Comparison of the ICRP 60 and ICRP 103 Recommendations on the Determination of the Effective Dose from Abdominopelvic Computed Tomography ()
1. Introduction
The effective dose is currently deemed to be the best available dose descriptor for quantifying stochastic risks in diagnostic radiology [1] . The factor by which the equivalent dose in tissue or organ is weighted is called tissue weighting factor (WT), which represents the relative contribution of that organ or tissue to the total detriment resulting from uniform irradiation of the whole body. The effective dose is expressed as:
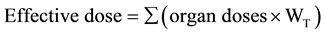 (1)
(1)
where, WT is tissue weighting factor. The unit of the effective dose is Sievert (Sv).
Since the effective dose may be taken as an approximate measure of the stochastic radiation risk, it may be used to quantify the amount of radiation received by patients undergoing diagnostic examinations [2] . Therefore, it is imperative to determine the effective dose obtained from every procedure and also to compare such dose to another obtained using slightly different values in the calculations.
P.K. Sakar stated that the sum of the organ equivalent doses weighted by the ICRP organ―weighting factors, WT, is termed the effective dose, E. And that none of these quantities are measurable nor are they derivable using the laws of physics [3] .
CT scanners have made remarkable advances over the past few years, contributing to the improvement of diagnostic image quality and the reduction of examination time. Computed Tomography represents only 11% of radiologic procedures, but it accounts for as much as 70% of the total effective dose from all diagnostic radiologic studies [4] . However, unlike natural radioactivity which mostly produces non-ionising radiation and is common in the rocks and soils, water and oceans and virtually every material on earth [5] ; computed tomography gives out ionising radiation and the absorbed dose in tissues from CT are among the highest observed from diagnostic radiology (i.e. 10 - 100 mGy).
The International Commission on Radiological Protection (ICRP) is an advisory body providing recom- mendations and guidance on protection against the risks associated with ionising radiation, from artificial sources widely used in medicine, general industry and nuclear enterprises, and from naturally occurring sources [6] .
The International Commission on Radiological Protection (ICRP) was established in 1928 by the Second International Congress of Radiology. At the time, it bore the name, “The International X-Ray and Radium Protection Committee” (IXRPC). It wasn’t until 1950 that the committee reorganized into its present form to more effectively cover the expanding field of radiation protection [7] . The primary goal of the recommendations of the ICRP, as stated in ICRP Publication 103 (2007) is to:
“Contribute to an appropriate level of protection for people and the environment against the detrimental effects of radiation exposure without unduly limiting the desirable human actions that may be associated with such exposure” [8] .
The ICRP 60 report was published in 1991 as an update to ICRP 26 which was published in 1977. It contained several revisions to ICRP 26, including enhancements to the radiation weighting factor and tissue weighting factor methods.
The 2007 recommendations (known as ICRP 103) update the radiation and tissue weighting factors in the quantities of equivalent and effective dose, based on the latest available scientific information of the biology and physics of radiation exposure [9] .
For instance, in the ICRP 60, the tissue weighting factor WT for the gonads is 0.20 and the tissue weighting factor recommended by the ICRP 103 is 0.08.
The ICRP 103 recommendations despite having no changes to the operational quantities and dose limits, attribute changes to the effective dose due to changes to the radiation weighting factor, WR and the tissue weighting factor, WT independent of radiation type. Table 1 shows a summary of tissue weighting factors, WT in ICRP 26, 60 and 103.
2. Methodology
Scanning parameters of 20 randomly selected adults who had a diagnostic abdominopelvic CT scan at a large tertiary hospital in Nigeria using the Toshiba Aquilion 64 CT machine were collected.
The radiographic techniques, together with the measured cross sections of patients, were used to estimate the total dose imparted to each patient. Corresponding parameters were subsequently converted into the correspond-
![]()
Table 1. A summary of tissue weighting factors, WT in ICRP 26, 60, and 103.
Table source: [10] .
ing effective dose to the patient, with the aid of the Impact CT Patient Dosimetry Calculator version 1.0.4 using the ICRP 60 and ICRP 103 recommendations.
The following data were collected for each patient; machine type, patient’s age, tube current (mA), collimation, rotation or exposure time, X-ray tube kilo voltage (kVp), CTDIvol, and DLP. However, since most of the patients had more than one series of the scan, parameters were collected for each series and in some cases the average of the parameters were used for calculations.
A paired t-test was calculated at 95% confidence limit to determine if there was any significant difference between the ICRP 60 and 103 publications.
3. T-Test Evaluation of the Effective Dose
The t-test is a statistical test which determines whether two sample means (averages or proportions) are equal. Here, the t-test is used to determine whether the means of the effective doses obtained with the ICRP 60 and the ICRP 103 are in any way equal, and also to determine any significant difference at 95% confidence limit.
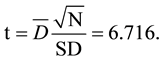
The t-test is mathematically expressed as:
 (2)
(2)
where t is the t-test value calculated, D = average individual deviation of each pair,  = total number of values in each set and SD = standard deviation of the deviations.
= total number of values in each set and SD = standard deviation of the deviations.
From Table 2, the total deviations from each pair:
∑D = 33.7 mSv.
And the mean of the total deviations is:

The standard deviation (S.D) calculated from the table is
![]()
Table 2. Showing the obtained ICRP 60, ICRP 103 effective doses.
And since the total number of the deviations,
N = 20.
Therefore, the T-test, t is calculated as:
4. Discussion
The effective dose is the sum of all equivalent doses in all the tissues and organs of the body. The effective dose, E, is a radiation dose parameter and it takes into account the absorbed dose received by each irradiated organ and the organ’s relative radiosensitivity. CT doses are relatively high and have not decreased over time as they have in conventional radiography.
It is observed from Table 2 that the values obtained with the use of the ICRP 60 recommendations are higher than those obtained from the use of the ICRP 103 recommendations for every instance. The ICRP 60 report was published in 1991 as an update to ICRP 26 which was published in 1977. With various revisions to ICRP 26, including enhancements to the radiation weighting factor and tissue weighting factor methods.
The ICRP 103 report published in 2007 establishes no change to the operational quantities and dose limits. However, it attributes changes to the effective dose as a result of changes to the radiation weighting factor, WR and the tissue weighting factor, WT regardless of the radiation type. In the ICRP 103 report, most tissues have reductions in the tissue weighting factor as compared to the ICRP 60 report and this in turn contributes to the reduction in the effective dose obtained.
Table 2 shows that the minimum effective dose obtained with the ICRP 60 is 8.5 mSv while the corresponding minimum with ICRP 103 is 7.8 mSv. Similarly, the maximum effective dose obtained with the ICRP 60 is 49 mSv while the corresponding maximum with the ICRP 103 is 44 mSv. Consequently, the minimum and maximum deviations from both ICRP 60 and ICRP 103 recommendations for the abdominopelvic CT scans results under consideration are 0.7 mSv and 5.0 mSv respectively.
From Table 2, the mean obtained from the ICRP 60 recommendations is 18.75 mSv while the mean obtained from the ICRP 103 recommendations is 17.065mSv. The difference in the means obtained suggests a marked variation in them. Therefore, a T-Test was applied for verification of the statistical difference. At 95% confidence limit and 18 degrees of freedom (i.e. V = N − 2), the value in the t-table is 2.10 and since the t-calculated (6.716) is greater than t-tabulated (2.10), it can be concluded that there is a statistical significant difference in the ICRP 60 and ICRP 103 recommendations in the determination of the effective dose. This confirms that there is an appreciable difference between both recommendations and it implies the ICRP 103 is more suitable for use because it gives a statistical reduction in radiation dose to the patient.
5. Conclusion
Attention should be paid to quality control and application of diagnostic reference levels. More than a 50 percent reduction in patient dose is possible by appropriate choice of scanning parameters―these together with other factors such as patient size, patient age could also affect the radiation dose. When the volume/size to be imaged is not irradiated simultaneously, there could be irregularity in the radiation dose to the patient. Similarly, reduction in the tube current-time product in relation to the size of the patient will equally reduce radiation dose to the patients.
NOTES
*Corresponding author.