Relationship between peripheral arterial disease, carotid intima-media thickness and C-reactive protein in elderly diabetic patients ()
1. INTRODUCTION
Diabetes mellitus (DM) is a prevalent disease especially among elderly. Egypt was ranked the 10th worldwide for the number of people with DM in 2003 (3.9 million) and this number is expected to reach 7.8 million in 2025 [1].
Persons with DM are at an increased risk for atherosclerosis which is responsible for cardiovascular diseases (CVD) (coronary heart disease, peripheral arterial disease, or cerebrovascular disease) [2]. Atherosclerosis starts by preclinical increase in the thickness of the internal and medial membrane of the arterial wall (intima-media thickness—IMT) [3] together with inflammation of the wall of the artery [4]. Several studies addressed the correlation of C-reactive protein (CRP) as a marker of inflammation to the preclinical increase in IMT [5] and now CRP level has emerged as an interesting novel and clinically useful marker for increased cardiovascular risk [6].
Peripheral arterial disease (PAD) is considered an independent risk factor for vascular diseases in other arteries and its prevalence increases with age, resulting in increased rate of cardiovascular events and mortality. On top of that, it adversely affects the functional status of the elderly [7]. In epidemiological reports, PAD prevalence among diabetic patients varies widely among countries, ranging from 6.3% to 36.1% but generally; PAD is more frequent among diabetic patients than non-diabetic ones [8,9].
The most objective practical mean of documenting the presence and severity of PAD is the measurement of ankle brachial index (ABI) [10]. It is non-invasive, simple, and at the same time it can be correlated with coronary artery disease [11].
Identifying markers of early PAD—in such a large population at risk (diabetic patients)—can facilitate appropriate and early intervention. For this reason, the aim of this work was to study the association between carotid IMT (CIMT) and high sensitivity CRP (hs-CRP) level as markers for PAD in elderly patients with DM.
2. PATIENTS AND METHODS
2.1. Study Design and Setting
A case-control study was conducted on 90 participants aged 60 years and older attending outpatient clinic of Specialized Medical Hospital of Mansoura University, Mansoura, Egypt.
Sixty cases were recruited and subdivided into group (1) that included 30 participants suffering from DM with other co morbidities and group (2) including 30 participants suffering from DM alone. Another 30 healthy elderly represented the controls and referred to as group (3).
For purpose of the study, exclusion criteria included any causes of altered CRP level (e.g. current infection, rheumatological disease…etc.).
2.2. Data Collection
All participants were subjected to comprehensive geriatric assessment that includes detailed personal and medical history and physical examination. Detailed medical history included common comorbidities in elderly with special focus on PAD, hypertension, cardiovascular diseases as coronary heart disease, and cerebrovascular disease.
2.3. Laboratory Investigations
Markers for cardiovascular disease such as high-sensitivity CRP (hs-CRP), total cholesterol (TC), triglycerides (TG), high density lipoprotein (HDL), and low density lipoprotein (LDL) levels were measured.
2.4. Radiological Assessments
2.4.1. Carotid Duplex
Bilateral B mode-Doppler with color imaging carotid artery duplex was done to evaluate the carotid arteries. Measurement of CIMT was made at a point on the far wall of the common carotid artery, 2 cm proximal to the bifurcation, from a longitudinal scan plane that showed the intima-media boundaries most clearly. On the screen displaying the frozen magnified image of the far wall of the common carotid artery, two cursors were positioned on the boundaries of the intima-media. The distance between these cursors was recorded to the nearest 0.1 mm (maximum axial resolution of the scanner) as the IMT. The procedure was repeated for each side of the neck. CIMT is a simple non-invasive way and with high predictive value for cardiovascular complications [12].
2.4.2. Hand-Held Doppler Ultrasound
Bilateral measuring of ABI was done. The ABI is the ratio of the highest systolic blood pressure (SBP) in the dorsalis pedis or posterior tibial arteries of each leg to that of the highest SBP in the brachial artery of each arm [13]. During the inflation of a pneumatic cuff, the onset of flow was detected with a hand-held continuous wave Doppler ultrasound device probe placed over the dorsalis pedis and posterior tibial arteries and thus denoting ankle SBP while brachial artery SBP was assessed by the routine method using stethoscope. Decrease in the ABI is consistent with PAD. Mild-to moderate PAD usually produces ABI in the range of 0.41 to 0.90. A reading below 0.40 suggests the presence of severe PAD [14].
2.5. Statistical Analysis
Data collected was revised, coded, tabulated, and introduced into a personal computer. Statistical analysis was performed using the 16th version of Statistical Package of Social Science (SPSS). Quantitative variables were presented in the form of means and standard deviation. Qualitative variables were presented in form of frequency tables (number and percent). Comparison between quantitative variables was done using t-test to compare two groups and ANOVA to compare more than two groups. Control for overall type I error was performed using the Bonferroni post hoc comparison test. Comparison between qualitative variables was done using Pearson’s Chi square test or Fisher’s exact. Correlation between two quantitative variables was done using Pearson’s correlation co-efficient. Odds Ratio (OR) was also calculated for PAD symptoms between cases and controls. Logistic regression analysis was done to identify the predictor of PAD. P value is considered significant if equal to or less than 0.05.
3. RESULTS
Ninety patients aged 60 years and more were recruited. Mean age among group (1) was 67.30 ± 6.82 yr, group (2) was 65.83 ± 5.96 yr and among group (3) was 67.10 ± 9.40 years. Males represented 37.8% (n = 34) while females represented 62.2% (n = 56) of the study sample (Table 1). As for comorbidities in group (1), 40% (n = 12) had ischemic heart disease and 16.6% (n = 5) had cerebrovascular disease and all of them had hypertension.
Systolic and diastolic blood pressures, weight and hsCRP levels showed statistically significant difference between group (1), (2) and (3) (P value ≤ 0.001, < 0.001, 0.030, < 0.001 respectively) being all highest among group (1) and lowest among group (3) (Table 1). Post hoc Bonferroni test revealed that the significant differences in systolic and diastolic blood pressures and weight were only between those of group (1) and group (3), while the significant differences in hs-CRP levels were between groups (1) and (3) (P value < 0.001), (2) and (3) (P value < 0.001), and (1) and (2) (P value < 0.021). Hs-CRP levels were highest in group (1) (1266.67 ± 392.96 mg/dl) followed by group (2) (991.6 ± 448.12 mg/dl) then group (3) (420.43 ± 303.11 mg/dl) (Table 1).
There is no statistical significant difference regarding other cardiovascular risk factors (male sex, smoking, age,
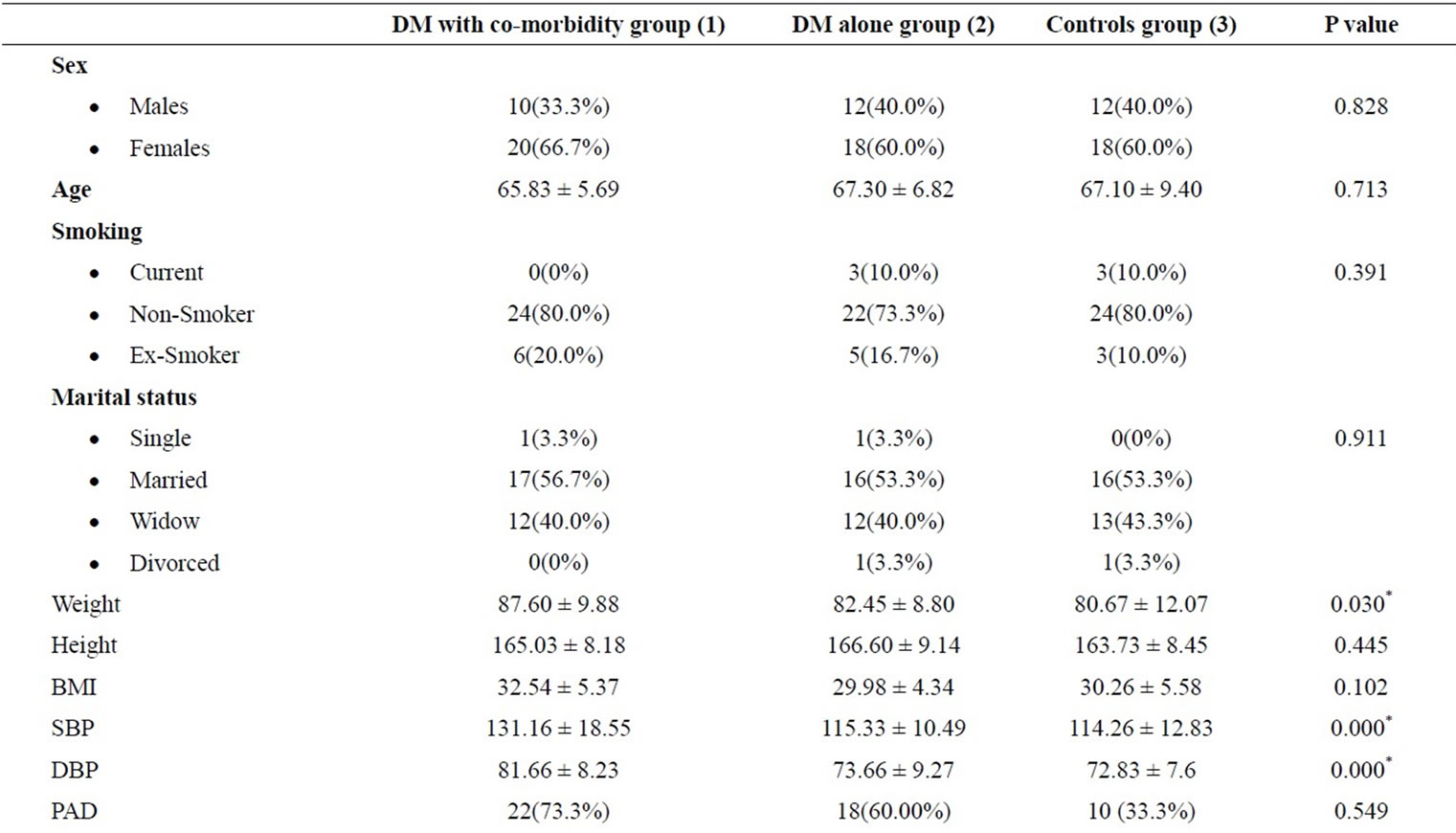
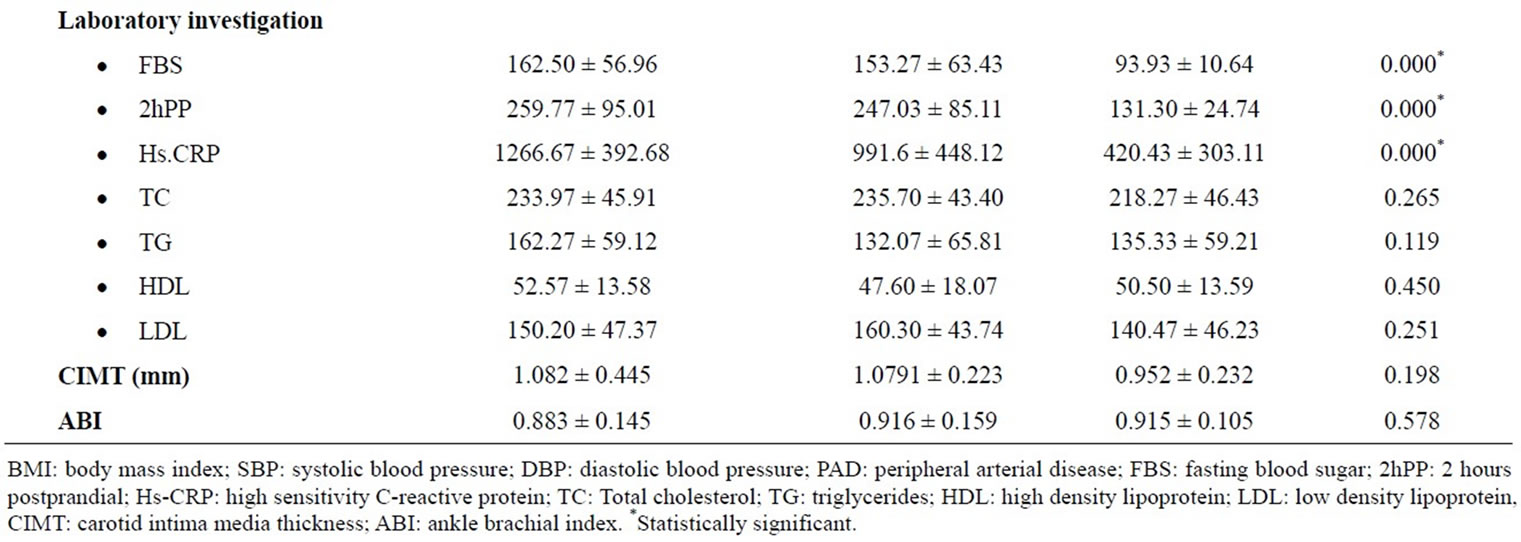
Table 1. Comparison between the three studied groups as regard qualitative and quantitative variables.
BMI, TC, TG, HDL-C, LDL-C, CIMT, and ABI) between group (1), (2) and (3) (P value = 0.828, 0.391, 0.713, 0.102, 0.265, 0.119, 0.450, 0.251, 0.198, 0.578 respectively) (Table 1).
Although not reaching statistical significance, percentage of PAD was higher in group (1) (73.3%, n = 22) and group (2) (60.00%, n = 18) than group (3) (33.3%, n = 10).
As regard the correlation between diabetes control and complications, group (1) had statistically significant higher use of insulin (100% vs 73.3%), symptoms of poor control (96.7% vs 70%), cataract (40% vs 13.3%), diabetic neuropathy (93.3% vs 53.3), diabetic retinopathy (43.3% vs 6.7%), diabetic nephropathy (20% vs 0%) and longer duration in month (170.40 ± 80.98 vs 85.87 ± 72.14) than group (2) (P value = 0.002, 0.006, 0.020, < 0.001, < 0.001, 0.010, < 0.001 respectively) (Table 2).
Generally, symptoms of PAD as color changes, delayed wound healing, claudication pain, resting pain, trophic changes, cold extremities were statistically significantly higher among cases than controls (P value ≤ 0.001, 0.025, 0.035, 0.034, 0.011, 0.001). Their Odds Ratios were higher for cases than controls. For color changes, delayed wound healing, claudication pain, resting pain, trophic changes, cold extremities, OR were 10.286, 5.091, 7.250, 7.250, 9.667, and 6.111 respectively (Table 3).
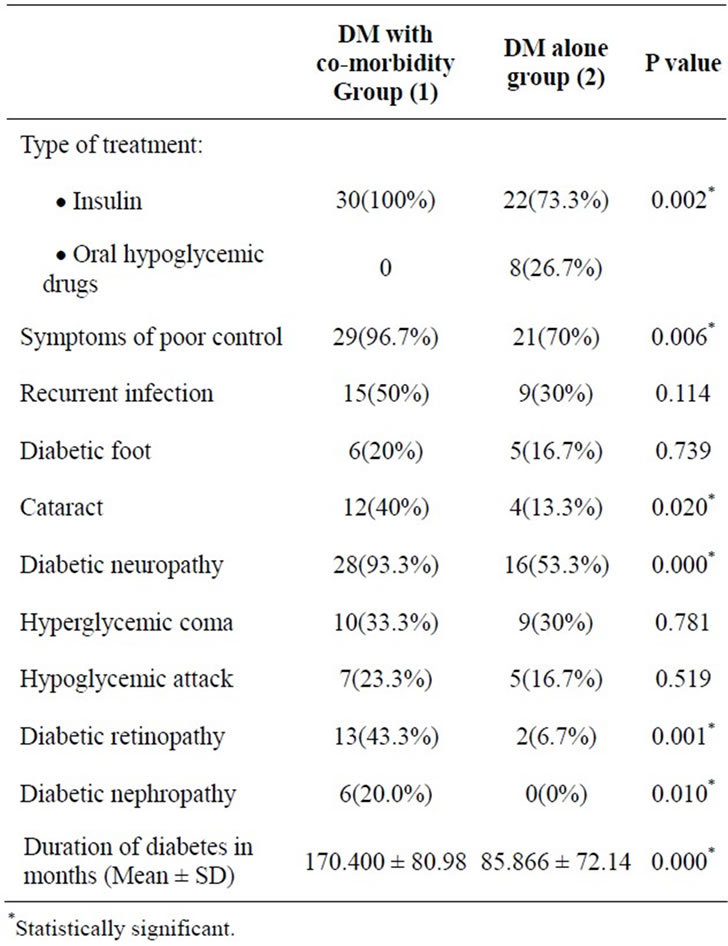
Table 2. Comparison between group (1) and group (2) as regard Diabetes Control and Complications.

Table 3. Comparison between cases (groups (1) & (2)) and controls (group (3)) regarding symptoms of peripheral arterial disease.
ABI was able to detect PAD in many asymptomatic patients. Color changes were present in only 50.20% (n = 26) of positive PAD cases and delayed wound healing, claudication pain, rest pain, cold extremities, and trophic changes were present in 28.00% (n = 14), 20.00% (n = 10), 20.00% (n = 10), 54.00% (n = 27), and 26.00% (n = 13) (Table 4).
Using logistic regression analysis revealed that DM, CIMT, and hs-CRP were independent predictors for PAD (OR = 4.194, 7.236, 1.003; P value = 0.044, 0.25, 0.031) after adjustment of other coronary risk factors such as sex, smoking, hypertension, TC, and TG (Table 5).
4. DISCUSSION
DM and its complications represent a major burden to public health. Early diagnosis and management of PVD in the elderly especially in diabetics is very crucial because it is an independent risk factor for vascular diseases in other regions, resulting in increased rate of cardiovascular events and mortality in addition to its impact on physical function [7,15,16].
So a case-control study was performed on 90 elderly to identify the predictors of PAD in elderly diabetic patients. Sixty cases were divided into group (1) that included 30 participants suffering from DM with co-morbidities and group (2) including 30 participants suffering from DM alone. Another 30 healthy elderly represented the controls group (3).
In this study, despite finding no significant difference in the prevalence of PAD between DM cases and controls groups, the symptoms of PAD were statistically significantly more in DM cases than controls.
This study like many other studies found that most elderly men and women with PAD did not suffer symptoms [7,17] as more than half of the PAD cases diagnosed by ABI which were asymptomatic by history and physical examination. In fact a recent database population based study found that age was the strongest risk
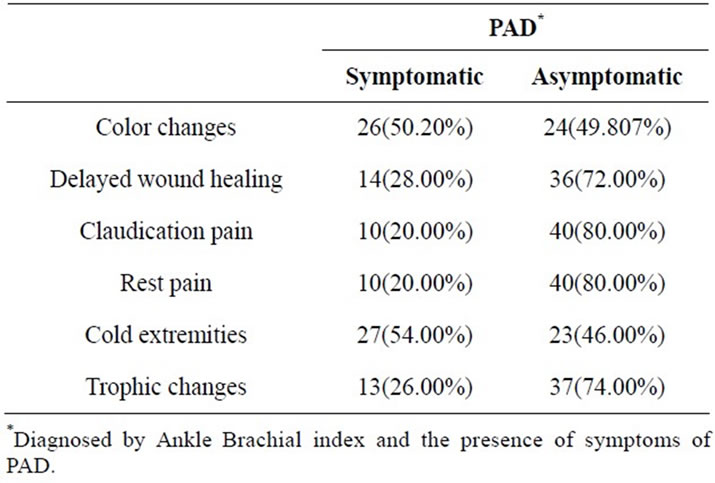
Table 4. Relationship between symptomatic and asymptomatic cases of peripheral arterial disease (PAD).
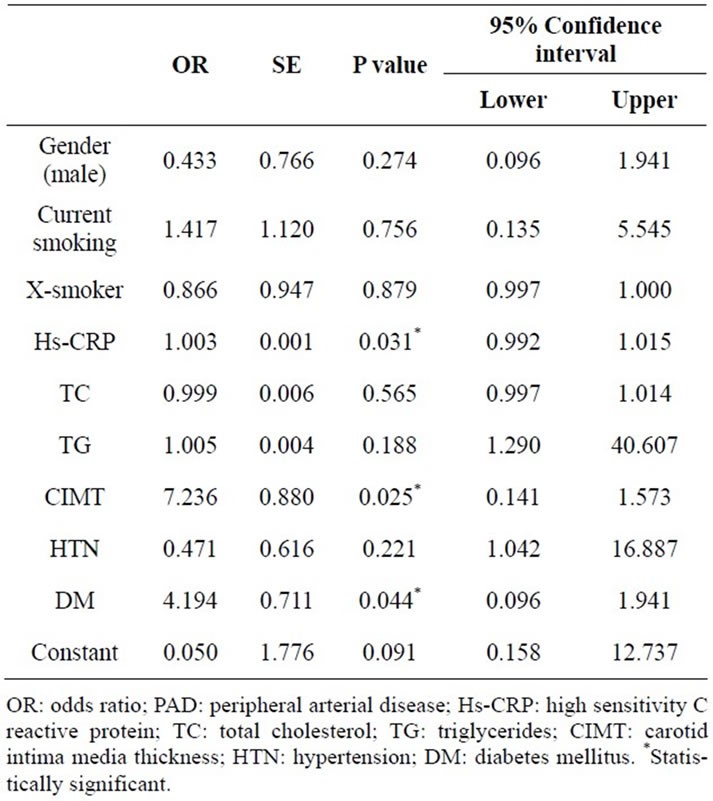
Table 5. Logistic regression analysis for predictors of peripheral arterial disease.
factor for the development of asymptomatic PAD [18]. So, poorer outcomes are expected in asymptomatic elderly patients with concomitant PAD and DM due to delayed diagnosis.
We found that DM, CIMT, and hs-CRP levels were independent predictors for PAD after adjustment for other coronary risk factors as sex, smoking, hypertension, TC, and TG. So, PAD should be suspected in any elderly patient when one or more of these risk factors is present putting in mind that CIMT had the highest odds ratio (7.136) followed by DM (odds ratio = 4.194) and lastly hs-CRP (odds ratio = 1.003).
With age, there were increased IMT and inflammation in the arterial wall due to exposure to advanced glycation end products, which, in turn, stimulate systemic inflammation, oxidative stress, fibrosis, and lipid deposition in the arterial wall especially in DM. An increased CIMT is considered as a sign of early atherosclerosis and as a window for coronary and lower limb arteries [19,20].
DM patients are more likely to present late due to impaired pain perception resulting from associated peripheral neuropathy in those patients. In fact, the presence of concomitant DM in patients with PAD was associated with a 15-fold increased risk of lower extremity amputation [21,22].
It is also reported that CRP is present in the core of atheromatus plaques in subjects who experienced sudden death [23]. High CRP causes direct reduction in the nitric oxide production and induces monocyte chemotaxis, cytokine release, and tissue factor secretion (110) which eventually predicts adverse vascular events as coronary heart disease and PAD [24-27].
So, we concluded that DM in elderly is associated with higher prevalence of asymptomatic PAD using solely ABI. DM, CIMT, and hs-CRP are independent predictors for the occurrence of PAD. Hs-CRP levels are highest among diabetic group with comorbidities.