Assessment of ESAK and ED for Adult’s Patients Examined by Computed Radiography ()
1. Introduction
Present day computed radiography (CR) is based on the use of photostimulable phosphors, which are also known as storage phosphors [1] . Computed radiography (CR) is at this moment the most common digital radiography modality in radiology departments, in place of conventional screen film systems. With the CR technology, the detector is a photostimulable phosphor screen, usually indicated as an imaging plate (IP).
They are commercially the most successful detectors for digital radiography; the phosphors used are most often in the barium fluorohalide family [2] in powder form and deposited onto a substrate to form an imaging plate or screen. X-ray absorption mechanisms are identical to those of conventional phosphor screens used with film. They differ in that the useful optical signal is not derived from the light emitted in prompt response to the incident radiation, but rather from subsequent emission when the latent image, consisting of trapped charge, is optically stimulated and released from metastable traps. This triggers a process called photostimulated luminescence (PSL) resulting in the emission of shorter wavelength (blue) light in an amount proportional to the original X-ray irradiation. In CR, an imaging plate (IP) containing the storage phosphor is positioned in a light-tight enclosure, exposed to the X-ray image and then read out by raster scanning with a laser to release the PSL. The blue PSL light is collected with a light guide and detected with a photomultiplier tube (PMT). The PMT signal is digitized to form the image on a point-by-point basis [3] .
The main advantages of CR include: wider dynamic range (latitude), ability for post processing (manipulation of radiographic contrast and brightness), multiple viewing options, electronic transfer and storage options [4] . The wide exposure latitude of CR means that a greater range of radiation exposures (mainly current-time product (mAs)) can be used to produce a diagnostic image [4] .
Underexposure and overexposure with film-screen radiography (FSR) are associated with poor image quality and the film may need to be repeated; whereas underexposure in CR results in a grainy image (high noise) that could be tolerated with some post processing, and higher than appropriate exposures in CR leading to increasing image quality due to an increase in signal-noise ratio [5] [6] [7] [8] . Gross artefacts are not evident on CR until exposure levels are 100 times lower or 500 times greater than those used in FSR [8] . Thus, while there is a potential for reduced repeat examinations and hence dose reduction in CR, it has been reported that radiographers develop a tendency to use higher than necessary exposure factors to improve image quality and avoid repeat radiographs. This tendency to increase exposure factors is referred to as exposure factor creep [6] .
While FSR allows the radiographer to visually assess whether exposures are optimum, this direct visual assessment is lacking with CR systems. To allow for exposure parameter control and to safeguard from overexposure in CR, manufacturers have introduced numerical parameters that are a direct estimate of the incident exposure on the imaging plate [7] . Each manufacturer provides its own ‘‘exposure indicator’’, with an algorithm for its calculation; for example, this is called the exposure index (EI) by Kodak [8] and sensitivity (S) value by Fuji [9] .
2. Material and Method
2.1. X-Ray Unit
This work was carried out in five public hospitals in Khartoum, Sudan and included five X-ray units. The hospitals are thereafter refereed as: A, B, C, D and E. These hospitals were chosen because they had a considerable number of X-ray examination performed on daily basis.
2.2. Parameters and Calculating of ESAK
To calculate the ESAK, X-ray tube exposure parameters were recorded for each patient undergoing the specified diagnostic procedure: peak tube voltage (kVp), exposure current-time product (mAs) and focus-to-film distance (FFD).
Radiographic projections studied were: Skull AP/PA and Skull LAT, Chest PA, Lumbar Spine AP, Lumbar Spine LAT and Pelvis AP. The ESAK (Ki) is defined as the air kerma to air on the X-ray beam axis at the point where the X-ray beam enters the patient or a phantom, including the contribution of the backscatter. The ESAK was calculated in the present work using the following relation [10] [11] :
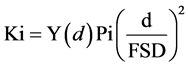
where Y(d) is the tube output per mAs measured at a distance of 100 cm from the tube focus along the beam axis at different kVp different mAs values typically encountered in the clinical practice. Pi is tube current exposure time product (mAs). kV is peak tube voltage recorded for any given examination, mAs is the tube current-time product, FSD is the focus-to-surface distance is a backscatter factor for a particular examination at the required potential, taken from UK Health Protection Agency HPA (previously NRPB) numerical simulations [12] .
2.3. Patient Samples
A total of 408 patients were examined in five hospitals in Khartoum state, patients undergone of one of the selected exams Skull, Chest, Lumber spine and Pelvis. The data were collected using a sheet for patients in order to maintain consistency of the information. The (collected data included) following parameters were recorded age, weight, height, Body Mass Index (BMI) derived from weight (kg)/(height (m))2 and (tube voltage, and tube current-time product setting) exposure parameters were recorded. The dose was measured for four main examinations: Skull AP/PA and Skull LAT, Chest PA, Lumbar Spine AP, Lumbar Spine LAT and Pelvis AP. The examinations were collected according to the availability.
3. Results and Discussion
Doses were calculated in regard to 408 patients with Radiographic projections studied were: Skull AP/PA and Skull LAT, Chest PA, Lumbar Spine AP, Lumbar Spine LAT and Pelvis AP using measured tube output data and the patient specific exposure parameters. All X ray equipment for which doses were measured were properly maintained, checked as part of quality control program and were found to perform according to specification.
The data show the number of patients from five public hospitals in Khartoum, Sudan and included five X-ray units. The hospitals are thereafter refereed as: A, B, C, D and E. And the number of patients for each exam was 182,125,172 and 129 for skull, chest, lumber spine and pelvis examinations respectively.
For all examinations here the FFD for skull AP/PA and Skull LAT, Lumbar Spine AP, Lumbar Spine LAT and Pelvis AP was in range 100 to 120cm and for Chest PA was 180 cm.
The mean and ±SD values of all the patients examined to skull X-ray were presented in Table 1. Study population Comprised 125 adult’s patients (50% for each male and female) patient age ranged from 28 - 70 years, Body Mass Index ranged from 18.54 to 26.67 kg∙m2 with mean ± SD 22.8 ± 3.26 kg∙m2, and ESAK ranged from 0.588 to 3.303 mGy, with 1.704 ± 0.682 mGy, and for Effective Dose 0.141 ± 0.057 mSv and ranged from 0.048 to 0.274 mSv.
The mean and ±SD values of all the patients examined to chest X-ray were presented in Table 1. Study population Comprised 180 adult’s patients (52.6% for male and 47.4% female) patient age ranged from 16 - 88 years, Body Mass Index ranged from 19.02 to 27.123 kg∙m2 with mean ± SD 25.54 ± 12.64 kg∙m2, and ESAK ranged from 0.031 to 2 mGy with the mean ± SD 0.290 ± 0.244 mGy, and for Effective Dose 0.023 ± 0.018 mSv and ranged from 0.002 to 0.0138 mSv.
The mean and ±SD values of all the patients examined to lumber spine X-ray were presented in Table 1. Study population Comprised 172 adult’s patients (64.8% for male and 35.2% female) patient age ranged from 21-88 years, Body Mass Index ranged from 19.03 to 26.53 kg∙m2 with mean ± SD 23.25 ± 1.93 kg∙m2, and ESAK ranged from 2.05 to 5.15 mGy with the mean ± SD 3.15 ± 1.58 mGy, and for Effective Dose 0.127 ± 0.067 mSv and ranged from 0.087 to 0.365 mSv.
The mean and ±SD values of all the patients examined to pelvis X-ray were presented in Table 1. Study population Comprised 129 adult’s patients (58.7% for male and 41.3% female) patient age ranged from 21 - 85 years, Body Mass Index ranged from 21.88 to 36.88 kg∙m2 with mean ± SD 24.13 ± 4.34 kg∙m2, and ESAK ranged from 1.05 to 4.402 mGy, with 1.53 ± 0.814 mGy, and for Effective Dose 0.127 ± 0.067 mSv and ranged from 0.087 to 0.365 mSv.
![]()
Table 1. Patient demographic data and patient radiation doses during examinations of X-ray.
Table 2 shows statistical parameters in four for ESAK mean, median, STD, minimum, maximum and third quartile for all patients with different X-ray examinations according to gender, gender and statistical parameters including mean, median, STD, minimum, maximum and third quartile for ESAKs.
Table 3 shows statistical descriptive of ESAK mGy depending on the exam projection, statistical parameters Mean, Median, standard deviation, minimum, maximum and third quartile of ESAK mGy was used to Skull AP/PA and Skull LAT, Chest PA, Lumbar Spine AP, Lumbar Spine LAT and Pelvis AP.
Compared between present study with international study and international organization, the ESAK found in this study was lower than that reported by International organizations. However, the results compared with some establishing international dose reference dose levels such as IAEA, CEC in Table 4.
![]()
Table 2. Standard deviation for ESAK in mGy according to gender.
![]()
Table 3. Show descriptive statistic of ESAKD (mGy) in all hospitals according to exam projection.
![]()
Table 4. Compression of this study with international studies and IDRLs [13] [14] [15] [16] [17] .
List of Symbols and Acronyms: ESAK: Entrance Surface Air Kerma; CEC: Commission of the European Communities; IAEA: International Atomic Energy Agency; NRPB: National Radiological Protection Board; BMI: Body Mass Index.
However, the risk from radiation exposure of the patients must be balanced versus the diagnostic benefit. Many departments do not use recommended radiographic parameters for patient using digital radiography, furthermore, wide variations in the applications of the radiographic techniques, equipment performance at different hospitals over the world.
4. Conclusions
The patient dose was measured in five large hospitals for different computed radiography modalities. The findings from the present study showed that optimization of technical and clinical factors may lead to a substantial patient dose reduction.
The results of this study allow a better understanding of how different working habits and examination technology influence the patient doses and make medical staff aware of their responsibility for optimization of daily radiological practice.
For all the examinations studied in the hospital, the mean ESAK values obtained are found to be within the standard reference values of doses.
Reference dose levels for diagnostic radiology must be established on the national scale, in order to reduce the patient exposure and to maintain a good diagnostic image.