Intravascular Profile of Coronary Artery Disease in Diabetic Patients with Acute Coronary Syndrome: Results of the Saudi Coronary Athero-Thrombotic Disease (SAUDICAT) ()
1. Introduction
Coronary artery disease (CAD) remains the main cause of death in patients with diabetes mellitus (DM) [1] . Diabetes affects nearly one in ten adults and its prevalence is increasing worldwide [2] . The epidemic situation is even worse in Middle East countries, especially in Saudi Arabia where DM prevalence in adults reaches 23.7% [3] and CAD affects 5.5% of the population [4] .
The coronary artery lesions in diabetic patients are more extensive and diffuse. Revascularization therapies are still debated and clinical outcomes after either percutaneous coronary interventions (PCI) or coronary artery bypass graft (CABG) are poorer than in non-diabetic patients [5] .
The cardiac catheterization laboratory at King Salman Heart Centre is the leading center in the use of intravascular ultrasound (IVUS) in Saudi Arabia and the region: ~30% of PCI are IVUS-guided (unpublished data). We embarked on investigating the spectrum of Coronary Athero-Thrombotic Disease of Saudi patients (SAUDICAT) presenting with Acute Coronary Syndromes (ACS). Our aim was to establish a database of anatomically defined Athero-thrombotic disease in Saudi nationals in Diabetic compared with Non-Diabetic (NDM) patients. While coronary angiography offers only the possibility to scan the luminograms, IVUS also provides detailed information about the extent of the disease and the conformational changes within the vessel walls over the length of the lesion. Ultrasonic examination typically reveals three-layered components of the coronary wall: the intima, the media and the adventitia, each of which possess a variable echogenicity.
Since the clinical course and outcomes of DM patients are in many ways more challenging and pose considerable stresses on optimal management including the choice of the most appropriate interventions, we opted to study our largely diabetic population of Saudi patients who presented with ACS.
The selection of intermediate lesions for IVUS evaluation was considered more appropriate in order to avoid plaque distortion by prior ballooning of more severe lesions. IVUS provides real-time high resolution cross-sectional tomographic images from lumen and vessel wall. Current intracoronary ultrasound catheters typically range in size from 2.9 to 3.5 French (0.96 - 1.17 mm in diameter) and can therefore only be used in the proximal and mid segments of the coronary arteries and in the absence of tight coronary stenosis. IVUS is commonly used in high volume PCI centers, but its use is limited to certain interested and trained operators.
2. Material and Methods
This is a retrospective study conducted at King Fahad medical city. All procedures performed involving human participants were in accordance with the ethical standards of the national research committee. An informed consent was obtained from all individual participants included in this study. A total of 504 IVUS studies in 441 patients were reviewed. The indication for the IVUS studies was to evaluate angiographically intermediate coronary lesions. All IVUS studies were screened in order to exclude from the current analysis IVUS runs performed in patients with instent restenosis, runs that were technically inadequate or without automatic pullback. Of all the reviewed IVUS runs a total of 210 IVUS studies in 181 patients were considered suitable for analysis in keeping with the inclusion/exclusion criteria summarized in Table 1.
2.1. Clinical Data
We reviewed hospital records of all patients presenting with ACS to obtain information on clinical demographics and medical history, including troponin negative unstable angina and troponin positive NSTEMI and acute STEMI with borderline lesions. Patients with ischemia driven heart failure were also included. Eight patients diagnosed as stable angina were included because after careful review their diagnosis appeared to be unstable angina. The respective clinical presentation data, major cardiac risk factors and cardiac biomarkers were collected.
2.2. IVUS Analysis
Segments of interest were selected around the most affected diseased segment harboring the minimal cross sectional area (CSA) or maximal plaque burden (PB), as shown on Figure 1. Less diseased, most normal reference segments (distal and proximal-panels A and E on Figure 1) were also analysed. For the lesion runs that ended ostially like LAD-LM, LCx-LM, Diagonal-LAD or OM- LCx, the analysis was stopped at the bifurcation and taking into account the vessel size differences, only the distal reference segment was taken into account. The standard speed of the pullback runs were 0.5 mm per second. Each segment of interest was divided into 0.5 mm thin slices. Manually corrected digitally obtained intimal and external elastic membrane (EEM) tracings were carried out
![]()
Table 1. Inclusion and exclusion criteria.
![]()
Figure 1. IVUS analysis of a mild LAD lesion. Measurements of luminal, plaque and vessel areas were done every 0.5mm, on the slices marked with the yellow ticks on the longitudinal view in the lower center panel. Panel A shows the proximal reference with an eccentric plaque between 6 and 9 o’clock. External elastic lamina is traced in red, lumen border in yellow. Lumen area was 11.0 mm2, vessel area 16.3 mm2 and plaque burden 32.5%. The corresponding location on the longitudinal view is indicated by A. More distally, at the level of a small septal branch seen at 10 o’clock on panel B, a plaque with superficial calcium and shadowing behind is seen between 7 and 9 o’clock, with its corresponding location on the longitudinal view (B, in the shadowed region). Panel C shows the cross-section with the minimal lumen area (3.7 mm2), demonstrating positive remodeling (vessel area 14.8 mm2, plaque burden 75%, remodeling index 1.1). Panel D shows distally where the plaque burden started to be >50%, accumulating between 7 and 11 o’clock (lumen area 6.7 mm2, vessel area 13.8 mm2, plaque burden 51%). Panel E is the distal reference with the least plaque accumulation before any significant side branch (lumen area 8.7 mm2, vessel area 12.1 mm2, plaque burden 27.9%).
using INDEC medical system software (EchoPlaque v 4.0, INDEC Medical System, Santa Clara, CA). The analysis was carried out in collaboration with the IVUS Core Laboratory of UMONS.
2.3. IVUS Parameters
・ Cross Sectional Area (CSA, in mm2),
・ IVUS slice thickness (mm) = distance between 2 consecutively measured CSA,
・ Average Lumen Diameter (ALD, mm),
・ Lumen Area (LA, mm2),
・ Average Vessel Diameter (AVD, mm),
・ Vessel Area (VA, mm2) = EEM CSA,
・ Plaque Area (PA, mm2) = VA − LA,
・ Plaque Burden (PB, %) = 100 × (VA − LA)/VA,
・ 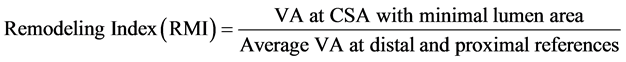 ,
,
・ Lumen Volume (LV, mm3) = ∑Lumen CSA × IVUS slice thickness,
・ Vessel Volume (VV, mm3) = ∑EEM CSA × IVUS slice thickness,
・ Plaque Volume = (Vessel Volume − Lumen Volume),
・ Percent Volume Obstruction (%) = 100 × Plaque Volume/Vessel Volume.
2.4. Statistical Analysis
The collected data were entered and analyzed using SPSS ver. 22. Descriptive statistics were done for all studied variable expressed as mean ± standard deviation (SD) for continuous variables and as percentages for categorical variables. Bivariate analysis was done on categorical data, compared using chi-squared test. Analysis of variance (ANOVA) using Scheffee method and t-test were used appropriately to compare means of quantitative variables. Significant P value was set to be <0.05 through the study.
3. Results
A total of 181 patients were included, mean age was 57.8 ± 10.1 years. In 210 IVUS pullback, inclusion and exclusion criteria were met and 78% (n = 163) of these IVUS runs were recorded in men. Overall, 71% (n = 128) of our patients were diabetics with higher rate of associated cardiac risk factors as compared to non-diabetic group. STEMI was the most common clinical presentation (47.8%, n = 88). We observed that the patients in the diabetic group were more frequently suffering from a NSTEMI (p < 0.01). Table 2 summarized the principal clinical features and sociodemographic data of our population according to the presence or absence of diabetes mellitus.
Among the 210 IVUS pullback analyzed, most of the segments of interest were located in the left anterior descending artery (155 IVUS runs, 73.8%). Detailed locations of analyzed segments are summarized in Table 3.
As compared to non-diabetics, patients with DM had significantly larger plaque volume (267.4 ± 173.7 mm3 versus 193.1 ± 111.1 mm3 for non DM group, p < 0.01), larger vessel volume (495.9 ± 313.6 mm3 versus 358.2 ± 181.7 mm3,
![]()
Table 2. Sociodemographic data and clinical features.
DM: diabetes mellitus group, NDM: non-diabetic group, STEMI: ST elevation myocardial infarction, NSTEMI: non ST elevation myocardial infarction, UA: unstable angina, SAP: stable angina pectoris, IHF: ischemic heart failure, SOB: shortness of breath (clinical presentations were not exclusive). (p value for the comparison DM vs NDM).
![]()
Table 3. Segments of interest in all IVUS studies.
LM: left main coronary artery, LAD: left anterior descending coronary artery, D: diagonal branch, LCx: left circumflex artery, OM: obtuse marginal artery, PL: posterolateral artery, RCA: right coronary artery, PDA: posterior descending artery. Although LM was included in the LAD (proximal and ostial) runs, LM runs were excluded from final IVUS analysis. Each IVUS run could include multiple segments (total = 631).
p < 0.01), larger lumen volume (231.2 ± 156.2 mm3 versus 163.5 ± 87.9 mm3, p < 0.01) and longer lesions (37.37 ± 12.25 mm versus 29.93 ± 8.43 mm, p < 0.01) as shown on Figure 2.
Both DM and NDM patients had an increased remodeling index without a significant difference (1.4 versus 1.3, p = 0.7).
We did not observe any other significant difference between the two groups, in particular percent plaque volume and obstruction were not different (Table 4).
The above findings were more obvious in the STEMI subgroup. Diabetic patients with STEMI had significantly larger lumen diameter and area, bigger lumen, plaque and vessel volume and longer lesions as compared with non-dia- betic patients with STEMI (Table 5). In patients with NSTEMI, UA or equivalents, we did not find a statistically significant difference between DM and NDM groups.
4. Discussion
Diabetes mellitus has been associated with an increased risk of cardiovascular
![]()
Figure 2. Box plot with scatter diagram for Lumen volume (L vol), Vessel volume (V vol) and Plaque volume (P vol), in mm3, for DM vs NDM patients.
disease. Moreover, individuals with diabetes are generally more difficult to treat due to associated comorbidities, more complex coronary lesions and more frequent in-stent restenosis. The aim of the current study was to establish an intravascular profile of coronary stenosis in Saudi diabetic patients.
It is well known, based on previous angiographic or post mortem studies, that diabetic patients experience more extensive atherosclerosis with more frequent multivessel disease and more severe and diffuse coronary lesions [6] [7] [8] [9] .
![]()
Table 4. IVUS finding in lesion segment in diabetics patients as compared to non-dia- betics.
DM: diabetes mellitus group, NDM: non-diabetic group, ALD: average lumen diameter, AVD: average vessel diameter, LA: luminal area, VA: vessel area, PA: plaque area, PB: plaque burden, MVD: minimal vessel diameter, MLD: minimal luminal diameter, LL: lesion length, V vol: vessel volume, L vol: luminal volume, P vol: plaque volume, PPV: percent plaque volume, PVO: percent volume obstruction, RMI: remodeling index.
![]()
Table 5. Major IVUS finding according to clinical presentation in diabetic patients compared to non-diabetics.
STEMI: ST elevation myocardial infarction, NSTEMI: non ST elevation myocardial infarction, UA: unstable angina, DM: diabetes mellitus group, NDM: non-diabetic group, ALD: average lumen diameter, LA: luminal area, LL: lesion length, V vol: vessel volume, L vol: luminal volume, P vol: plaque volume, RMI: remodeling index.
However, other researches demonstrated that the angiographic profiles are similar among diabetic and non-diabetic patients [10] [11]
Our study demonstrates that in Saudi diabetic patients with acute coronary syndrome, coronary lesions are longer, with more plaque but without an increased remodelling index as compared to non-diabetics.
While recent IVUS studies focused on plaque virtual histology in the diabetic population, few trials compared quantitative intravascular parameters and showed controversial results. Hong et al. [12] reported similar results to ours showing that DM patients with ACS seems to have relatively larger vessel, lumen and plaque volume than NDM patients (respectively in mm3 272 ± 211 vs 263 ± 220, 131 ± 103 vs 129 ± 100 and 141 ± 115 vs 134 ± 126; p: NA). Larger plaque volume was also reported in a sub analysis of the TRUTH Study [13] but unlike our study DM patients had relatively smaller lumen volume and shorter lesions. In 86 patients with ACS, there was no significant differences found in culprit lesions quantitative analysis among the two groups [15] . These studies were conducted in eastern Asiatic population with different baseline characteristics and inclusion criteria.
In a recent prospective observational study, Kuroda et al did not find a significant difference between DM and NDM patients in terms of plaque volume, plaque burden and lesion length [14] . However, ACS were excluded from this study.
Our patients, DM and NDM ones, had an increased remodeling index. This finding goes against previous studies that have shown a high prevalence of negative artery remodeling in diabetics patients [16] [17] [18] .
Conducted in different populations, these controversial results should be taken with caution.
5. Study Limitations
The current study was retrospective and monocentric. Detailed biological features are not reported, considered out of the scope of this report. No qualitative analysis of the plaques was attempted, knowing the variability of grey-scale interpretation in this population [19] .
6. Conclusion
Diabetic patients with acute coronary syndrome in Saudi Arabia have larger vessel, lumen and plaque volume and longer lesions. This is the first intravascular database in the region that could lead to a better understanding of coronary artery disease particularities in our patients, a better therapeutic management and more favorable prognosis.
Acknowledgements
This work would not have been completed without the help of Mr Nadir Siddiqi with his expert contribution in data analysis. We also would like to thank the cardiovascular technologists Lamis Al Shahrani, Amal Al Bunyan, Shiraz Mirza and Ola Al Kathiri who dedicated their time and effort to collecting and analysing the IVUS runs and collecting the patients’ clinical database.