Analysis of Bone Quality on Panoramic Radiograph in Osteoporosis Research by Fractal Dimension ()
Received 27 November 2015; accepted 14 March 2016; published 17 March 2016

1. Introduction
Osteoporosis is a major health problem and affects a significant number of people. This skeletal disorder is characterized by bone fragility due to deterioration of the bone micro-architecture, which confers strength and bone quality; this can increase the risk of risk and is associated with certain serious complications resulting in death [1] [2] . Screening for osteoporosis is currently recommended for all women aged 65 years or older. The complications of this disease may be prevented by early detection [1] . Diagnosis is currently based mainly on measurement of bone mineral density (BMD) using dual-energy X-ray absorptiometry (DXA) considered as “gold standard”, but bone densitometry is expensive and has limited availability for routine use in population screening [3] [4] .
Several studies have demonstrated that individuals with osteoporosis have altered morphology of the mandible and there is evidence that intraoral and panoramic radiographic findings might be indicators of osteoporosis [1] [5] -[10] . The BMD of the mandible is correlated with that in the lumbar spine and femoral neck in osteoporosis [7] .
Panoramic radiography (PR) is highlighted in this context because it is frequently conducted in the dental office; it is rapid and low-cost and uses low-dose X-radiation. The most commonly studied measure of mandibular morphology in relation to osteoporosis is the integrity of the inferior border. Erosions of the inferior border are typically scored using the mandibular cortical index (MCI) [9] . This index (known as the Klemetti index) [11] developed for PR in a study in which the authors concluded that individuals with osteoporosis is also more likely to show erosions. They suggested that this evaluation is useful for identifying postmenopausal women with undetected low skeletal BMD or osteoporosis.
One of the most common bone patterns is trabecular bone. Trabecular bone has a branching pattern, as seen in this vertebral specimen. The idea that the fractal index or fractal dimension (FD) of trabecular bone might be related to bone strength is an appealing one, since the fractal index is simple to calculate from clinical radiographies [12] [13] . Thus, the aim of this study was to assess the correlation between different quality analysis parameters of trabecular pattern in digital panoramic radiographies and relations with forearm bone density performed by pDXA in Brazilian population.
2. Material and Methods
Initially the sample consist in 78 panoramic radiographs (PR), but only 68 of these patients had the BMD tests, by pDXA, for this reason our sample was limited to 68 patients, 9 males and 59 females (19 - 73 years old). The digital panoramic radiographs had been gotten in a Veraviewepocs device of J. Morita MFG. CORP.
2.1. Trabecular Pattern Analysis
The trabecular bone pattern study was done using the morphological analysis methodology proposed by White et al. (2000) [14] . For this analysis we used the NIH ImageJ (National Institutes of Health, Bethesda, MD) software. Thus, was performing measurements of the morphological factors of trabecular architecture in the digital panoramic radiographs.
First of all was selected the region of interest (ROI). It was selected the rectangular selection tool, a fixed manner, in the dimension of 230 × 130 pixels located in the region of the mandibular body below the lower canine tooth apex, always on the right, avoiding overlapping anatomical structures, as the mental foramen, Genis apophyses and regions of masticatory stress (premolars and molars) [15] . Thus, it was cut the same size rectangular pictures in all PR [16] (Figure 1).
In Image J software (National Institutes of Health, Bethesda, MD) to analyze the images and possibilities for changes in trabecular pattern of the ROI. The following steps were followed [14] : 1) ROI image duplication; 2) Image blurring (From Gaussian) with 33 radius (pixels)―this step remove all the fine and medium scale structures and retains only large variations in density (low-pass filter); 3) Image subtraction―The blurred image was subtracted from the original of the same patient; 4) Adding―This operation adding a constant to each pixel of the result subtracted image. This generates an image with an average value of about 128, regardless of the original image intensity, discarding gross variations in the intensity RP; 5) Binary transformation―The previous image was transformed into binary image that is black and white; 6) Erode―The previous result was “eroded”. Each pixel is placed with the minimum value of your neighborhood; 7) Dilate―Previous result was “dilated”.
![]()
Figure 1. The region of interest (ROI) selected the images of digital panoramic radiographs, in the region of the mandibular body, before the mental foramen and after the mental area, usually in the apical region of the tooth 33/43.
Each pixel is loaded with the maximum value in the vicinity 3 × 3; 8) Inversion―The image of the previous result was reversed. Similar to a photographic negative; 9) Skeletonized―It was removed edges of the pixels of the binary-object-dilated-eroded-inverted images until they were ducted to a single wide skeleton of a single pixel. The object (trabecular) is black and background is white (Table 1).
The skeletonized images from each patient were then saved in TIFF format. Using the same software Image J performed the analysis of the images as follows: Analyze particles-Analysis of the trabecular area checking the average size of trabeculae (particles), TMP, and the number of trabeculae different sizes (particles), DTP. These values represent the connectivity of the trabecular meshwork. The higher the value of TMP and the smaller the value of the DTP, greater trabecular bone connectivity of ROI. To facilitate the analysis of those parameters did a ratio using the following equation:
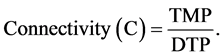
The second analysis in the same image was by histogram. Thus, evaluating the total number of “bright” pixels (black) in the binary image of the ROI in terms of percentage, called ET.
The third analysis was Fractal Box Count. This analysis provides us with the value of “D” called FD or fractal dimension. Boxes were used in the following sizes 2, 3, 4, 6, 8, 12, 16, 32, 64.
2.2. Bone Mineral Density Measure (BMD)
The peripheral bone densitometry measurements of absorption by dual energy X-ray absorptiometry (DXA) were carried out in the apparatus of Norland, pDXA determining the bone mineral density of the forearm to identify who has a high risk of osteoporosis. The region of choice for scanning and harvesting of data for risk assessment osteoporosis was the distal forearm [17] . The scanning resolution was 1.00 × 1.00 mm , prior to scanning. The radiation dose was less than 0.03 mSv for each examination.
2.3. Statistical Analysis
The statistical analysis was performed by the GMC program, version 2002, Biological Research. In addition to verifying the normality tests were performed Pearson.
3. Results
The sample was 78 panoramic radiographs, but only 68 of these patients had the BMD tests, by pDXA, for this reason our sample was limited to 68 patients, 9 males and 59 females. It should be noted that WHO has no reference data for densitometry measurements for man even so they were considered.
BMD measurements of the total sample based on T-score value for the three sites and the average of these
![]()
![]()
Table 1. Methods of digital image processing, for skeletal samples from each patient.
values for each patient. It may be noted that only 26 patients have correlation between the three values: Proximal radio = osteopenia, proximal radius plus ulna = osteopenia and distal of radius plus ulna = osteopenia, or 38.2% of the sample (Table 2). HORNER et al. 2002 [10] considered that any measure with standard deviation below or equal to −1 classify the patient in the group of patients with low bone mass, or possessed of some risk for osteoporosis, and consequently the fracture risk.
The correlation was made between the tested parameters, performing the Pearson correlation tests to verify the correlation coefficient between the variables associated and the statistical significance of the possible relationship (Table 3). For the FD values, higher values, the greater the complexity of the structure analyzed in this work, the mandibular ROI [18] .
In Table 4 displays have skeletonized ROI samples for each patient and the respective FD, ET and TMP/DTP values. Each patient has a representative color classification by DXA, according to HORNER et al. (2002) [10] , who classified the patients in healthy (green) and with osteoporosis possibility (yellow and red).
![]()
Table 2. Classification of patients according to the measurements of bone mineral density (BMD) by pDXA.
Color significance according to pDXA graphics exam: green = healthy; yellow = medium risk to osteoporosis or osteopenia and red = high risk to osteoporosis.
![]()
Table 3. Summary results of correlation tests.
FD: fractal dimension; ET: percentage of black pixels (trabeculae); TMP/DTP: average size ratio and different particle sizes (connectivity); BMD: bone mineral density average.
It was also performed the Cohen’s kappa test to evaluate the correlation between the sample data (trabecular morphology, FD-ET-TMP/DTP and BMD. This analysis was based on the visual observation of the ROI and the mean values of the parameters analyzed. We consider the following parameters: FD lower than 1.4500―unsatis- factory; ET less than 8.00%―unsatisfactory; TMP/DTP lower than 150―not satisfactory. It should be emphasized that using the mean values of the ratio of TMP/DTP, does not reach 500, considered approximately 1/3 of this value, so there is no risk of overestimation, since it represents the connectivity samples. Thus, this parameter had significant weight on visual observation of the ROI.
4. Discussion
Bone quality may be underestimated when based on trabecular bone density due to increase of radiographic density and which has no correlation with the state of bone mineral skeleton. The contributions of soft tissue as much as kVp, exposure time, mA and a different image receptors affect the radiographic outcome. The method used to evaluate the cortex morphology are less susceptible to these types of errors [19] , as recommended morpho-digital studies of trabecular bone pattern [9] [14] [20] -[28] . Therefore, it may be more reliable, perform the evaluation considering the appearance of the cortex in the panoramic radiography, examining the trabecular bone or alveolar process, when, for example, diagnostic analysis of pre-implant bone quality, is required.
White & Rudolf (1999) found sufficient evidence that the trabecular pattern is affected in individuals with osteoporosis, either medium or high risk [29] . We found a significant correlation between the FD factors, ET and TMP/DTP (or connectivity) level of 5% in the Pearson correlation test. Despite the highly significant correlation of FD with ET, however correlation tests showed no significant correlation of BMD, with the analysis parameters of the trabecular morphology.
WHO defines osteoporosis as “a disease characterized by low bone mass and deterioration of bone microarchitecture, leading to increased bone fragility and a consequent increase in fracture risk”. Thus, evaluating the connectivity of trabecular bone is of paramount importance to the dentist, the analysis of the mandibular bone quality. Observation of ROI numbers: 16, 17, 35, 41, 42, 43, 45, 52, 56, 60, 63, 65, 69, 70, 71, 72 e 73, clearly demonstrates a lack of connectivity in the region, therefore, values TMP/DTP very low (less than 100), 72.4% correspond to patients with low bone mass. The no statistical correlation between BMD and TMP/DTP may be due to the samples being not normal or need to improve the size of sample.
SLEMENDA et al. (1996) also had recognized to have modest correspondence enter the values of BMD, in the different skeletal small sites. When consider in set the factor age, the results had been still less satisfactory due to great overlapping between sick people and not sick [30] .
The morphological filter used in this study was similar to that used by Kumasaka (1997) for extracting skeletal pattern of trabecular bone in panoramic digital images, and transformed into binary images with enhanced geometric components [9] [14] [20] . The authors found that the morphology of trabecular pattern in anterior mandible based on radiographic studies, was indistinct, and the digital extraction site by morphological filter has a very clear observation and revealed details before scarce. For this reason the election site to the digital
![]()
![]()
![]()
Table 4. Skeletonized areas of trabecular structures (patients: 1-78).
FD: fractal dimension; % E.T.: percentage of black pixelss; TMP/DTP: proportion between average size of trabeculae (particles) and number of trabeculae different sizes (particles). Green = healthy, yellow = ostepenia, red = osteoporosis, by pDEXA, according to HORNER et al. (2002).
processing of panoramic radiographs images, and used in this study. The ROI chosen because it is free of image artifacts showed in processed images much more details. Thus, the results suggest that images “improved” radiographs with “poor” quality, can show details of trabecular skeletal pattern. It is necessary to define the best binary processing threshold for adequate results. In this study was followed the technique which can be further enhanced. This technique was possible to see the direction, continuation or termination of trabeculae and are extremely useful for the analysis of bone structures, computer-assisted, to determine, for example, the prognosis following surgery, or to assess certain medical treatment [20] [31] .
5. Conclusion
In conclusion, due to easy access to the panoramic radiograph by a dentist, low cost exam, and frequency, this exam has been recommended as routine in dental care for initial evaluation; the professional should conduct visual examinations of the cortex and the standard morpho-digital of their patients, relating them to factors such as body bone mass index, age and sex, for in case of finding predictors of osteoporosis, and discuss with other medical professionals, the patient’s indication for examination of bone densitometry by DXA. The no statistical correlation between BMD and fractal dimension and TMP/DTP may be due to the samples being not normal or need to improve the size of sample.
NOTES
![]()
*Corresponding author.