Mothers’ and health workers’ perceptions of participation in a child-friendly health initiative in rural South Africa ()
1. INTRODUCTION
In South Africa HIV care is commonly delivered in primary health care clinics (PHCs) where health workers are instrumental in supporting good adherence to antiretroviral treatment (ART) [1]. In the family context HIV-uninfected children often play an important role in supporting their HIV-infected parents, including helping them to adhere to their medication [2-5]. Therefore, increasing children’s access to health care support networks has the potential to improve health outcomes in families.
However, PHCs are often not perceived as childfriendly spaces [6,7]. Barriers reported to lower childfriendliness includes inappropriate physical structures and job dissatisfaction or fatigue amongst health workers [8,9]. Facilitators include staff training on child-friendliness and engaging children with toys and activities [10,11]. In resource-poor settings PHCs are often overburdened, so health promotion is a low priority [12-14]. A multi-site study in Uganda, Kosovo and Pakistan found that children, parents and health workers shared frustrations with rigid health care structures and poor systems for disseminating health information [6]. Even in resource-rich settings health workers acknowledge the challenges of promoting health amongst children in primary health care [6,15].
Despite being home to most of the world’s families living with HIV, literature addressing the health care support needed by HIV-affected families in South and southern Africa is minimal [3,12,16-18]. Most has focused on the utilization of health services by sick people [13,14,17,19,20] and suggests that children are often marginalised as they find health care facilities frightening [21,22] and do not understand the terminology being used [23,24].
A family-centred HIV disclosure intervention, the “Amagugu intervention” [25], was developed and tested in rural South Africa to support HIV-infected mothers to disclose their HIV status to their 6 - 10-year-old, HIVuninfected, children. The intervention was tested with 281 families and found to increase maternal HIV disclosure [25]. After disclosure the mother was encouraged to engage in a health promotion activity by taking her child with her to a clinic visit. The mothers were educated on the importance of early health promotion for children and provided with health education tools for use at the clinic visit. In addition, an intervention to support childfriendliness at the nine participating health facilities was developed and implemented. This research used qualitative and quantitative methodology to explore health workers’ perceptions of delivering child-friendly services and presents maternal data to support improvements in child-friendliness as a result of this intervention.
2. METHODS
The research setting: This study was undertaken at the Africa Centre for Health and Population Studies (www.africacentre.com) in northern KwaZulu-Natal, South Africa, in a predominantly rural area with a high HIV prevalence [1,26]. Health care, including HIV care, is delivered through 17 PHCs and one district hospital with a comprehensive, decentralised, HIV Treatment and Care Programme [13,27,28].
Research design: This research used both quantitative rating data from structured questionnaires administered to mothers, and qualitative data from focus groups with health workers and in-depth interviews with a sub-group of mothers. Mixed methodology was chosen because of its value in understanding health behaviours and perceptions in under-researched issues and populations [29,30].
Health care initiative: A health facility intervention was developed specifically for this research, using participatory qualitative techniques to increase its relevance and acceptability for health staff. Thereafter, the training was piloted at four of the nine implementation clinics, selected to include both rural and peri-urban settings. During piloting, dialogue and feedback were elicited from staff at participating clinics to finalise the training programme and clinic resources for a child-friendliness component (see Box 1). The training was then implemented at the five remaining PHCs. The health worker training targeted a diversity of staff including nurses, HIV counsellors and clerks to maximise opportunities for improving the quality of interactions with children during clinic visits.
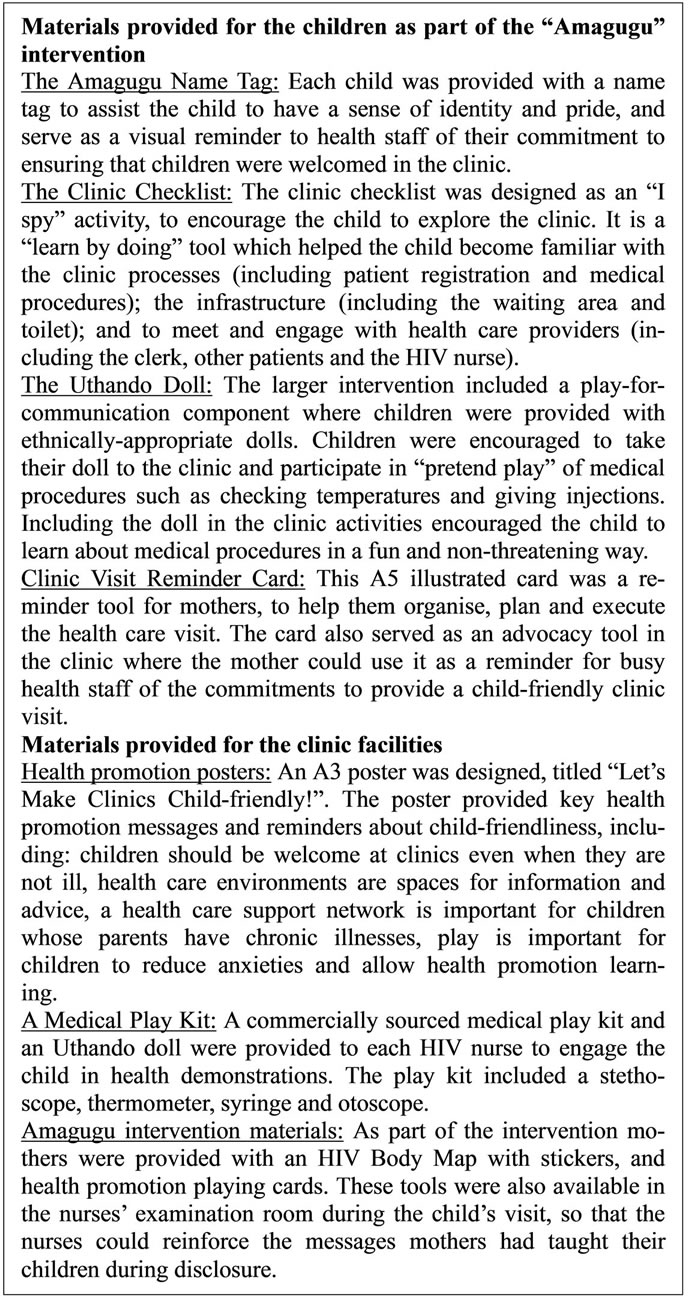
Box 1. Health care educational materials provided as part of the Amagugu intervention.
Data collection tools: Three data collection tools were utilized in this research: 1) Interviews with mothers (N = 281): These structured interviews followed the health promotion clinic visit and collected maternal ratings of child-friendliness; 2) In-depth interviews with a sub-set of mothers (N = 20): A group of mothers were interviewed at their homes two weeks after the Amagugu intervention, to explore their experiences of participating; 3) Health care worker focus groups (N = 87): Focus groups were conducted with health staff at all nine participating clinics, three months after the intervention. Focus group methodology was used to explore perceptions, opinions and attitudes towards child-friendliness. Prior to the research we identified five key issues from the literature [10-12,19-21,31-33] which were important for the development and uptake of this kind of intervention: 1) willingness to engage in child-friendliness; 2) activities to support child-friendliness; 3) barriers and 4) facilitators of child-friendliness; and 5) contributors to sustainability. These formed the basis of the focus group guide and were also used as guiding categories in focus group analyses.
Data analysis: Quantitative data analysis: Mothers’ data from the post clinic interviews were entered into an Access database and imported into STATA 11 for analysis. Descriptive statistics were used to quantify and describe the demographic characteristics of the participants including mothers and health workers. Qualitative data analysis: Focus groups and in-depth interviews were transcribed verbatim, translated from IsiZulu to English, imported into ATLAS. ti version 7 for analysis [34,35], and organised using the themes explored in the focus group and interview guides. Categories were reviewed for redundancy and similar codes and categories grouped under a single higher order category. Higher order categories which resulted from collapsing codes with similar ideas together reflected the important thematic areas linked to the focus group and interview guide categories.
Ethics permissions: Approval was granted by the University of KwaZulu-Natal Biomedical Research Ethics and the University of Witwatersrand Human Research Ethics Committees.
3. RESULTS
Sample: All 281 HIV-positive mothers enrolled in Amagugu completed the health promotion training; their socio-demographic and health characteristics are shown in Table 1.
Maternal intervention impact: Mothers’ experiences of the clinic visit, including ratings of child-friendliness of health workers are shown in Table 2. Almost all the mothers took their child to the clinic, with a third reporting waiting less than 5 minutes to see the nurse. Approximately two-thirds of the mothers rated the clerks and nurses as “very friendly”, and most reported that the nurses had used the medical play kits and the childfriendliness posters, although only a third used the HIV Body Map.
Characteristics of health workers participating in focus groups N = 87: Forty-one (47%) participants were nurses, 23 (26.5%) HIV counsellors and 23 (26.5%) clinic clerks. The median age of participants was 39 years (IQR 31 - 49); six were male. Sixty two (71%) participants were from rural, 17 (20%) from peri-urban and 8 (9%) from urban clinics.
Themes from the focus groups of health workers and in-depth interviews of mothers:
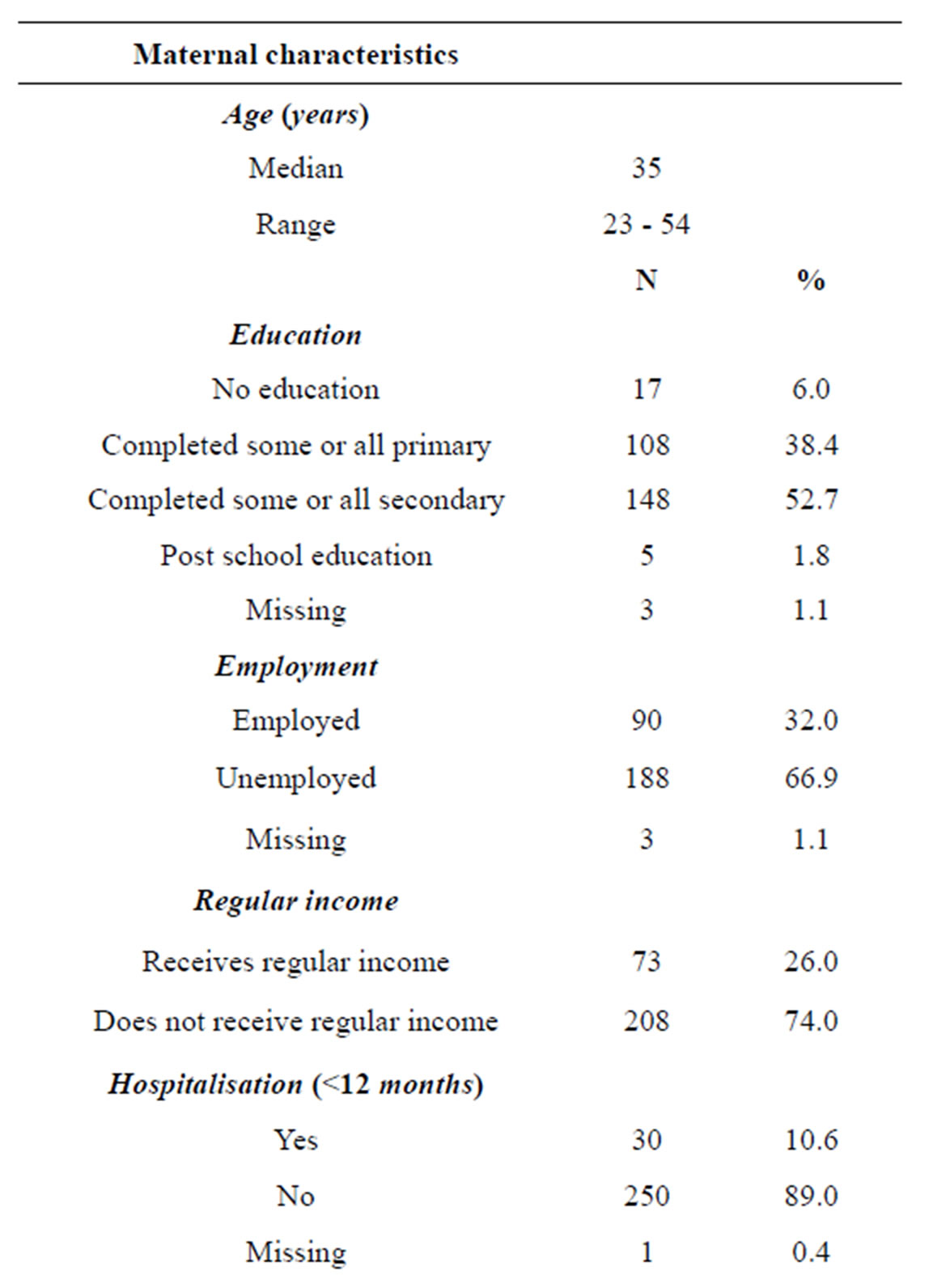
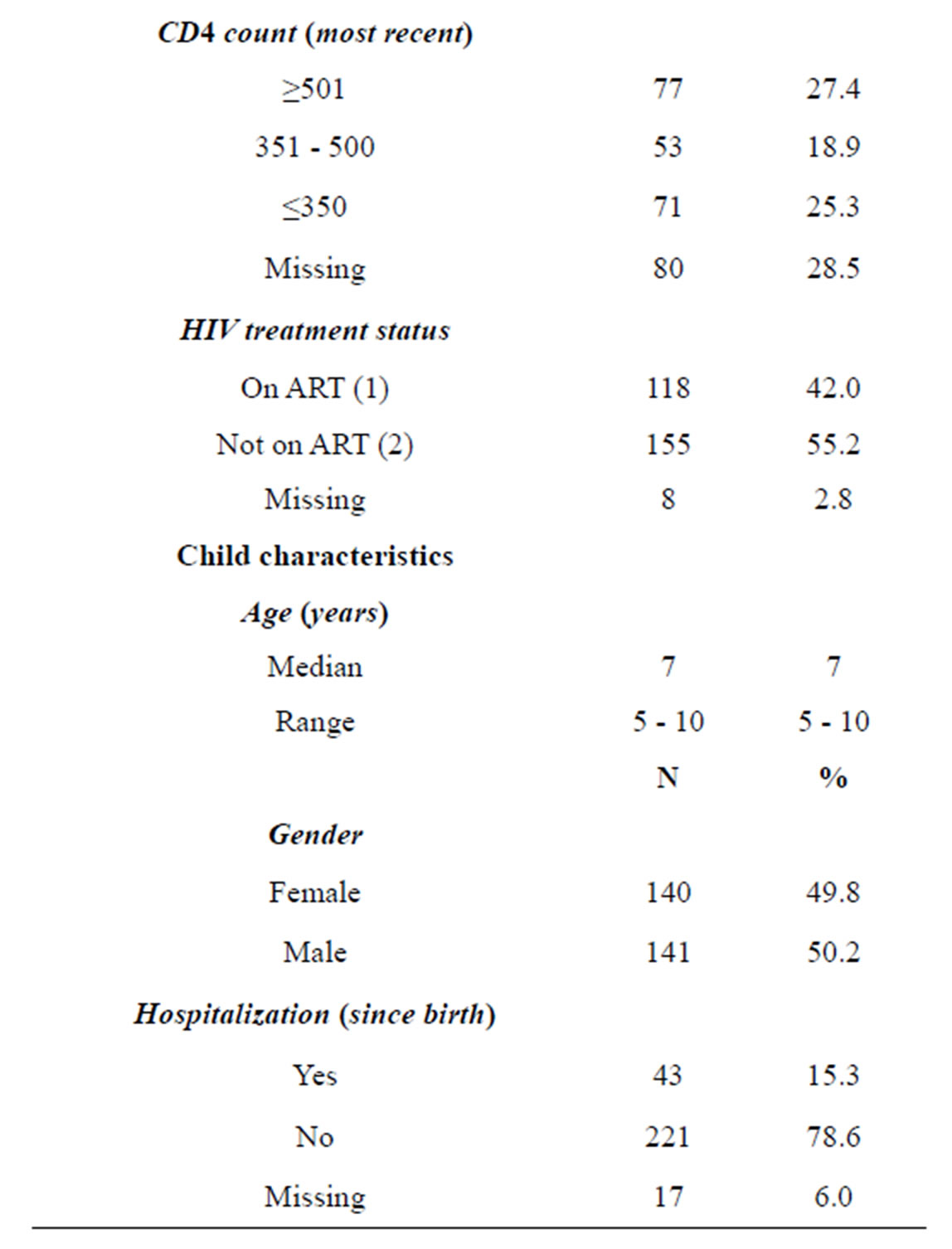
Table 1. Maternal and child characteristics.
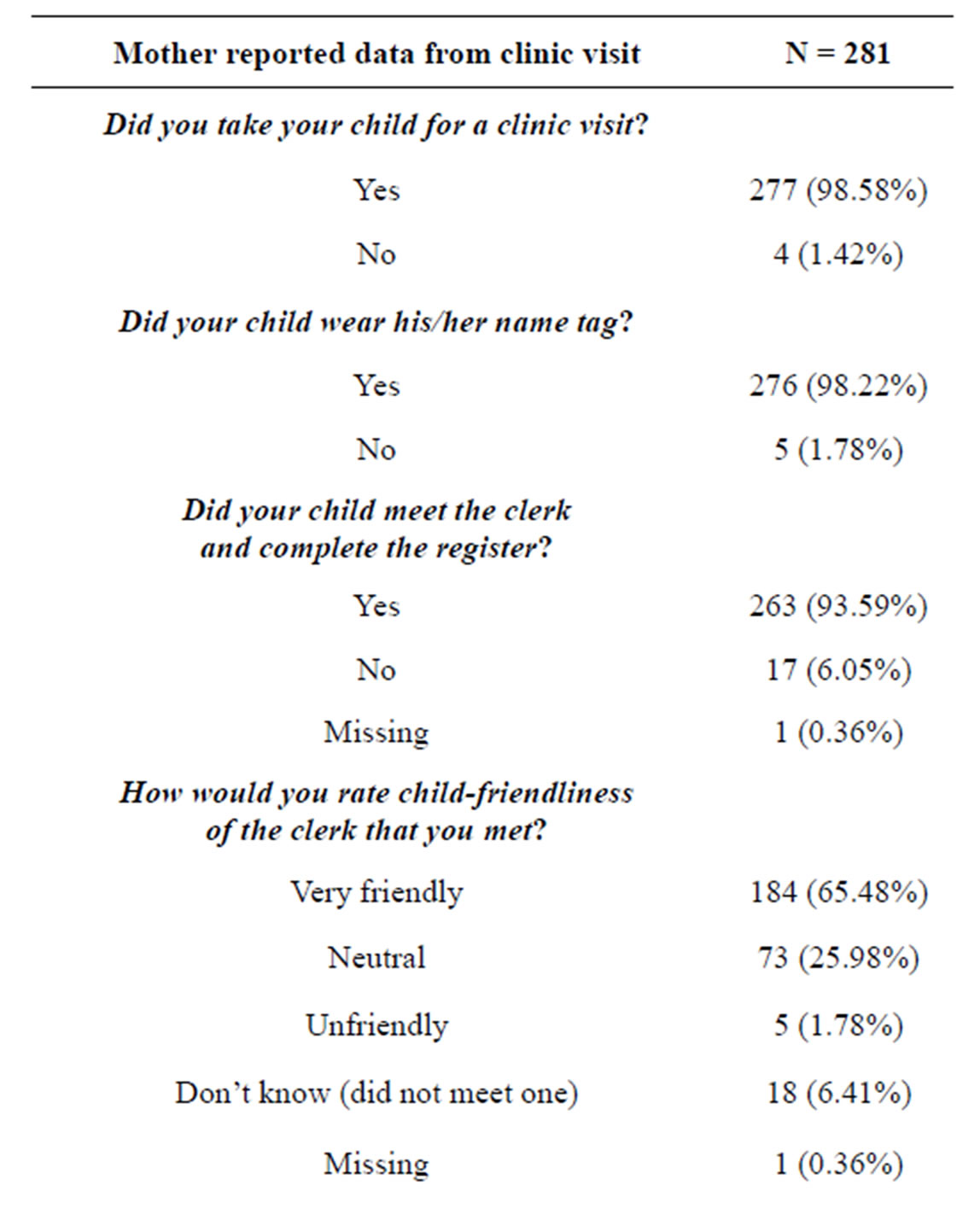

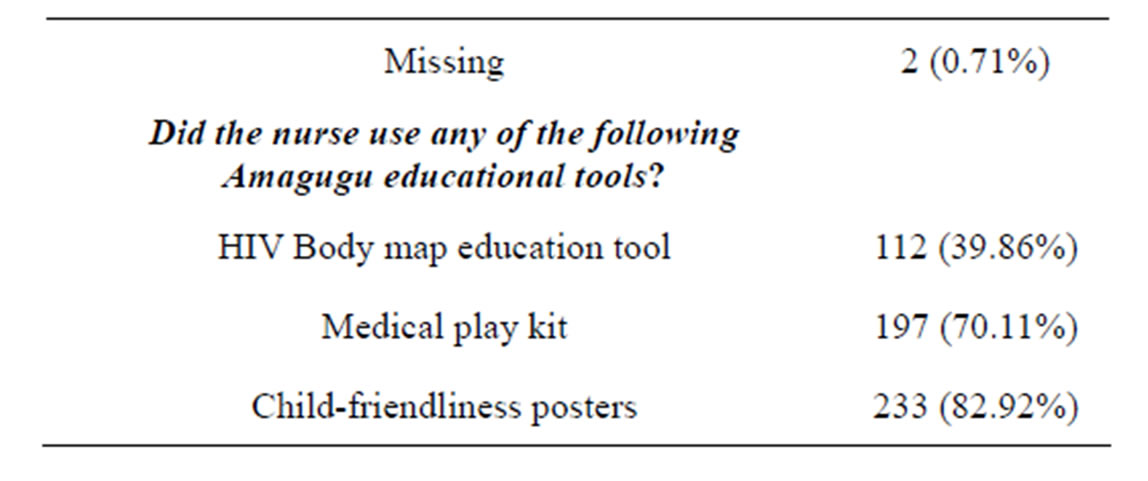
Table 2. Maternal experiences of child-friendliness at the health promotion clinic visit.
Continued
1) Willingness to participate in, and acceptability of, child-friendly initiatives and health promotion for children
The importance of children’s rights to friendly and accessible health facilities, emphasised in the training, resonated with most participants. In focus groups, discussion centred on beliefs about what a child-friendly clinic should or should not be. Participants felt that clinics should represent safe and welcoming places where children were not discriminated against. One 47-yearold female nurse stated: “I think it (child-friendliness) means that if the child is below the age that they can go to the clinic by themselves, they should not be scared of going to the clinic when left alone at home and they have a running stomach. They should just have that confidence that I’m used to going to the clinic and I know that they are going to help me. They can just go because they know that children are welcome at the clinic, they don’t get scolded and they are not in that frightened state.”
Mothers agreed that the health promotion visit encouraged their children to visit the PHCs. A 49-year-old mother of an 8-year-old boy said: “From there (after disclosing) I started talking to him about positive living, and we continued educating each other about sickness and pills and I made him have an interest in going to the clinic and enjoy it. He used to be that person that fears going to the clinic; he feared that they will give him an injection. He ended up liking the clinic and being interested in going there and wants us to go there all the time.”
A 36-year-old mother of an 8-year-old girl echoed the same sentiments: “Through participating in the Amagugu intervention I got encouraged to go to the clinic because we sometimes forget. The child also enjoyed visiting the clinic”.
2) Activities that support child-friendly initiatives
Table 3 summarises the activities thought to support child-friendliness in the focus groups.