Fasting for Laboratory Tests Poses a High Risk of Hypoglycemia in Patients with Diabetes: A Pilot Prevalence Study in Clinical Practice ()
1. Introduction
Lipid profiles are conceivably the most commonly used laboratory tests that traditionally require overnight fasting. Since patients with diabetes, especially type 2 diabetes mellitus (T2DM), have a high prevalence of lipid abnormalities [1] , these patients expectedly undergo frequent lipid testing. Conceivably not originally based on compelling evidence, the current, deeply-rooted, practice of fasting for lipid profiles as recommended by current guidelines [2] , has been recently challenged [3] - [9] . As important, there is an emerging discussion about the atherogenicity of postprandial hypertriglyceridemia, which can be missed in fasting lipid profiles [5] - [13] .
In addition to the inconvenience and questionable necessity of fasting for lipid profiles in clinical practice, there is ongoing discussion regarding the safety of such fasting in patients with diabetes [7] [9] - [13] . As recently reported, patients with diabetes on hypoglycemic medications are especially vulnerable to fasting that can increase their risk for hypoglycemia especially if they are not adequately prepared for fasting [10] - [12] . Specifically, patients with diabetes who use insulin or sulfonylureas are put at increased risk for hypoglycemia when fasting [10] - [13] . Whereas patients who are not taking hypoglycemic medications (i.e., insulin and insulin secretagogues) are protected by a complex physiological response that inhibits insulin production by the beta cells during fasting, patients taking such medications typically do not have such a protective mechanism in view of continued circulating insulin [10] . This risk is further aggravated in patients with long-standing diabetes due to the loss of additional counter-regulatory mechanisms that protect from hypoglycemia during fasting, i.e., glucagon and catecholamines [12] - [15] .
We recently described a “novel” form of hypoglycemia referred to as Fasting-Evoked En-route Hypoglycemia in Diabetes or FEEHD [9] [11] - [13] . FEEHD as defined herein is diagnosed by the following criteria: Documented hypoglycemic event (blood glucose below 70 mg/dL) in patients with diabetes who take insulin or sulfonylurea, or both, who fast overnight for lab tests (and thus miss or delay breakfast), and who commute to the laboratory facility while fasting. The condition in a broader term can be applied to any fasting-related hypoglycemic event in patients with diabetes who are taking hypoglycemic medications (e.g., occurring at home or elsewhere). We restricted the definition in the acronym to reflect this “en-route” circumstance. This terminology, thus, highlights the risk of this form of hypoglycemia that can potentially occur during driving to and from the laboratory for blood testing. This poses a significant threat given that hypoglycemia during driving has been shown to impair performance and lead to traffic accidents [16] .
To our knowledge, the morbidity or mortality associated with FEEHD has not been studied, and we believe that this might be due to under recognition and under reporting [9] - [13] . However, upon more meticulous literature search, we came across one case report of laboratory-associated hypoglycemia from Thailand, which reported on a patient who died in the laboratory waiting room, while waiting for a fasting lab test [17] . She was reportedly on sulfonylurea and her blood glucose was reported as 0 (zero) mg/dL. Unlike FEEHD, however, diabetes-associated hypoglycemia and associated morbidity and mortality have been well-studied as being the “major limiting factor in diabetes management” [14] [15] .
While FEEHD has been described recently in two small studies [10] [11] and a case series [12] , the exact prevalence of FEEHD remains largely unknown. Thus, we hypothesized that this form of iatrogenic hypoglycemia is widely prevalent in clinical practice but judging from the dearth of reports is greatly under recognized. In this pilot study, we set out to evaluate the prevalence of FEEHD in a real life clinical setting.
2. Materials and Methods
This study was approved by Michigan State University’s (MSU) and Sparrow Hospital’s Institutional Review Boards. Informed consent was obtained from all participating patients. Patients were recruited from multiple clinics, as detailed below.
2.1. Selection of Patients
The study was conducted at four clinical sites: three MSU and Sparrow Hospital teaching clinics: Internal Medicine, Family Medicine and Endocrinology (Diabetes) clinics, in East Lansing and Lansing, Michigan, and The Care Free Clinic, a non-for-profit family medicine clinic for the underserved in Lansing, Michigan. The selection of the aforementioned clinics was made at random: Those were the fairly diverse set of clinics that data collectors (residents or students) happened to have access to at the time.
Inclusion criteria included adult patients who: were able to understand and answer the survey questions; had a confirmed diabetes diagnosis; and who were taking insulin and/or oral hypoglycemic agents (OHA’s) or non-insulin injectable medications. Exclusion criteria included: patients who were unable to understand or complete the survey questionnaire even with assistance; patients who were not taking medications regularly; and surveys that were not completely filled.
2.2. Study Design
The study was conducted from October 2014 to October 2015. The research protocol consisted of a two-page written survey that was offered to patients attending the participating clinic sites. Patient inclusion and exclusion criteria were determined by data collectors: attendings, fellows, residents, medical students or by research-dedicated medical assistants (MA) in the clinics. Once a potentially eligible patient was identified, the MA would either complete the study enrollment using a pre-signed survey or would ask a non-MA data collector to enroll the patient.
If a participant expressed reluctance to complete the survey because of time constraints, he or she was given the option to complete the questionnaire at home and mail it to the clinic.
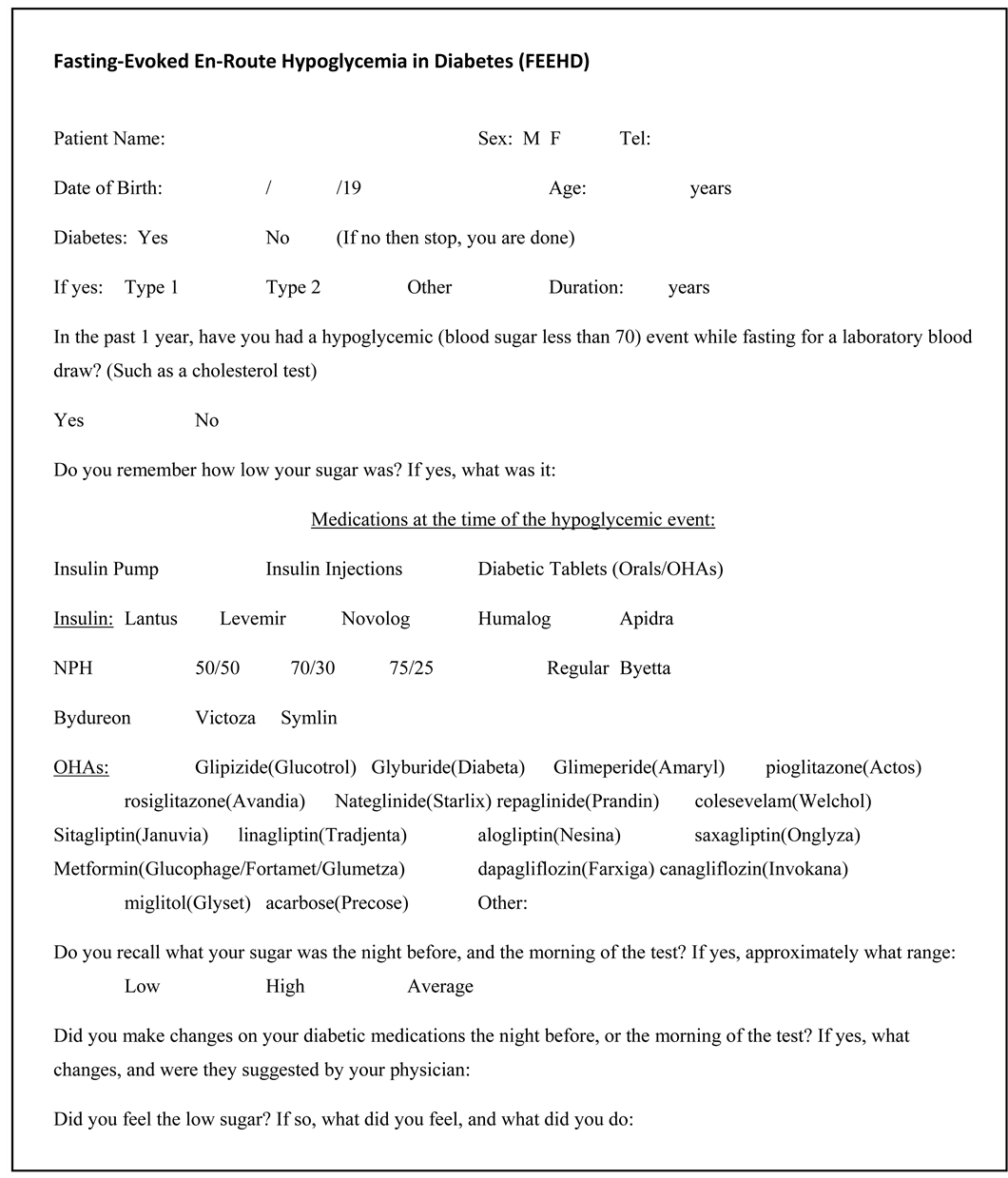
2.3. Survey Questionnaire
The survey questionnaire was designed by the study investigators. It is a simple, customized survey tool that was adapted from original questionnaires used in prior studies [10] [11] , which were preliminary questionnaires intended strictly to help obtain raw information from patients to collect data in a structured manner about hypoglycemic events and circumstances thereof. The questionnaire had not been validated in prior studies, and was not intended for sophisticated larger-sample statistical analysis. Thus, the reliability of the questionnaires was not validated but was utilized in this pilot study as a facilitator in data collection.
The customized questionnaire used in this study (shown in Appendix)is a two-page simple-language survey which included, in addition to demographics and clinical info, specific questions about the number of fasting lab tests, the number of hypoglycemic events in general and the number and circumstances of FEEHD events. Hypoglycemia in patients with FEEHD was defined similar to the definition of diabetes-associated hypoglycemia in general, that is blood glucose below 70 mg/dL, as defined in the literature [15] . All specific questions about hypoglycemic events were limited to the preceding 12 months. At the end of the survey, a template notification was made to instruct patients to notify their care providers of any hypoglycemic events to implement preventive measures.
2.4. Statistical Analysis
For this pilot study, the investigators had opted to avoid trying to conduct any pre-hoc minimal sample size calculations due to the largely unknown characteristics of the anticipated patient samples across the clinic settings. Survey questionnaires were then reviewed and entered into Excel spreadsheets and a series of cross tabulations were generated to examine for statistically significant sample subgroup differences. During Chi-square calculation and analysis of variance (ANOVA), procedures were completed with complete data sets. Variables tested to evaluate correlations with patient characteristics and the occurrence of FEEHD episode(s) included: a) clinic type (i.e., Diabetes versus other primary care clinics); b) sex; c) total number of FEEHD-associated medications taken during year; d) type of diabetes; e) duration of diabetes; f) number of reported all-cause hypoglycemic episodes during the prior year; and g) total number of fasting lab orders issued during the prior year. Finally, a series of conservative forward stepwise binary logistic regression procedures free of parametric assumptions were completed to examine for categorical factors and continuous covariates that were significantly associated with the occurrence of hypoglycemic episodes(s).
3. Results
One hundred sixty-eight patients consented to participate in the study, of whom 166 patients completed the surveys in the clinic, and 2 patients took the survey to be completed at home. After the exclusion of 2 patients who did not complete the study surveys, a final sample of 166 respondents was achieved. The mean age of patients was 55.3 years (SD 15.4), and diabetes duration averaged 16.7 years (SD 12.3). A total of 79 (47.6%) patients were females, and 119 (71.7%) reported having been diagnosed with T2DM (Table 1).
In regards to current medication regimen, 24 (14.7%) reported taking one or more OHA’s only; 58 (34.9%) reported taking insulin or other injectable medications with no OHA’s; and 83 (50.0%) patients reported taking both types of medications. Patients indicated having received a mean of 2.4 (SD 21.7) fasting lab orders during the past 12 months. A total of 103 (62%) of patients reported having experienced between one and four all-cause hypoglycemic episodes during the past year.
![]()
Table 1. Descriptive characteristics of patients and results of key questions in the study’s survey questionnaire.
Abbreviations: SD = standard deviation; FEEHD = fasting-evoked en-route hypoglycemia in diabetes; OHAs = oral hypoglycemic agents.
Of the 166 sample patients, 45 (27.1%) patients reported having one or more lab- related FEEHD hypoglycemic events during the past 12 months. Within this sample subgroup, 39 (86.7%) patients could recall at least one specific circumstance related to their FEEHD episode(s). These included (frequently overlapping) reasons such as: 1) fasting/eating less during prior night (33%); 2) exercising (4%); 3) recent medication changes (3%); and 4) multiple cited reasons (19%). Notably, only 31.1% of patients who experienced FEEHD clearly indicated that they had advised their providers of the event. Of concern as well, only 40% of FEEHD events reportedly resulted in any subsequent provider medication change(s).
Major non-significant correlations with patient characteristics and FEEHD episode(s) during prior 12 months included 1) clinic type (Pearson r = −0.069, p = 0.378); 2) gender (r = 0.012, p = 0.882); 3) total number of FEEHD-associated medications taken (r = 0.083, p = 0.292); and (4) total number of fasting lab orders received during prior year (r = 0.000, p = 0.999). On the other hand, patient characteristics that were significantly correlated with experiencing one or more FEEHD episode during the prior 12 months included: 1) type of diabetes (r = −0.175, p = 0.026); 2) duration of diabetes (r = 0.173, p = 0.042); and 3) number of reported all-cause hypoglycemic episodes during the prior 12 months (r = 0.305, p =< 0.001). In summary, T2DM; diabetes duration for 11 or more years; and/or multiple all-cause hypoglycemic episodes were more likely correlated with experiencing one or more FEEHD episode(s) during the prior 12 months.
Furthermore, variables such as age category (p = 0.758), gender (p = 0.568), clinic type (p = 0.685), number of prior annual fasting labs during prior 12 months (p = 0.761), and total number of FEEHD-associated medication(s) taken during prior year (p = 0.779), each with score test statistics of p > 0.10 were removed from later models. In the final logistic regression model, only one covariate demonstrated statistical significance: The frequency of all-cause hypoglycemic episodes during prior 12 months (p = 0.014). Of note, patients’ categorical diabetes duration just barely fell out of statistical significance (p = 0.054). Table 2 summarizes the variables as predictors of FEEHD events.
Finally, the study was not designed to evaluate for possible association of FEEHD with factors that could influence the risk of hypoglycemia, including medications types or doses; comorbidities such as liver or kidney disease; the duration of the fasting; etc. The whole mark of the study design was the fasting itself (and skipping a meal), being iatrogenic and a known major cause of hypoglycemia in patients on hypoglycemic medications (insulin and sulphonylureas).
4. Discussion
This study supports the hypothesis that FEEHD occurs in clinical settings with a surprisingly high prevalence (27.1%). To our knowledge, this is the first study to evaluate the prevalence of FEEHD in clinical practice. In our previous studies [10] [11] , study designs did not allow for prevalence calculation. While we cannot necessarily extrapolate
![]()
Table 2. Predictors of FEEHD event(s) during 12-month pre-survey period* (N = 166 adult patients).
Abbreviations: FEEHD = fasting-evoked en-route hypoglycemia in diabetes; Exp (B) = the Exp (B) is equivalent to the “Odds Ratio” with numbers less than 0.500 representing less than 50% likelihood of a FEEHD occurring (e.g. the 0.402 for patients with diabetes duration of 1 - 11 years) versus more likely (e.g. patients with 11 - 20 years of diabetes (1.581)―about one and a half more likely) of experiencing one or more FEEHD event(s). In other words, patients with longer history of diabetes were generally more likely to experience a FEEHD event, although not quite significantly (p = 0.054). *Patients may have experienced mare than one FEEHD event during 12-month study window; **Categorical variable; ***Continuous variable.
these findings to other clinical settings, we believe that FEEHD is likely to be quite highly prevalent in clinical practice, but is perhaps under recognized. Considering 70 mg/dL as the cut off for diabetes-associated hypoglycemia [15] , the severity of hypoglycemia reported by patients who recalled the exact glucose measurement ranged from 30 to 69 mg/dL. Of concern, 10 patients reported FEEHD events below 50 mg/dL and five patients reported events below 40 mg/dL, with variable reported hypoglycemic symptomatology.
FEEHD is a recently recognized circumstantial category of hypoglycemia [7] [9] - [13] that is largely preventable. More concerning is that it is primarily iatrogenic. Hypoglycemia, described by Fowleras being “in many ways the Achilles heel of diabetes treatment”, is the major limiting factor in diabetes management [14] , with significant morbidity and mortality [15] . It is conceivable that diabetes-related hypoglycemia is a heterogeneous, multifactorial and complex condition. Multiple factors interplay to precipitate hypoglycemia in patients with diabetes, such as carbohydrate intake, medications, physical activity and comorbid conditions―but the common denominator is a net imbalance between medications (mainly insulin or sulfonylureas) and carbohydrate intake. The American Diabetes Association’s (ADA’s) practice guidelines emphasize the importance of teaching patients to balance insulin use, carbohydrate intake and exercise, adding that these strategies are not always sufficient to prevent hypoglycemia [1] .
FEEHD is such a circumstance of a skipped meal that is imposed on patients by their caregiver; ordering fasting labs in patients with diabetes, without educating them to adjust their anti-diabetic medications, and to perform more glucose monitoring while fasting. More concerning, our study demonstrated that less than one-third of patients informed their clinicians about the occurrence of FEEHD and only 40% of patients had implemented strategies to prevent future FEEHD episodes. Although this iatrogenic form of hypoglycemia has been reported since 2011, currently there are no guidelines related to FEEHD [7] [9] - [13] . However, to increase awareness about FEEHD, the results of the published studies were communicated to the ADA via the online portal for public proposals suggesting the education of patients about FEEHD in the practice guidelines. As a result, in 2012 the ADA provided [18] an addendum to the thereto guidelines (2011) in the “Hypoglycemia” section [19] , to include the following statement: “Patients should understand situations that increase their risk of hypoglycemia, such as fasting for tests” [18] .
However, this statement would need to be implemented with various educational routes to clinical practice. Moreover, current investigators have now implemented a preventive program [11] in their clinic (attempting to streamline the fasting pre-requisite for lipid profiles, the principal lab test requiring fasting). The preventive program also implemented educational instructions for patients who are; nevertheless, requested to fast for any labs, explicitly describing medication changes and frequent glucose monitoring [11] .
We had conducted a previous study after implementing the above preventive program and did a retrospective design comparing two groups of patients, one with the teaching intervention and one without. The study demonstrated a significant reduction of FEEHD in the group that received instruction prior to fasting for blood testing. Hypoglycemia was reduced by over 50% in the glucose levels of 70 mg/dL, 88% for 50 mg/dL and 100% below 40 mg/dL [11] .
Two major concerns regarding FEEHD need to be emphasized:
Many patients do not have a clear understanding of hypoglycemia, and physicians do not seem to track the frequency of hypoglycemia in their patients. Thus hypoglycemia is conceivably underreported, as emphasized by Moghissi [20] and by Skarulis and Hirshberg [21] that hypoglycemic events are often underreported by patients to their clinicians.
Diabetes-associated hypoglycemia occurring during driving has been reported to occur in 19% of T2DM in a national survey report [20] . A growing concern is emerging in regards to hypoglycemia and driving [14] [22] - [25] . The ADA’s practice guidelines emphasized that “severe hypoglycemia can cause acute harm to the person with diabetes or others” [1] . Also, there is an emerging concern of litigation regarding hypoglycemia and traffic accidents [25] . Currently, we are not aware of reported cases for FEEHD occurring while driving, but there is a potential risk of this occurrence, and there is a concern of underreporting of such cases.
In parallel to this discussion, it is prudent to emphasize that in clinical practice lipid profiles are the commonest lab tests requiring fasting, including in patients with diabetes. Coincidentally, recent compelling literature has cast a doubt on the necessity of fasting for lipid profiles, altogether [3] - [13] [26] - [33] which is a stark departure from a decades-long tradition. But still, most national and international guidelines continue to recommend fasting for lipid profiles [2] [30] - [33] . This is despite the compelling evidence that fasting is not only unnecessary for lipid profiles [6] [8] [30] - [33] , but in addition studies have shown that non-fasting lipid profiles are probably more relevant as predictors of cardiovascular disease [8] [26] [27] . Numerous studies have found that nonfasting lipids are not inferior to fasting, as cardiovascular disease predictors [32] .
Interestingly, this deeply-rooted tradition of fasting for lipid profiles is slowly changing, however. In the US, most organizations continue to recommend fasting for lipid profiles for initial evaluation and monitoring of lipid status. However, over the last decade guidelines have evolved with more guidelines recommending that non-fasting measurement of total and high-density lipoprotein (HDL) cholesterol could be alternatively utilized, the so-called Non-HDL cholesterol [32] . Furthermore, the American Heart Association in its 2013 guidelines [32] emphasized that while the guidelines prefer fasting but fasting is not considered mandatory, nevertheless [32] . As a recent departure from the tradition of routine fasting, a recent Veterans Affairs’ guideline explicitly recommended against fasting for lipid tests, except when triglycerides exceed 400 mg/dL [28] . Similarly, The Danish National Society of Clinical Biochemistry’s Guidelines, now recommends non-fasting lipid profiles, with “the possibility of” ordering a fasting test if the nonfasting triglycerides level is over 350 mg/dL [29] , More explicitly, Langsted and Nordestgaard (lipid experts from Denmark) recently published an editorial in the journal, Chemical Chemistry, in which they stated that “nonfasting lipid profiles are the way of the future” [30] .
An entertaining example of how this issue is still being debated, at present, can be seen in a Q&A article recently published in the journal of Clinical Chemistry [31] , in which six international lipid experts were interviewed. The experts were each asked a set of questions about the issue of fasting versus nonfasting lipid testing. On the final question “Do you personally believe that nonfasting samples should be used for routine lipid profiles?”, four experts said “yes” and two said “no”, with diverse elaborations!
Most recently, the most powerful step towards the push for nonfasting lipid profiles, so far, has been taken by an international expert panel (21 experts including 3 from the US) convened by the European Atherosclerosis Society and the European Federation of Clinical Chemistry and Laboratory Medicine, which developed a joint consensus statement, simultaneously published ahead of print in two major medical journals [33] . The consensus statement, stated that “Fasting is not routinely required for determination of a lipid profile”, and proposed cut-point values for nonfasting lipid components to be flagged by laboratories.
The primary limitations of this study include a sample size that is small; lack of exact calculation of survey response rate; data that is acquired based on patients’ recollection of the hypoglycemic events and glucose measures; a survey questionnaire that did not include the type of tests for which fasting was requested. Finally, the study did not address if patients were driving themselves to and from the laboratory nor if FEEHD events caused traffic accidents. However, despite these limitations, this pilot study can serve as an initial step in bringing attention to this serious and often overlooked management problem in patients with diabetes. We suggest larger population-based studies be performed to evaluate the prevalence of FEEHD.
5. Conclusion
This is the first prevalence study to evaluate the prevalence of FEEHD in clinical practice. The high prevalence (27.1%) noted in this study is quite alarming, and as alarming is the apparent unawareness of this iatrogenic problem amongst clinicians. Although this is a pilot, non-randomized study, and despite the study’s limitations, it is hoped that this pilot study triggers further studies of larger samples and improved designs to address the prevalence of FEEHD in other clinical settings and in the population. Finally, it is hoped that health organizations, especially diabetes organizations, take a note of this issue and develop specific educational guidelines to prevent FEEHD.
Acknowledgements
The authors would like to thank Ms. Jinie Shirey (Department of Medicine, MSU College of Human Medicine, East Lansing, MI) for assistance with manuscript preparation; Dr. Christie Clipper (Healthy Edge, Ann Arbor, MI) for revision of the manuscript; and senior librarians Laura Smith, Michael Simmons and Steve Kalis (Sparrow Hospital, Lansing, MI) for assistance with literature search. The authors also would like to thank the clinical and support staff at all clinical sites for facilitation of the study conduction, and finally to thank all patients who participated in the study.
Author Disclosure Statement
SA: Speaker for Janssen Pharmaceutical and Sanofi Pharmaceutical.
GA: Speaker for Merck, Amgen and Diiachi Sankyo. He served as a consultant to Kowa Pharmaceutical. He was a participant at Merck’s US Thrombosis Advisory Board and Atherosclerosis Global Therapeutic Experts Forum and he has received grant support from Merck.
SM: Research support from Atherotech Diagnostics and NHLBI. She served as a consultant to Amgen, Quest Diagnostics, Lilly, Pfizer, and Cerenis Therapeutics.
Other co-authors: No conflict of interests.
Funding
None.
Authors Contributions
SA: Designed study; wrote/revised manuscript.
WC: Participated in study design; analyzed data; reviewed manuscript.
GA: Contributed to discussions; revised manuscript.
SM: Contributed to discussions; revised manuscript.
KS: Collected data; reviewed manuscript.
PK: Collected data; reviewed manuscript.
FB: Participated in study design; collected data; reviewed manuscript.
AH: Participated in study design; collected data; reviewed manuscript.
DG: Participated in study design; reviewed manuscript.
Appendix
IRB-approved Survey Questionnaire, Page 1:
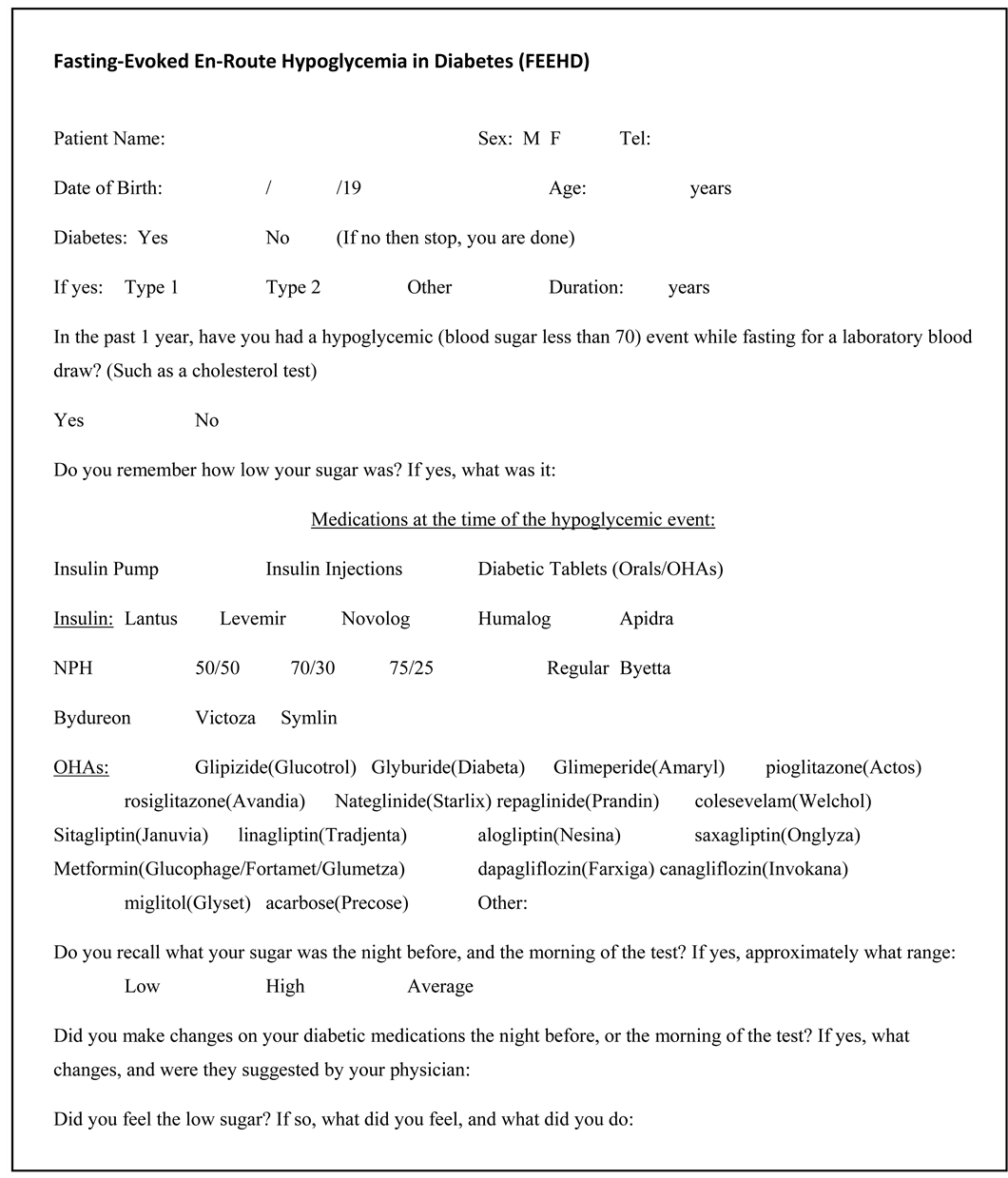
IRB-approved Survey Questionnaire, Page 2: