The use of diuretics in acute heart failure: Evidence based therapy? ()
1. INTRODUCTION
There is no universally agreed definition of acute heart failure, but it is generally considered to represent the relatively abrupt onset of symptoms severe enough to merit hospitalization. It can occur de novo, or in patients with chronic heart failure, in whom it is termed acute decompensated heart failure. In extreme cases, cardiogenic shock may be present where there are symptoms of poor organ perfusion as a consequence of low cardiac output and a low blood pressure.
Fluid retention or shift is a key feature of acute heart failure, manifesting as ankle swelling, ascites, and/or pulmonary edema. Therapeutic strategies to control fluid balance, and to shift fluid out of the interstitium, lead to significant symptomatic relief and improved health-related quality of life.
Before modern diuretics were available, the treatment of fluid retention was limited to the use of such mechanical measures as rotating tourniquets to reduce preload, Southey tubes inserted through the skin to drain fluid [1] and venesection [2]. In 1785, digoxin, given in the form of foxglove, was also reported to have a diuretic effect, as observed by William Withering, and was the treatment of choice for dropsy, a condition characterized by congestion [3].
The first diuretics that were available were mercurial diuretics given via intramuscular injections [4]: their effect was discovered coincidentally when patients were treated with these drugs for syphilis. The treatment of fluid retention in heart failure was revolutionized with the development of thiazide diuretics in the 1950s [5] and loop diuretics in the 1960s [6].
The clinical evidence for the efficacy of diuretics in reducing the symptoms of heart failure is based on clinical experience and relatively small-randomized studies. Most clinical practice guidelines on the management of heart failure have given diuretic therapy a “Class I” recommendation (evidence and/or general agreement that a given treatment or procedure is beneficial, useful or effective), with a level of evidence based on expert opinion for relief of symptoms of congestion in patients presenting with fluid retention [7,8].
In the most recent European guidelines on heart failure [8] diuretics are recommended for the relief of dyspnea and edema in patients with signs and symptoms of congestion, irrespective of left ventricular ejection fraction, with the stated aim of achieving and maintaining euvolemia with the lowest achievable dose. It is acknowledged that the dose must be adjusted, particularly after restoration of “dry body weight”, to avoid the risk of intravascular volume depletion and dehydration, which can lead to hypotension, renal dysfunction and the inability to introduce disease modifying therapies such as angiotensin converting enzyme inhibitors, beta-blockers and mineralocorticoid receptor antagonists.
In this review we discuss the evidence base for the use of these modern diuretics in the management of acute heart failure.
2. TYPES OF DIURETIC
There are four pharmacological classes of diuretics used in HF:
a) Loop diuretics (furosemide, bumetanide, torasemide, ethacrynic acid);
b) Thiazide diuretics (hydrochlorothiazide, bendroflumethazide, or the “thiazide-like” metolazone);
c) Directly acting potassium-sparing diuretics (amiloride and triamterene);
d) Mineralocorticoid receptor antagonists (spironolocatone, canrenoate and eplerenone).
2.1. Loop Diuretics
Loop diuretics are the most commonly used diuretics for HF. They act on the ascending limb of the loop of Henle, blocking the reabsorption of up to 20% - 30% of filtered sodium by inhibiting the sodium, potassium and chloride co-transporter. This results in an intense, and usually short-lived, diuresis. The drug must be delivered to the lumen of the nephron and is thus dependent on glomerular filtration being sufficiently preserved.
Loop diuretics have a rapid onset of action, working within minutes when given intravenously or within 30 minutes when given orally [9]. They have a short halflife, so their action is usually of short duration, and consequently they may have to be given several times in a day to maintain the diuretic effect, and to minimize rebound sodium reabsorption. They can be administered orally, or intravenously as a slow injection or an infusion.
All the loop diuretics are roughly equivalent in terms of efficacy but oral bumetanide has higher bioavailability, so may be more useful than oral furosemide in patients with marked fluid retention or gut absorption problems. Bumetanide is more potent than furosemide with a 1:40 dose equivalence. Torasemide has a longer half-life (3 - 4 hours), therefore can be given less frequently than furosemide or bumetanide. Bumetanide and torasemide undergo hepatic elimination, as opposed to furosemide which undergoes renal elimination, therefore the latter is likely to accumulate with renal impairment. Absorption of oral loop diuretics can be delayed by food. Nonsteroidal antiinflammatory drugs blunt the natriuretic response to all of the loop diuretics by preventing the prostaglandininduced rise in renal blood flow that accompanies and sustains the natriuretic response to loop diuretics. This effect is not seen with low-dose aspirin (<1 mg/kg/day) [10].
All loop diuretics, but particularly furosemide, cause changes in systemic hemodynamics that are initially unrelated to the degree and extent of natriuresis that they induce. Short-term administration of furosemide leads to a rapid increase in venous capacitance and a decline in cardiac filling pressure, coincident with a rise in plasma renin activity. This effect predominates over any rise in systemic vascular resistance in patients with pulmonary edema or decompensated acute heart failure [11]. This effect is maximized at an intravenous dose of 20 mg [12].
All of the loop diuretics possess some ototoxicity, with ethacrynic acid the worst. Transient hearing loss may occur in patients receiving rapid intravenous bolus injection—so injection at a rate > 4 mg/minute is not advisable. Permanent sensorineuronal hearing loss may occur at doses equivalent to furosemide 1000 mg per day [13].
2.2. Thiazide and Thiazide-Like Diuretics
Thiazide diuretics act on the distal tubule, where they inhibit sodium and chloride reabsorption, and block 10% - 15% of sodium reabsorption. They cause a slower onset (1 - 2 hours) and more prolonged (12 - 24 hours) but milder diuretic effect compared to a loop diuretic. Rebound sodium reabsorption is unlikely to occur. Despite thiazide diuretic having a less potent diuretic effect, their long duration of action allows a similar degree of sodium excretion to occur throughout a 24-hour period as compared to a loop diuretic [14]. Thiazides are more likely to result in hypokalemia and nocturia as they have a longer duration of action. Thiazides on their own are largely ineffective if glomerular filtration rate is below 30 ml/ min, but they may be useful in combination with a loop diuretic in patients who have refractory edema.
Metolazoneacts like a thiazide, but in addition it acts on the proximal tubule where 60% - 70% of sodium is reabsorbed. Therefore metolozone can result in a profound diuresis when combined with a loop diuretic. It appears to be effective even in moderate renal dysfunction [15]. Such combination usage is typically only required for a few days in most cases of resistant fluid retention.
2.3. Potassium Sparing Diuretics
Potassium sparing diuretics (such as amiloride) produce a mild diuretic effect by blocking the sodium/potassium exchange pump in the distal tubule. This exchanger is highly active in patients with HF who are on the combination of a loop and thiazide diuretic. As they have a weak diuretic effect, they are mainly used in combination with thiazide or loop diuretics to prevent hypokalemia [16,17], as they appear to be more effective than potassium replacement [18]. There is a risk of hyperkalemia, particularly in patients with renal dysfunction [19].
Aldosterone (mineralocorticoid) receptor antagonists are mainly used at low dose as neuro-hormonal blockers, for prognostic benefit, rather than as diuretics per se. However, in patients with right sided heart failure, liver impairment and ascites, characterized by very high circulating levels of aldosterone, higher doses of spironolactone (typically, 200 - 400 mg/day) are often used for their diuretic effect.
Common side effects of diuretics most frequently used in ADHF are summarized in Figure 1.
3. EVIDENCE BASE FOR THE USE OF DIURETICSIN ACUTE HEART FAILURE
The evidence based for the use of diuretics in acute heart failure is limited. Trials of diuretics in HF patients with a description fitting the contemporary definition of ADHF such as hospitalized patients with worsening symptoms, or those with NYHA II-III characterized by fluid retention are described and are summarized in Figure 2. Trials not fitting this description were not included.
3.1. Placebo-Controlled Trials of Diuretics
Placebo-controlled randomized trials of diuretic therapy for the treatment of heart failure are limited to studies that include small number of patients (3 - 247 patients). However, all of these studies reported that diuretics significantly improved symptoms in heart failure [20-25]. None was powered to estimate the effect on mortality,
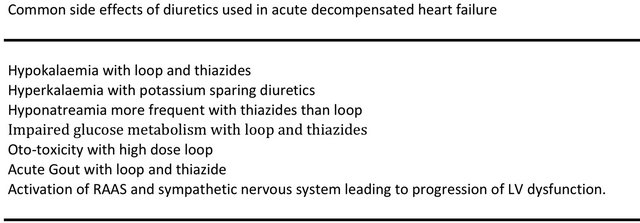
Figure 1. Common side effects of diuretics used in acute decompensated heart failure.

Figure 2. Renin-angiotensin-aldosterone system (RAAS).
but a meta-analysis of three short-term studies reporting mortality (follow-up ranging from 1 - 12 months) suggested a 75% reduction [95% CI 16% - 93% P = 0.03] in the risk of death, however the number of deaths were low (12 in the placebo group and 3 in the diuretic group), and the majority of the patients within the meta-analysis were unlikely to have met the contemporary definition of ADHF [26].
3.2. Thiazide versus Loop Diuretic
The evidence from several small studies (studies with more than 10 patients are listed in Figure 2) suggests that loop diuretics are more effective than thiazides alone in the management of HF [25,27,28]. Thiazides are also more likely to result in hypokalaemia and hyponatreamia [14,25,29]. Patients may prefer thiazides, however, as they have a less harsh onset and longer duration of action [30].
3.3. Comparison between Loop Diuretics
In the past 20 years the only head-to-head comparisons between loop diuretics have been between torasemide and furosemide. Four of these studies were randomized [31-34]; see Figure 2, but only two enrolled patients with acute decompensated heart failure [32,33], both in the USA. Both of these studies were unblinded. At 12 months Stroupe [32] reported half the risk of readmission in the torasemide-treated group (18% vs 34%; P = 0.013), but the larger study by Murray [33] reported no difference in all-cause rehospitalization, although HF readmission was reduced in those taking torasemide (19% vs 32% P < 0.01).
A randomized open-label study in primary care confirmed that torasemide was better tolerated than furosemide, with less urgency to micturate and less daily restrictions reported by the 237 patients, but there was no difference in the risk of hospitalization, adverse events, or mortality [34].
In general, international guidelines do not favor one loop diuretic over another [7,8]
3.4. Dose of Loop Diuretic
The Diuretic Optimization Strategies Evaluation (DOSE) trial is the largest prospective, double blind, randomized ADHF trial to evaluate initial diuretic strategies in patients with acute decompensated heart failure [35]. Using a 2 × 2 factorial design, the DOSE trial randomized 308 ADHF patients to IV furosemide given as twice-daily boluses or continuous infusion and to either a low dose (IV dose numerically equivalent to the patient’s oral dose) or a high dose (2.5 times oral dose given intravenously) strategy, with specified dose adjustments permitted after the first 48 hours.
There was no significant difference in either of the coprimary endpoints of global assessment of symptoms, or change in serum creatinine over 72 h, with diuretic administration by bolus or continuous infusion or with a lowversus a high-dose strategy. However, patients randomized to the higher dose strategy had a more favorable outcome with regard to several secondary measures, including relief of dyspnea (P = 0.04), change in weight (P = 0.01), and net fluid loss (P = 0.01), albeit with a greater risk of serum creatinine increasing by >0.3 mg/dl within 72 hours (23% versus 14%, P = 0.04). There was no difference in length of initial hospital stay, or in days alive and out of hospital at day 60.
The trial data therefore suggest that a strategy of using higher doses of diuretics on admission to hospital with ADHF is likely to more rapidly control fluid retention and relieve symptoms, at the cost of a slightly higher risk of renal dysfunction that does not appear to have medium-term consequences.
3.5. Bolus versus Continuous Infusion of Loop Diuretic
In the DOSE trial [35] there was no statistically significant difference between continuous infusion or twice daily bolus injection of furosemide in terms of the patients’ global assessment of symptoms, mean change in serum creatinine, net fluid loss, change in weight or length of hospital stay. This confirmed the result of an earlier single-centre randomized but single-blind study [36].
3.6. Use of Hypertonic Saline to Facilitate Effect of Loop Diuretics
One group has published several randomised studies where the combination of hypertronic saline infusion (150 ml of 3% NaCl) with a furosemide 250 mg infusion appeared superior to furosemide alone. All of the studies have been single-blind, but have reported increased diuresis and serum sodium levels, and a reduction in initial hospitalization length of stay. Mortality is also reported to be reduced on follow-up as is readmission rate, with the largest study of 1771 patients reporting a mortality of 12.9% versus 23.8% P < 0.0001, and readmission proportion of 18.5% versus 34.2% over a median follow up of 57 months (P < 0.0001) [37]. The proposed mechanism of action is expansion of intravascular volume, improved renal blood flow, and shift of fluid from the interstitium into the circulating volume [38].
This method of increasing diuresis has not been endorsed by international guidelines, and further studies from other groups are awaited.
4. DIURETIC RESISTANCE
There is no accepted definition of diuretic resistance. Often diuretic resistance is described when higher doses of diuretics are needed to gain a similar diuretic response, or when the diuretic response is either diminished or lost before the therapeutic goal is reached. Diuretic resistance is associated with a poor prognosis [39], and has been reported in occur in up to a third of hospitalized patients [40].
Mechanism involved in diuretic resistance are illustrated in Figure 3, and include:
• Decreased drug bioavailability: increased peripheral and bowel wall oedema, leading to reduced absorption of the diuretic, in particular with oral furosemide [41,42].
• Reduced glomerular filtration rate: may occur secondary to a reduced renal perfusion due to low cardiac output or venous congestion. Chronic kidney disease, or acute kidney injury, can prevent diuretics exerting their beneficial effects. For example, furosemide has to be secreted by the organic acid transporter in the proximal tubule to reach its site of action [43]: reduced GFR can therefore reduce delivery or reduce active secretion of loop diuretics.
• Excessive sodium uptake in the proximal tubule and the loop of Henle: may occur secondary to the following mechanisms:
◦ Excessive neuro-hormonal activation (renin-angiotensin system);
◦ The presence of the Braking phenomenon: occurs in the period between boluses of loop diuretic, when there is no diuretic in the proximal tubule or at the loop of Henle, leading to rebound excessive sodium reabsorption at both the proximal tubule and loop of Henle;
◦ The reduced active secretion of loop diuretic into the proximal tubule can also lead to less diuretic being delivered to site of action leading to less diuresis;
◦ Excessive sodium intake can also lead to diuretic resistance due to excessive sodium uptake in the proximal tubule.

Figure 3. Mechanisms of diuretic resistance.
• Renal adaptation: chronic diuretic use results in increased delivery of sodium to the distal convoluted tubule, which consequently hypertrophies [44,45], and can therefore retain more sodium (and water) than a diuretic naïve patient.
• Excessive sodium and water retention in the distal nephron and collecting ducts may occur secondary to excessive aldosterone and vasopressin mediated sodium and water retention, respectively
• Drug interaction: NSAIDS, aspirin [46], steroids, pioglitazone
• Pseudoresistance: poor compliance with diuretics can be misinterpreted as diuretic resistance. A good clinical history can help identify this, as can discussions with the patient’s family or carer.
5. OVERCOMING DIURETIC RESISTANCE
Several strategies can be employed in an attempt to overcome diuretic resistance in a patient with acute decompensated heart failure.
5.1. Diuretic Strategies
These include: changing the route of administration from oral to intravenous (thus overcoming bioavailability issues); continuous infusion of loop diuretic rather than intermittent bolus injections (minor effect); using higher doses of intravenous loop diuretics to increase dose reaching the tubules, particularly when glomerular filtration is poor; sequential nephron blockade by using a combination of diuretics [47-50] such as metolazone or bendroflumethazide in addition to a loop diuretic. Two of these randomized studies are summarized in Figure 2. This approach requires particularly close monitoring as it can lead to marked electrolyte disturbance, hypotension, dehydration and worsening renal function.
In some patients, restricting excessive dietary sodium and fluid intake can also help reduce diuretic resistance by reducing the sodium and fluid load arriving at the nephron.
5.2. Non-Diuretic Strategies
There are several non-diuretic strategies to enhance the effectiveness of diuretic therapy.
5.2.1. Renal Dose Dopamine
Dopamine has a dose-dependent mechanism of action. At doses of 2 - 3 μg/kg/min (renal dose dopamine) the drug acts on peripheral dopaminergic receptors (DA1 and DA2) resulting in vasodilation in the renal, coronary, splanchnic and cerebral circulations. At doses of 3 - 5 μg/kg/min, it acts as a β-agonist, and at higher doses (5 15 μg/kg/min) it acts also as an α-agonist inducing peripheral vasoconstriction [8]. The exact mechanism through which dopamine increases renal blood flow remains debated, but is likely to be related to an increase in cardiac output [51] and renal and peripheral vasodilation [52]. The latter effect may be less in advanced heart failure, with selective loss in renal vasodilating capacity [51].
“Renal dose” dopamine together with intravenous furosemide infusion is often used in patients with low systolic blood pressure who have demonstrated a poor response to furosemide infusion alone, although the evidence base for this approach is weak.
The recent Dopamine in Acute Decompensated Heart Failure (DAD-HF) Trial in 60 patients, compared continuous 8-h high-dose furosemide infusion (20 mg/h) with the combination of low-dose furosemide infusion (5 mg/h) plus lowdose dopamine (5 μg/kg/min). Both strategies had a similar effect on total diuresis, and changes in dyspnea score, but worsening renal function was less common in the dopamine group (7% versus 30% P = 0.04) and serum potassium fell less in the dopamine group. There was no difference in length of stay, or in 60-day mortality or rehospitalization rates [53].
The Renal Optimization Strategies Evaluation in Acute Heart Failure (ROSE-AHF) trial is currently comparing the efficacy and safety of low dose dopamine versus intravenous nesiritide versus placebo in patients with ADHF treated with loop diuretics (NCT01132846).
5.2.2. Aquaretics
Vasopressin 2 receptor antagonists, such as tolvaptan, may promote an aquaresis by blocking the effects of vasopressin on the vasopressin 2 receptors located in the collecting ducts, thus blocking the resorption of free water as urine passes through the collecting ducts. This promotes water clearance without having an effect on sodium balance. In the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) trial, involving over 4100 patients with ADHF, tolvaptan at a dose of 30 mg once per day for a minimum of 60 days had no effect on total mortality or HF hospitalization when compared to placebo [54,55]. Tolvaptan did significantly improve hyponatremia in the patients with a baseline serum sodium less than 134 mmol/l (sodium increased by 5.40 mmol/l at day 7 or discharge, compared with an increase of only 1.85 mmol/l in the placebo group (P < 0.001)) and edema score at day 7 (P < 0.003, with 74% of tolvaptan patients reporting an improvement in pedal edema by at least 2 grades compared with 70% of placebo patients). The effect on serum sodium was maintained throughout a maximum of 40 weeks of treatment. The drug has not been licensed for use in ADHF.
5.2.3. Adenosine antagonists
Adenosine antagonists can potentially increase glomerular filtration, and enhance the diuretic effect of diuretic drugs. Despite promising early phase data, the placebocontrolled randomized study of the selective A1 adenosine receptor antagonist rolofylline for patients hospitalized with acute decompensated heart failure and volume overload to assess treatment effect on congestion and renal function (PROTECT) trial, involving 2033 patients with heart failure and renal dysfunction, reported that the adenosine antagonist, rolofylline, did not have any beneficial effects, and was associated with an increased risk of seizures [56].
5.2.4. Ultrafiltration
Acute decompensated heart failure patients with refractory oedema unresponsive to diuretic therapy may be considered for ultrafiltration (UF). This method is very effective at removing plasma fluid from blood across a semipermeable membrane, and the recent development of veno-venous peripheral UF with devices that focus on UF alone has positioned UF as a potential alternative to loop diuretics in ADHF [57]. Small studies suggest that UF improves pulmonary and peripheral edema, lung function and hemodynamics without adverse effects on renal function [58,59]. UF can remove fluid relatively rapidly, at rates of up to 400 ml/hour, but in practice 200 - 300 ml/hour is considered adequate. Lower rates may be used if there is significant right ventricular disease or pulmonary arterial hypertension. The fluid removal rate is reevaluated using clinical assessment and serial hematocrit measurements to ensure adequate vascular compartment refill [59,60], and help prevent further renin angiotensin aldosterone system activation, hypotension, and renal injury [61]. Another advantage of UF is that more sodium can be removed (and less potassium) as compared to diuretic therapy [62].
In randomized trials, the typical treatment period has been 24 hours, but UF membranes can last up to 72 hours with care.
There are three key trials of UF in patients with ADHF. The first, Relief for Acutely Fluid Overloaded Patients with Decompensated Congestive Heart Failure (RAPIDCHF), was a proof of concept study of 40 patients with ADHF randomized to a single 8 hour period of UF or to usual care [63]. There was no significant difference between UF and usual care for the primary end point of weight loss at 24 hours, but fluid removal after 24 h was significantly greater with UF, with significantly improved dyspnea and HF symptoms at 48 h in the UF group. The second trial was the Ultrafiltration versus Intravenous Diuretics for patients hospitalized for acutely decompensated heart failure (UNLOAD) trial [58], which enrolled 200 patients with ADHF, unblinded and randomized to either UF or loop diuretic therapy within 24 h of hospitalization. The co-primary endpoints of the UNLOAD trial were weight loss and dyspnea relief at 48 h. The UF group had greater weight loss (5.0 ± 3.1 kg vs 3.1 ± 3.5 kg; P < 0.001), but there was no difference in the patient-reported outcome of dyspnea. Patients with UF also had lower rates of rehospitalization for HF compared with diuretic therapy (16 of 86 UF patients vs 28 of 87 usual care patients; P < 0.04). There was significantly less hypokalemia and also no difference in serum creatinine with UF compared with diuretics. The third trial is the recently published Effectiveness of Ultrafiltration in Treating People with Acute Decompensated Heart Failure and Cardiorenal Syndrome (CARESS-HF) study [64]. This trial looked at 198 patients with ADHF, worsened renal function and persistent volume overload and patients were randomized to a strategy of UF versus stepped pharmacological management with a primary endpoint of the change in serum creatinine and change in weight considered as a bivariate endpoint at 96 h. This trial showed that UF at a removal rate of 200 ml/hour of fluid was inferior to stepped pharmacological therapy for the primary end point, owing to an increase creatinine level at 96 hours (20.3 ± 61.9 vs –3.5 ± 46.9 mmol/l; P = 0.003). There was no difference in weight between the UF and stepped pharmacological therapy at 96 hours, with a mean of 5.5 Kg weight loss. UF was associated with higher rate of adverse events related to hypotension or filter problems.
International guidelines suggest that despite these recent trials, further trials are required to assess the exact role of UF in ADHF [8]. Furthermore, the economic impact of UF as an initial strategy for ADHF remains uncertain, and the recent review on the financial implications of UF highlighted the high costs of disposable materials and staff training [65].
In our experience, patients who are unsuitable candidates for UF include those with poor venous access, those in cardiogenic shock requiring inotropic support, and patients with advanced renal disease in whom renal replacement therapy with hemofiltration would be more appropriate.
6. CONCLUSIONS
Diuretics have an important role in the management of ADHF. Although the evidence base is not extensive, they remain the mainstay of first line therapy. International guidelines endorse the use of diuretic therapy for the relief of symptoms of congestion, and their use is likely to remain key to clinical management for the forseeable future.
The initial management strategy is likely to be a loop diuretic, such as furosemide, and the evidence suggests that an initial “high dose” strategy either by twice daily bolus injection or continuous infusion is likely to be more successful than a slower, more “ramped” approach. In cases of diuretic resistance, adding a thiazide or thiazide like diuretic can enhance diuresis, although close monitoring of fluid balance and electrolytes is necessary. This strategy can also be useful in patients with significant renal dysfunction. Low dose (renal dose) dopamine infusion can improve the effectiveness of diuretic therapy, and help maintain renal function, although the evidence base for this is also limited. Mechanical ultrafiltration is increasingly used for the treatment of fluid retention and/or diuretic resistance, but further trials are required to assess which patients would benefit most from this treatment modality.
NOTES