performed on this distal resection plane (Figure 2(a)). The mediolateral axis was taken as the transepicondylar axis (TEA), a line connecting the lateral epicondylar prominence and the medial epicondylar prominence. Tangents parallel to the TEA and passing through the anterior and posterior extremities were constructed. Distance between two medial and lateral extremities in the resected plane measured collinear to the TEA was defined as the femoral Mediolateral width (fML). Distance between two tangents parallel to TEA and passing through anterior and posterior extremities of distal femur was defined as the femoral Anteroposterior width (fAP).
The resected tibia was oriented perpendicular to the transverse plane and all measurements were performed on this proximal resection plane (Figure 2(b)). The mediolateral axis was constructed parallel to the femoral TEA. Tangents parallel to the TEA and passing through the anterior and posterior extremities were constructed. Distance between medial and lateral extremities in the resected plane measured parallel to the mediolateral axis was defined as tibialMediolateral width (tML). Distance between two tangents parallel to TEA and passing through anterior and posterior extremities of proximal tibia was defined as tibialAnteroposterior width (tAP).
2.5. Implant Selection Procedure
Based on the guidance and feedback of surgeons, a fixed implant selection procedure was decided which was commonly followed by knee arthroplasty surgeons for conventional implants. As mentioned in literature, clinical consequences of overhangs in TKA are disastrous [11] . Hence, the first priority and the most important criterion in selecting a suitable implant, either for femur or tibia, is that there should be no overhangs in any dimension.
In case of the femoral component, the fML is the deciding dimension i.e. the size of the implant is selected such that the ML dimension of the implant closely matches to that of the subject but is less than or equal to the fML of the subject. This is done to ensure no overhangs in ML dimension.
In case of the tibial component, the size of the implant is selected such that the ML dimension of the implant closely matches to that of the subject but is less than or equal to the tML of the subject. Thus, any possible overhang in ML dimension is prevented. However, while doing so, if there is an overhang in AP dimension, then the size of the implant is selected such that the AP dimension of the implant closely matches to that of the subject but is less than or equal to the tAP of the subject. Thus, overhang is prevented in the AP dimension, although a compromised underhang occurs in ML dimension.
2.6. Statistical Analysis
In the statistical analysis, best-fit lines were calculated with use of least squares regression method. The data was summarized as the mean and standard deviation (mean ± SD). Data analysis of the Indian knees was performed by using the Student t-test. Welch’s t-test was used to compare data with dissimilar number of population samples. Values for p < 0.05 were regarded as statistically significant.
3. Results
The average age for males was greater than the average age of females (73.6 ± 8.4 years, range 64 - 82 years for
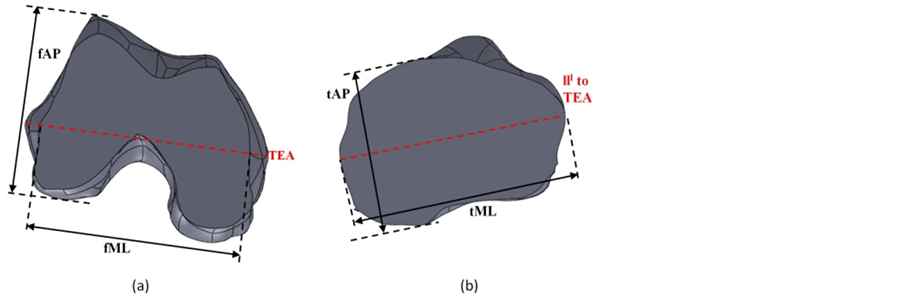
Figure 2. Measurements performed on resected planes (a) Distal femur (b) Proximal tibia.
males vs. 66.2 ± 8.2 years, range 52 - 80 years for females, p = 0.07).
3.1. Analysis of Indian Knee
Average femoral mediolateral length (fML) was 68.3 ± 3.9 mm and average femoral anteroposterior length (fAP) was 62.7 ± 4.8 mm. Average femoral aspect ratio (fML/fAP) was 1.09 ± 0.05. Males had larger values of fML and fAP as compared to females (p < 0.01).
A positive correlation was observed between fAP and fML for both males and females. In case of the femoral aspect ratio (fR), no statistically significant difference was found between males and females (p = 0.998). Femoral measurements for the Indian population have been compared across genders in Table 1.
The average tibial mediolateral length (tML) was 73.8 ± 4.7 mm and average tibialanteroposterior length was 51.2 ± 4.3 mm. The average tibial aspect ratio (tML/tAP) was 1.45 ± 0.08. Males had larger values of tML and tAP as compared to females (p < 0.01). A positive correlation was observed between tAP and tML for both the genders. In case of the tibial aspect ratio (tR), no statistically significant difference was found between males and females (p = 0.588). Tibial measurements for the Indian population have been compared across genders in Table 1.
3.2. Comparison across Ethnicities
To compare the Indian knees morphologically with other ethnic groups, the anthropometric measurements of knees of various ethnicities were retrieved from literature. The aspect ratios were defined as mentioned above in order to make our data coherent with the anthropometric data of other ethnic groups. The data of the distal femur of Indian population was compared with that of Chinese, Caucasian, Japanese, Korean and American population as shown in Table 2. The data of the proximal tibia of the Indian population was compared to that of Chinese, Japanese, Korean and American population as shown in Table 3.
3.3. Comparison with Conventional Implants
The Indian knees were compared to the following commercially available conventional implants – JOURNEY Knee (Smith & Nephew, London), PFC Sigma Knee System (DePuy, NJ, USA), ADVANCE Knee System (Wright Medical Technology Inc., TN, USA), Triathlon Total Knee (Stryker Corp., MI, USA), NexGen LPS Flex Mobile Knee System (Zimmer Holdings, IN, USA) and Scorpio NRG Knee System (Stryker Corp., MI, USA).
In case of the femoral components, the various implant sizes covered the entire range of the Indian population (Figure 3(a)). However, implants with smaller fAP were undersized in fML and those with larger fAP showed overhang in fML i.e. the slope of the implant sizes and Indian population was different. This was clearly seen in the graph of femoral aspect ratio (fR = fML/fAP) vs. fAP (Figure 3(c)). The fR of the Indian population showed a decreasing trend with increase in fAP; however, implants had an almost constant fR.
In case of the tibial components, the various implant sizes covered the entire range of the Indian population

Table 1. Average values of the Indian femur and tibia morphology measurement.
a. The p-values are calculated for comparison across genders.

Table 2. Summary of the measurements of distal femur across various ethnic groups.
a. Data presented as mean ± SD in mm. Abbr.—fML: femoral mediolateral, fAP: femoral anteroposterior, fR: femoral aspect ratio.
(Figure 3(b)). However, as observed for femoral components, the slope of the implant sizes and Indian population was different—implants with smaller tAP were undersized intML and those with larger tAP showed overhang in tML. The graph of tibial aspect ratio (tR = tML/tAP) vs. tAP (Figure 3(c)) clearly displayed the above result. Although the tR of the Indian population had a decreasing trend with increasing fAP, implants had an almost constant tR.
3.4. Errors in Optimally Selected Implants
Although the graphs of ML vs. AP, for both femur and tibia, suggested that Western implants covered the demographic population, the mismatch of foreign implants on Indian knees needed to be closely observed. To correctly quantify implant errors, every patient’s femur and tibia was virtually fitted with an optimal implant component of each implant manufacturer, according to the procedure mentioned previously.

Table 3. Summary of the measurements of proximal tibia across various ethnic groups.
a. Data presented as mean ± SD. Units in mm. Abbr.—tML: tibial mediolateral, tAP: tibialanteroposterior, tR: tibial aspect ratio.

Figure 3. Comparison with conventional implants (a) fML vs. fAP (b) tML vs. tAP (c) fMLfAP vs. fAP (d) tMLtAP vs. tAP.
In case of the femur, fML being the deciding dimension, errors in this dimension were minimized by selecting an optimal implant size. Thus, the overhangs in this dimension were negligible; however, due to fixed sizes of implants, underhangs up to 5 mm were observed (Figure 4(a)). When these optimal implants were checked for the fAP dimension, overhangs upto 5 mm were observed; moreover, underhangs reached high errors of upto 12 mm (Figure 4(b)). The graph of femoral aspect ratio (Figure 4(c)) revealed that errors were largely positive for smaller fR and negative for larger fR (> 10% relative error).
In case of the tibia, the selection criterion only involved minimizing overhangs i.e. any one of tML and tAP could be the deciding dimension. Hence, two sets of studies were analyzed—one with tML as the deciding dimension and the other with tAP as the deciding dimension.
In the first case, with tML being the deciding dimension, errors in this dimension were minimized by selecting an optimal implant size. Thus, it was ensured that there are no overhangs in this dimension; however, due to fixed sizes of implants, underhangs up to 7 mm were observed (Figure 5(a)). When these optimal implants were checked for the tAP dimension, overhangs up to 5 mm were observed; moreover, underhangs reached high errors of up to 12 mm (Figure 5(b)). The graph of tibial aspect ratio (Figure 5(c)) revealed that errors were largely positive for smaller tR and negative for larger tR (> 10% relative error).
In the second case, with tAP being the deciding dimension, errors in this dimension were minimized by selecting an optimal implant size. Thus, overhangs in this dimension were negligible; however, due to fixed sizes of implants, underhangs up to 4 mm were observed (Figure 6(a)). When these optimal implants were checked for the tML dimension, underhangs up to 13 mm were observed; moreover, overhangs reached high errors of upto 21 mm (Figure 6(b)). The graph of tibial aspect ratio (Figure 6(c)) revealed that errors were largely positive for smaller tR and negative for larger tR (> 10% relative error).
4. Discussion
Total knee replacement, being a precise surgical procedure, shape match between the prosthesis and the resected surface of the knee is a vital factor for long-term success [2] . According to various research studies, Asian knees are generally smaller than the Western population [3] -[5] [8] [12] . Moreover, a study has also demonstrated that Asian knees have a smaller aspect ratio than those of the Western population [8] . Since components of the knee

Figure 4. Error in optimally selected femoral components (a) fML error (b) fAP error (c) fR error.

Figure 5. Error in optimal tibial components selected with ML dimension as base (a) Error in tML (b) Error in tAP (c) Error in tR.

Figure 6. Error in optimal tibial components selected with AP dimension as base (a) Error in tAP (b) Error in tML (c) Error in tR.
implants are required to cover maximum resected surface in order to achieve a successful outcome [2] [3] , it is important to know the exact morphology of the resected surface of the Indian knees in order to design or validate knee prostheses for the Indian population. This study used a 3D CT image technique for morphological measurements of the tibia and femur in an Indian population. The measurements from the CT images strongly correlate to intraoperative measurements since the 3D CT image of the knee can undergo unconstrained rotation and the correct three dimensional axis can be determined and maintained [13] . Moreover, in this study, instead of solid unresected bones, measurements were performed on the resected planes of the femur and tibia so as to directly compare the corresponding dimensions with the implants at the surface where they would be implanted on the patients.
Morphological measurements of the ML and AP dimensions revealed that the Indian female has a smaller femur and tibia than the Indian male, and both have smaller values than the Western population. Probably owing to differences in the imaging technique, some minor differences between other Asian populations were also observed.
The Indian knees were compared to Western implants which were commonly available in the Indian market and used by surgeons for TKA of Indian patients. The femoral data of the Indian population showed a decreasing aspect ratio (fML/fAP) as the fAP dimension increased. In case of the Indian tibia, the aspect ratio (tML/tAP) decreased as the tAP increased. In contrast to these observations in the aspect ratios of Indian patients, variations in aspect ratios of most implants were insignificant. For both the femur and tibia, it was found that the ML dimension was undersized with smaller AP and overhang was observed for larger AP dimensions. Thus our results suggest that Western implants, although suitable for the Western population, may not be suitable for Indian patients. To quantify the mismatch of the above mentioned foreign implants, error extremities signifying overhangs and underhangs were exploited.
A radiographic and cadaveric study, that evaluated sizing for knee prostheses, supported the idea that the required femoral designs component size should be based on the ML dimension of the femoral condyle [14] . When optimal implant sizes were chosen according to fML, there were large overhangs and underhangs observed especially in fAP. In case of the femur, overhang in fAP would not only adversely affect the surrounding soft tissues but it would also lead to pain in the patellar tendon during deep flexion. Underhang in fAP was also undesirable because a negative error would mean greater bone resection and loss of healthy bone. Moreover, any error in fAP, be it positive or negative, would alter the natural biomechanics of the knee. In case of the tibia, optimal implant sizes were chosen according to both the dimensions—first tML and then tAP. When optimal sizes were selected based on one of the two dimensions, large overhangs and underhangs were observed in the other dimension. Overhang in any dimension would mean interference with the adjacent soft tissues thus leading to pain and host-tissue reactions. On the other hand, underhang in case of the tibia would imply insufficient cortical bone coverage between the implant and the bone thus leading to stress shielding in some parts of the proximal tibia. Large errors in femoral and tibial aspect ratios were observed since Western implants had a somewhat constant aspect ratio while the aspect ratio of the Indian patients decreased with increasing AP dimension. These errors indicated that the implant sizes should accommodate change in aspect ratios along with the usual ML and AP dimensions.
One of the limitations of our analysis is the lack of morphologic data of healthy, non-arthritic knees. In this study, we chose osteoarthritic knees to study and compare the morphology of Indian knee with other ethnicities and foreign implants. However, for the Indian population, whether prosthesis should be designed according to the normal or osteoarthritic knee morphology needs further research. Moreover, we measured only one resected surface in the tibia and femur in this study since it involved comparison with conventional implants; however, in recent clinical procedures, the depth of the cut surface is determined according to the stage of the osteoarthritis present [3] .
5. Conclusion
Our study establishes that Western implants may have drawbacks when implanted in Indian patients. Moreover, this study provides definite rationale for designing total knee prosthesis, especially a gender-specific design suitable for the Indian population. This study clearly shows that while designing the prostheses, the relationship between aspect ratio and anteroposterior dimension of the tibia and femur should also be taken into account apart from the relationships between mediolateral and anteroposterior dimensions.
Acknowledgements
This work has been carried out at the OrthoCAD Lab set up with funding by the Office of the Principal Scientific Advisor to the Government of India, New Delhi. The extensive support, including CT imaging and data provided by the Department of Orthopaedics at Hiranandani Hospital, Mumbai is gratefully acknowledged.