Open Journal of Radiology
Vol.05 No.04(2015), Article ID:62196,8 pages
10.4236/ojrad.2015.54032
Partial Quality Assessment of 60Co-Teletherapy Machine Performance
Mohammed A. Ali Omer1,2
1College of Medical Radiologic Science, Sudan University of Science and Technology, Khartoum, Sudan
2Department of Radiologic Technology, College of Applied Medical Science, Qassim University, Buraidah, Saudi Arabia

Copyright © 2015 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 23 November 2015; accepted 22 December 2015; published 25 December 2015
ABSTRACT
The aim of this study was to assess the performance of 60Co-teletherapy unit at Radiation and Isotopes Center in Khartoum, using the common tools used for quality control (Front pointer, Graphic paper, Pin, Non-screen film, meter and Check plate). The collected and analyzed data revealed that: there was a difference between the calculated theoretical field size (FS) and the measured one relative to the change of SSD; and the average FS shift was 0.9 cm relative to the standard one, while the machine isocenter was almost fixed at 0˚ with a shift of 0.003 cm, which was within the standard limit (0.2 cm). The diaphragm isocenter showed a shift of ±0.36 cm (i.e. in clock and anti clock wise) in average relative to standard limit (±0.3 cm) and the couch vertical isocenter (CVI) relative to the SSD changes was exceeded the standard limit (0.2 cm) by a factor of 0.9 cm. Also the SSD determined by the optical distance indicator was greater than the actual SSD (determined by Front pointer and measured by scale meter) by an average of 0.8 cm; which exceeded the limit (0.3 cm) by an average factor of 0.5 cm. The study also showed that the penumbra profile (1.5 cm) was less than the actual specified for 60Co-teletherapy machine, while the radiation beam was so homogeneous across the field size.
Keywords:
60Co-Quality, Control, Teletherapy, Radiotherapy, Assurance

1. Introduction
The procedure of radiation therapy is so highly sensitive case of controlling the dose delivered to tumor target volume i.e. ±5% as permissible shift from the prescribed tumor dose and minimizing or protecting the critical organs [1] -[3] . However, such fine controlling of tumor irradiation is subjected to many factors that degrade the accuracy of radiotherapy, such as system aging, mechanical\electrical over load shift, electronic dysfunction, modifications of components and spare parts due to unexpected breakage and other technical and clinical errors. In relation to such realm ICRP, [4] classifies the causes of radiotherapy errors in the following sources: 1) deficiencies in education and training; 2) deficiencies in procedures and protocols; 3) equipment faults; 4) deficient communication and transfer of essential information; 5) lack of independent checks; 6) inattention and unawareness; and 7) unsecured long-term storage and abandonment of radiotherapy sources. And accordingly the quality assurance tests have been divided to the followings: a) acceptance test; b) commissioning test and; c) periodic routine test.
Therefore, the quality assurance in radiotherapy (All procedures that ensure consistency of the medical prescription, and safe fulfillment of that prescription, as regards the dose to the target volume, together with minimal dose to normal tissue, minimal exposure of personnel and adequate patient monitoring aimed at determining the end result of the treatment) [5] as a procedure has to be continued as necessary and inevitable. And based on the standards recommended by WHO in 1988, American Association of Medical Physics (AAPM) in 1994, European Society for Therapeutic Radiation Oncology (ESTRO) in 1995, Clinical Oncology Information Network (COINW) in1999, IEC in 1984 and Institute of Physics and Engineering in Medicine (IPEM) in 1999, an efforts had been devoted to assess the 60Co-teletherapy unit and the error shift relative to the standards and the equipment error source at radiation and isotopes centre of Khartoum RICK. The classified error source related to equipment mentioned above, implies the followings:
§ Stability of gantry & collimator axis’s;
§ Coincidence of gantry, collimator and table axis at the isocenter;
§ Verification of jaw symmetry;
§ Verification of radiation light fields congruence;
§ Accuracy readouts for field size, gantry & collimator angle;
§ Location of x-hair & verify that all the isocenter locators (front pointer, optical distance indicator ODI & lasers beams) identify the same point in space;
§ Identify of ODI, laser beams and x-hair coincide with isocenter;
§ Assurance automatic setting of the jaw with applicator size (for electrons).
However, the trend of this study scarcely is considered by authors, and it will focus on the equipment faults (Theoretical field size (FS) which is calculated using Myneord Factor and the measured one relative to the change of source surface distance SSD, agreement of practical measured field size with theoretical inverse square low stated by using Myneord Factor, agreement of collimator, couch and gantry angel isocenter versus SSD variability, agreement between scale meter SSD and the actual measured SSD determined by front pointer, extension of penumbra profile and the laser beams coincidence at the isocenter), and the relevant mechanical limits as stated by IAEA and ISRO [6] are as follows:
・ Isocenter indication, collimator rotation, room lasers and optical distance indicator (2 mm);
・ Angular scales of gantry and collimator (0.5˚);
・ Field size indication and coincidence between light and radiation field (2 and 3 mm);
・ Stability of gantry and collimator using lateral opposed beams (3 mm);
・ Table movements to test the vertical and lateral treatment couch displacements (2 mm).
And due to variation among institution for the clinical purposes and purchased equipments, there are certain generic considerations of assessment. These considerations include: 1) clinical needs assessment; 2) definition of specifications, selection and purchase process; 3) installation; 4) acceptance testing; 5) commissioning; 6) training; 7) clinical use and; 8) periodic quality control (QC) [7] -[9] , which are mostly under medical physicists responsibilities. In relation to this study, the European Organization for Research and Treatment of Cancer (EORTC) have carried out quality control for16 centers (Table 1) representing a total of 23 accelerators, 14 cobalt units and 14 simulators for a grand total of 1299 irradiation parameters, their results revealed that as major deviations, 3 cobalt units showed an 8 mm maladjustment of a laser and a 10 and 20 mm maladjustment of the optical distance indicator, for each unit type there was one occurrence of maladjustment of the field size indicator (9 mm, 9 mm and 10 mm, respectively). The score of 60Co units were inferior to those of accelerators and simulators, especially for isocenter indication with 43% of major deviations and only 36% of acceptable deviations, which was ascribed to the advanced age (up to 20 years) of some of these units [6] [10] .
The selection of 60Co-teletherapy machine for the current study; based on the technologist’s complaining at the radiation center, which is as well represents the common utilized machine among developing countries for
Table 1. Shows the distribution % of mechanical and beam alignment checks, where the acceptable limit as (A ≤ ε), minor (m = ε < ε ≤ 2ε) or major (M ≥ 2ε) [6] .
the cheapest price, easy maintenance and friendly usage.
2. Materials and Methods
2.1. Materials
・ 60Co-teletherapy unit: namely as Equinox teletherapy unit manufactured by MDS Nordion. This newly designed unit features asymmetric jaw capability and has a source to Axis Distance (SAD) of 100 cm and with a 2.0 cm diameter C-146 radioactive source.
・ Graphic paper (Figure 1 with field size 10 × 10 cm and center).
・ Mechanical front pointer.
Non screen film.
2.2. Methods
2.2.1. Congruence of Theoretical (Calculated FS) and Measured Field Size Relative to Variable SSDs
Determined the field size 10 × 10 cm in the graphic paper, so the graphic paper placed on the couch at SSD 80 cm with cross hair in the center of the field size of the paper; then opened field size 14 × 14, 12 × 12, 10 × 10, 8 × 8, 6 × 6, 4 × 4, 2 × 2 with different SSD 85, 95, 100, 105, 110, 115, 120 cm which is determined the light field in the graphic paper. These field sizes have to be compared with the calculated field sizes using inverse square law based on Mynerad factor.
2.2.2. Congruence of Gantry Rotation Isocenter (GRI) and Machine Isocenter
The stability test of GRI applied to confirm that: the machine is rotating around fixed pivot or center. It carried out by setting the Gantry angle at zero degree i.e. vertical position, and the projection of the cross hair shadow falls on a pin situated along the cross hair direction and all shadows shined and received on a graphic paper, which should be in concise and congruence at different gantry angles i.e. from 0˚ to 300˚, and the variation or the shift between the shadow of cross hair and the pin was measured on the graphic paper.
2.2.3. Diaphragm Isocenter (DI)
The DI test carried out to confirm that the diaphragm is rotated around fixed isocenter (pivot). To do so, the gantry angel set at zero degree (0˚) with opened field size as 10 × 10 cm at SAD = 100 cm, then a graphic paper placed on the top of treatment couch with a field size 10 × 10 cm drawn on it. Then the two fields were adjusted in congruence state ad well as the cross hair. Then the diaphragm rotated to different angles 0˚ - 360˚ and the shift of diaphragm isocenter (cross hair) has been registered from the graphic paper.
2.2.4. Cough Vertical Isocenter (CVI)
The CVI test carried out to assure that the couch being drive up or down wards a long true vertical constant track. Depending on the accuracy of GI, a field size of 10 × 10 cm was set and projected concisely with similar field size drawn on graphic paper situated at SAD = 100 cm on couch top, then the couch of treatment raised upwards to different SSD as (positive Numbers) and downwards to different SSD as (negative Numbers). And the shift of cross hair relative to drawn cross center at the graphic paper field has been recorded.
2.2.5. Source Surface Distance (SSD) Test
SSD test carried out to confirm that: the machine is rotating constantly based on constant radius which is 100 cm. it carried out by measuring the SSD using optical distance indicator 100 cm (Scale meter) as a part of machine assembled configuration and compared with SSD measured by standard meter, then a comparison between two measurers has been carried out.
2.2.6. Dose Homogeneity and Penumbra Assessment
The aim of this test is to assure the homogeneity of dose across the field and the penumbra profile. This test carried out by using non screen film (enveloped film), up on which the field size of 10 × 10 cm has been marked by drawing the corners of the film by pencil as well as the center of the field as shown in Figure 2, then the film has been put on the couch top with the machine field size 10 × 10 cm projected in concise manner with that field drawn on the enveloped film and a buildup material (polystyrene) with 0.5 cm thickness embedded on the top of the enveloped film for electronic equilibrium since the radiation was γ-radiation. Then the film with a buildup assembly has been exposed to radiation for 1 second. Then the film has been processed and scanned by the optical densitometer from edge to edge across the center. The optical density has been plotted versus the radiation field width as shown in Figure 5.
3. Results
The following chapter will highlight the results related to measurements carried out to assess the performance of the 60Co-teletherapy machine at RICK. The specific parameters were the comparative between the mathematical theory (calculated FS) and measured field size relative to variable SSDs, correlation between the Gantry angles and the machine isocenter, correlation between the couch vertical isocenter and the different SSD in cm, correlation between the collimator isocenter shifts in cm versus diaphragm angle of rotation, correlation between the optical density percent across the mid scanning of the irradiated field and correlation between the actual SSD (measured) and the SSD noted by distance indicator.
Figure 1. Shows the graph paper used to assess the variation shift of machine and laser beam isocenters.
Figure 2. Shows the enveloped film with a field size 10 × 10 cm drawn on and the light field projected on.
4. Discussion
Figure 3 shows the comparative between the mathematical theory (calculated FS) and measured field size relative to variable SSDs. It reveals that there is a difference between the theoretical FS i.e. calculated one based on Myneord Factor stated by Khan, [11] and the measured one relative to the change of SSD; and the average difference was 1.1 cm indicating that the average shift from the permissible standard was 0.9 cm. These linear curves suppose to be superimposing to confess the identicalness and agreement between the theory and practical, which is missed here. Such missing of superimposing between the two curves could be ascribed to the loss of standard gradient in couch driving upwards or down wards or misadjusting in the collimator blades. Such shift in the field size (0.9 cm) from the standard theoretical one is exceeding the permissible limit based on the limit stated by Zeman and Dooley, [12] and IAEA and ISRO, [6] , hence it needs urgent correction.
Figure 4 shows the correlation between the Gantry Rotation Isocenter and machine isocenter in degree. Such relation is fitted to equation of the form: y = 0; i.e. the isocenter “y” will remains “0” as long as the gantry angle changes, however the result reveals that the machine isocenter is almost fixed at 0 with a shift of 0.003 cm. The result is in agreement with the reference value of acceptance test dated back to the date of installation. And such parameter is usually unchangeable i.e. permanently fixed based on American Association of Physicist in Medicine AAPM report No. 13 [13] , therefore all other parameters such as couch isocenter, laser beams, scale meter… etc would be recon on.
Figure 3. Shows the comparative between the mathematical theory (calculated FS) and measured field size relative to variable SSDs in cm.
Figure 4. Shows the correlation between the Gantry angles and the machine isocenter in degree.
Figure 5 shows the correlation between the collimator isocenter shifts in cm versus diaphragm angles of rotation in clock wise (positive degrees) and anti clock wise (negative degrees). It shows that by rotating the diaphragm in clock wise and anti clock wise there is some shifts in the diaphragm isocenter as ±0.65 cm in average i.e. it will results in a deviation of the radiation beam relative to the planned target volume. Such shift in diaphragm isocenter could be ascribed to erosion of certain bearing by one side; and according to the permissible limit stated by AAMP and mentioned by Goran et al., [14] and IAEA and ISRO, [6] , the shift has exceeds the limit by a factor of 0.35 cm; hence such fault has to be corrected accordingly. Figure 6 shows the correlation between the couch vertical isocenter (CVI) and the different SSD in cm. it shows that the motion or raising the couch upwards relative to SSD variability resulted in a couch isocenter shift from the correct point i.e. at 0.0 cm which correspond to SSD = 100 cm to ±1.3 cm in upward and downward direction. And the motion of the couch could be represented by and equation of polynomial of the form: y = 0.006x2 − 1.295x + 63.55, where y refers to couch isocenter shift in cm and x refers to SSD in cm; the x2 has two values indicating the two direction of the couch i.e. positive for upwards direction and negative for downwards direction. Such average shift (±1.1 cm) is exceeding the limit stated by IAEA and ISRO, [6] and Goran et al., [14] by a factor of 0.9 cm. hence there will be necessity for QC procedure to reassure the proper motion of the table.
Figure 5. Shows the correlation between the diaphragm isocenter shifts in cm versus angles of diaphragm rotation in clock wise and anti clock wise.
Figure 6. Shows the correlation between the couch vertical isocenter and the different SSD in cm.
Figure 7 shows the correlation between the actual SSD (measured) and the SSD noted by optical distance indicator. It shows that the SSD determined by the optical distance indicator increases from the actual SSD (determined by Front pointer and measured by scale meter) by an average of 0.8 cm and the correlation could be given by the following empirical and significant (R2 = 0.9) equation: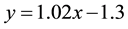 , where “y” refers to optical distance indicator SSD which is a part of machine assemble and “x” refers to actual SSD in cm. The increment in optical distance indicator SSD is exceeding the limit by a factor of 0.5 cm based on the limit stated by Adams and Warrington, [15] .
, where “y” refers to optical distance indicator SSD which is a part of machine assemble and “x” refers to actual SSD in cm. The increment in optical distance indicator SSD is exceeding the limit by a factor of 0.5 cm based on the limit stated by Adams and Warrington, [15] .
Figure 8 shows the correlation between the optical density percent across the mid scanning of the irradiated field. Such study shows that the optical density of the irradiated field started at a point outside the actual field size (10 × 10 cm) by 2 cm where it was 0% and increases towards the point of actual field size at which it was 100% in average. And based on Full Width at Half Maximum (FWHM) which is equal to 5.7 cm, the profile of penumbra would be equal to 1.5 cm [14] which was less than the actual penumbra profile (2 cm) obtained by calculation for 60Co radioactive source which was 2 cm, SAD 100 cm and the source collimator distance was 60 cm [11] [15] . This fact ascertaining the result in Figure 7 that as SSD increases the penumbra profile decreases. Also the optical densities scanning across the field profile reveal the homogeneity of the radiation dose across the field.
Figure 7. Shows the correlation between the actual SSD (measured) and the SSD noted by optical distance indicator.
Figure 8. Shows the correlation between the optical density percent across the mid scanning of the irradiated field.
5. Conclusion
The 60Co-teletherapy unit as common susceptible to faults due to overload and prolonged period of usage, the mechanical motion of the unit could be easily plotted and tracked in a curves for easy and friendly assessment that would suit the frequently faults.
Cite this paper
Mohammed A. AliOmer,11, (2015) Partial Quality Assessment of 60Co-Teletherapy Machine Performance. Open Journal of Radiology,05,235-242. doi: 10.4236/ojrad.2015.54032
References
- 1. Zhu, X.R. (2000) Entrance Dose Measurements for in-Vivo Diode Dosimetry: Comparison of Correction Factors for Two Types of Commercial Silicon Diode Detectors. Journal of Applied Clinical Medical Physics, 1, 100-107.
http://dx.doi.org/10.1120/1.308253 - 2. ICRU (1976) Determination of Absorbed Dose in a Patient Irradiated by Beams of x or Gamma Rays in Radiotherapy Procedures. ICRU Report 24, Bethesda, Maryland and Washington DC.
- 3. Huang, K., Bice Jr., W.S. and Hidalgo-Salvatierra, O. (2003) Characterization of an in Vivo Diode Dosimetry System for Clinical Use. Journal of Applied Clinical Medical Physics, 4, 132-142.
http://dx.doi.org/10.1120/1.1559920 - 4. International Commission on Radiological Protection (ICRP) (2000) Prevention of Accidental Exposure to Patients Undergoing Radiation Therapy. International Commission on Radiological Protection, Oxford.
- 5. Podgorsak, E.B. (2005) Radiation Oncology Physics: A Handbook for Teachers and Students. IAEA, Vienna.
- 6. IAEA and International Society for Radiation Oncology ISRO (1995) Quality Assurance in Radiation Therapy. Proceedings of the Working Meeting on National Programmes: Design, Harmonisation and Structures, Vienna, 8-9 May 1995, 62.
- 7. Van, D.J. (2009) Commissioning and Implementing a Quality Assurance Programme for New Technologies. International Conference on Advances in Radiation Oncology (ICARO), Vienna, 27-29 April 2009, 21.
- 8. Nath, R., Anderson, L.L., Luxton, G., et al. (1995) Dosimetry of Interstitial Brachytherapy Sources: Recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. Medical Physics, 22, 209-234.
http://dx.doi.org/10.1118/1.597458 - 9. Rivard, M.J., Coursey, B.M., Dewerd, L.A., et al. (2004) Update of AAPM Task Group No. 43 Report: A Revised AAPM Protocol for Brachytherapy Dose Calculations (AAPM Report No. 84). Medical Physics, 25, 633-674.
http://dx.doi.org/10.1118/1.1646040 - 10. Dam, V.J., Johansson, K.-A., Bridier, A. and Sernbo, G. (1993) EORTC Radiotherapy Group Quality Assurance: Mechanical Checks and Beam Alignment of Megavoltage Equipment. Radiotherapy and Oncology, 29, 91.
http://dx.doi.org/10.1016/0167-8140(93)90231-V - 11. Zeman, G.H. and Dooley, M.A. (1984) Performance and Dosimetry of Theratron-80 Co-60 Unit. Armed Forces Radiology Research Institute—AFRRI-Technical Report—Defense Nuclear Agency, Bethesda.
- 12. AAPM (American Association of Physicists in Medicine) (1984) Radiation Therapy Committee Task Group of Quality Assurance in Radiation Therapy. American Institute of Physics, New York.
- 13. Svensson, G.K. (1994) Physical Aspects of Quality Assurance in Radiation Therapy. AAPM Report No. 13, American Institute of Physics, New York.
- 14. Adams, E.J. and Warrington, A.P. (2008) A Comparison between Cobalt and Linear Accelerator-Based Treatment Plans for Conformal and Intensity-Modulated Radiotherapy. British Journal of Radiology, 81, 304-410.
http://dx.doi.org/10.1259/bjr/77023750 - 15. Faiz, K.M. (2003) The Physics of Radiation Therapy. 3rd Edition, Lippincott Williams & Wilkins, Philadelphia.










