Open Journal of Obstetrics and Gynecology
Vol.06 No.13(2016), Article ID:72948,10 pages
10.4236/ojog.2016.613103
Predictive Factors of Complications of Vaginal Delivery on Scarred Uterus at the Yaoundé Gynaeco-Obstetric and Paediatric Hospital
E. Ngo Um Meka*, P. Foumane, F. Essiben, E. R. Ngwesse, J. Dohbit Sama, E. T. Mboudou
Department of Obstetrics and Gynecology, Faculty of Medicine and Biomedical Sciences (FMBS), University of Yaoundé I, Yaoundé, Cameroon

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: November 8, 2016; Accepted: December 20, 2016; Published: December 23, 2016
ABSTRACT
Objective: This study was aimed at identifying predictive factors of complications during vaginal delivery on scarred uterus. Methodology: During 9 months, from October 1st, 2015 to June 30th, 2016, a case control study was carried out at the Yaoundé Gynaeco-Obstetric and Pediatric Hospital. Eighty nine women each with a single scarred uterus who presented with complications during delivery (cases) were compared to eighty nine others who had a successfully trial of scar (control) during the study period. Data were analyzed using the CSPro version 6.0 and SPSS version 20.0 softwares with statistical significance set at P < 0.05. Results: We recruited 2 groups of 89 women, aged 17 to 40 years, with an average age of 29.05 years. The majority of women with complications were married (50.6%) and unemployed (42.8%). Following univariate analysis, predictive factors of complications were: prematurity (OR = 7.4), post-term (OR = 13.7), no history of vaginal delivery on scarred uterus (OR = 4.3), inter-pregnancy spacing period greater than 60 months (five years) (OR = 2.9), History of caesarian delivery indicated for cephalo-pelvic disproportion (OR = 6.6), less than four ante-natal consultations (OR = 3.6), ante- natal consultations done in a Health Centre (OR = 2.7), ante-natal follow up conducted by a nurse (OR = 2.4; IC = [1.2 - 4.7]), referral from a different health unit (OR = 4.4, IC = 2.0 - 9.4), a Bishop score less than 7 on admission (OR = 12.4, IC = 5.6 - 27.4), a meconium stained amniotic fluid (OR = 9.9; CI = [3.6 - 26.8]). After logistic regression, the retained factors associated with complications were post-term (aOR = 34.5), absence of vaginal birth after caesarian delivery, (aOR = 11.7), previous caesarean section indicated for cephalo-pelvic disproportion (aOR = 6.1), a bishop score less than 7 (aOR = 12.0), meconium stained amniotic fluid (aOR = 13.6). Conclusion: Predictive factors of complications can help anticipate negative obstetric outcomes.
Keywords:
Caesarean, Scarred Uterus, Obstetrical Complications, Predictive Factors

1. Introduction
Caesarean section is an increasing mean of delivery. Its incidence in Cameroon increased from 10.3% in 1999 to 19.7% in 2012 [1] [2] . In developed countries, this rate can approach 50%, as is the case in Brazil, according to WHO [3] .
The goal of caesarian section is to limit maternal and neonatal morbidity and mortality. However, women with scarred uterus are at higher risk in subsequent deliveries especially as concerns the risk of uterine rupture [3] [4] [5] which increases significantly maternal and fetal morbidity and mortality.
A scarred uterus is defined as a uterus with one or more myometrial scar(s) located anyway from the isthmus to the body. This excludes scars that are limited to the endometrium or serosa [4] [5] .
Numerous factors have been associated with complications of childbirth in women with scarred uterus especially with the advent of vaginal birth after caesarian (VBAC). On the other hand, numerous factors have been associated with success of VBAC. Such factors include: spontaneous onset of labor and history of per vaginal delivery.
However, other factors are implicated in failure of VBAC. These factors include: maternal age greater than 40, fetal birth weight greater than 4000 g, maternal body mass index greater than 30 kilograms per square meter, medical (prostaglandines, ocytocines) and mechanic (Foley’s catheter) induction of labor [6] .
In Cameroon, few studies have been done on the factors of morbidity during vaginal birth in women with scarred uterus.
Halle-Ekane et al., in Limbe in Cameroon between 2005 and 2012, had recovered: the indication of previous caesarean section, the type of uterine incision, stimulation of labour and foetal birth weight as factors influencing the outcome of vaginal birth on scarred uterus [7] [8] .
This motivated us to seek predictive factors of complications during childbirth on a scarred uterus.
2. Methodology
A case-control study was carried out over a period of nine months from October 2015 to June 2016 at the Yaounde Gynaeco-Obstetric and Paediatric Hospital (YGOPH). We included all women who had a history of one scarred uterus and who underwent an emergency caesarean section between 1 January 2006 and 31 December 2015, that is to say over a period of 10 years. Women with a complication before and after their surgeries were compared to women who did not have complications. Women who presented with complications in ante-, per- and post-partum (cases) were compared to those who had no complications (controls). The case had either a cesarean section, or post partum complications, while the controls with a scarred uterus, had a success vaginal delivery.
We excluded women with elective caesarean, multi-scar uterus, history of ectopic pregnancy as uterine scar, any incomplete or unusable medical record
After obtaining the ethical clearance and approval of the Director of the Hospital, we consulted the delivery registers corresponding to our study period. The medical records of women concern by the study were searched in the archives service. We then filled our technical sheet with the informations necessary. The following variables: age, profession, matrimonial status, referral, venue of ANC (antenatal care), the ANC care provider, the number of ANC, the indication of previous caesarian section, the gestational age on admission, parity, interpregnancy spacing (uterine rest period), number of per vaginal delivery, the age of the scar, abnormal placental insertion and pathologies during pregnancy were retained. Delivery room parameters included: fundal height, position of the cervix, cervical dilatation, cervical effacement, Bishop score, ante-partum hemorrhage, premature rupture of membranes, premature and prolonged rupture of membranes ≥ 12 h, color of amniotic fluid, augmentation of labour, induction of labour, abnormalities in fetal heart sounds, duration of the second phase of the first stage of labour, duration of the second stage of labour, evolution of labour using partogram, complication during delivery such as uterine rupture, hemorrhage, acute fetal distress, cephalo-pelvic disproportion. Parameters necessitating action included: trial of scar, per vaginal delivery, instrumental delivery, emergency caesarian, complications after delivery, endometritis, parietal suppuration, persistent fever and hemorrhage. Cord features included cord prolapse, cord round neck and cord round the fetal body. Other fetal features included: presentation, number of fetuses, birth weight and death of new born.
We used the Schlesselman’s formula
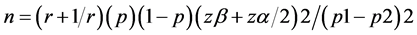
We used the data from the study made in Limbe Regional Hospital by Halle Ekane et al. [7] where about 34.5% of women had a complication during childbirth requiring emergency surgery (p1).
p2 = proportion of women with successful scar test was 65.5%.
The minimum sample size calculated was 41 cases and 41 controls. Data was analysed using the CSPro version 6.0 and SPSS version 20.0 softwares. The chi square (x2) and Fisher exact tests were used to compare variables with statistical significance set at P < 0.05. Multivariate analysis was used to eliminate confounding factors.
3. Results
A total of 178 women were recruited; 89 cases and 89 controls. Amongst the 89 cases, 84 (94%) had an emergency caesarian of which 44 (49.4%) were due to failed trial of scar while the other 40 (44.9%) were indicated on admission of the cases.
Complications seen before and during labour were; cord prolapse, cephalo-pelvic disproportion, acute fetal distress and uterine rupture while those that were seen in post-operation and post-partum were, endometritis, post-partum hemorrhage, anemia, abdominal wall infection and septicemia.
The age of women varied between 17 and 40 years, with a mean age of 29.05 years and a standard deviation of 5.17 years. The patients aged from 20 to 29 were the most represented in both groups (OR = 1.094, CI = 0.608 - 1.969; p = 0.764) (Table 1). We did not find any statistically significant association. The majority of women who had a complication were married (OR = 1.253, CI = 0.695 - 2.258; p = 0.453). We did not find a statistically significant association. Most of the women with a scar uterus who had a complication during childbirth were unemployed women (OR = 0.956, CI = 0.531 - 1.722; p = 0.881) (Table 1).
The principal indications for the emergency caesarian section in the cases with single scarred uterus were: cephalo-pelvic disproportion (CPD) (33.7%) and acute fœtal distress (13.5%) (Table 2). Post-partum and post-operative complications were dominated by post partum haemorrhage (36.8%).
Clinical and obstetric factors that predict complications during vaginal birth on scarred uterus were obtained as (Table 3); prematurity (OR = 7.4, CI = 1.627 - 34.027; p = 0.003), post-term (OR = 13.714, CI = 1.743 - 107.903; p = 0.002), history of CPD in previous caesarian (OR = 6.640, CI = 2.336 - 18.398; p ≤ 0.001), the number of ANC less than 4 (OR = 3.621, CI = 1.671 - 7.822; p = 0.01) ANC care in a Health Centre (OR =
Table 1. Socio-demographic characteristics.
Table 2. Complications obtained from the group of cases (N = 89).
Table 3. Clinical and obstetrical variables associated with complications during vaginal delivery on single scarred uterus.
2.758, CI = 1.397 - 5.444; p = 0.003) and by a nurse (OR = 2.387, CI = 1.203 - 4.733; p = 0.012), reference of the parturient by a different hospital.
Morbidity during delivery was found to be associated neither with parity nor gravidity. Previous surgery (caesarian or myomectomy) could not predict complications during subsequent deliveries. No statistically significant association was found between complications during birth and pathologies during pregnancy.
The risk factors for fœtal complications during vaginal birth on scarred uterus obtained was a meconium stained amniotic fluid. (OR = 9.900, CI = 3.644 - 26.898; p < 0.001).
Factors found to be independently associated with complications after logistic regression were post-term, absence of previous vaginal delivery on a scarred uterus ; the indication of the caesarian being a cephalo pelvic disproportion (CPD), a Bishop score less than 7 and a meconium stained amniotic fluid (Table 4).
The protective factors obtained for morbidity in women with single scarred uterus during delivery were: being a worker in the private sector (OR = 0.247, CI = 0.006 - 0.919; p = 0.026), delivery within the normal term (OR = 0.415, CI = 0.226 - 0.761; p = 0.004), ANC follow up in a reference hospital and by a specialist/obstetrician (OR = 0.432, CI = 0.226 - 0.826; p = 0.010). Normal fetal weight was rather a factor in favour of success of a trial of scar.
4. Discussion
Our study revealed that among socio-demographic variables, we did not find a significant risk of complications for VBAC.
Prematurity is a risk factor for complications during breech delivery found in this study and contrary to previous literature. Quinones et al. in the USA in 2005, [9] showed in their series that there was a higher rate of success during trial of scar with preterm delivery compared to term delivery with respective percentages of 82% and 74% thus implying preterm deliveries reduce the risk of uterine rupture. This dissimilarity could be explained by the fact that in the context of this study, preterm deliveries were treated as emergencies and systematically by caesarian.
A gestational age greater than or equal to 42 weeks was found to be associated with complications during VBAC. Our finding is concordant with that available in literature. Landon et al. showed that a gestational age greater than 41 weeks is a risk factor for failure during VBAC [10] . Also, Ola et al. working in Nigeria found that post-term is a
Table 4. Clinical and obstetrical variables associated with complications during vaginal delivery on single scarred uterus after logistic regression.
risk factor for failure of trial of scar [11] . Moreso, post-term is a well known cause of fœtal distress which consequently increases the risk of caesarian delivery [11] . Post- term is associated to fœtal macrosomia which in turn increases the risk of dystocia.
In our work, we have observed that the absence of prior vaginal delivery after a scar increases the risk of complications during vaginal delivery on a single scarred uterus. This is similar to findings in previous literature [7] [8] [10] [11] . In fact, there was a higher probability of success if there had been a prior vaginal delivery after a caesarian. This could be explained by the fact that women who had never been subjected to a trial of scar were less prepared psychologically compared to their counterparts who already had successful trial of scar. And prior delivery on a scar uterus demonstrate the solidity of the scar that make the consultant confident about the issue of the delivery
An interpregnancy spacing (uterine rest period) greater than or equal to 60 months (5 years), was shown as a risk factor for failure of VBAC. But no study, to the best of our knowledge, has confirmed this observation. Above 60 months, the uterus loses its elasticity as fibrosis sets in and could explain our result.
The cephalo-pelvic disproportion (CPD) indicated during the first caesarian section was found to be associated with complications during breech delivery on scarred uterus. This finding is similar to that of Flamm et al. and Hashima et al. in USA in 1999 and to that of Lehmann in France in 2004 [12] [13] . This could be explained on the one hand by a tendency of repetition of CPD and on the other hand by increase in fetal weight with parity.
Less than 4 ANC were statistically associated to complications during delivery. This was even more severe with VBAC with the risk of complication increased by a factor of 3 if the parturient failed to respect WHO recommendations [14] . In addition, a study done in Cameroon in 2012 showed that only 60% of parturients had at least 4 ANC visits [14] . This suggests that a poor ANC care increases the risk of maternal morbidity and mortality on non-scarred uterus as well as on scarred uterus [15] .
Antenatal care (ANC) done in a health centre and by a nurse constituted risk factors for complications during vaginal delivery on scarred uterus. This finding is similar to that of Foumane et al. in a study in Yaoundé, Cameroon in 2014 which showed that antenatal care in a Health Centre is a predisposing factor for emergency caesarian section [16] . As a matter of fact, these women live nearer to these health centres and thus spent less financially and time wise compared to reference hospitals. Antenatal care by an obstetrician was found to be a protective factor as the obstetrician has the competence to follow up high risk pregnancies and can take care of complications without referring the parturient which could constitute a delay in treatment.
Patients referred from other Health structures had higher risk of complications during delivery. Foumane et al. found that referred parturients are 27 times more likely to deliver by an emergency caesarian section [16] . Indeed, such women were followed up and had desired to put to birth in these first level health structures which do not have the competence for emergency obstetrical and neonatal care. This thus obliges them to refer parturients to tertiary level health structures and sometimes went maternal and/or neonatal health are already in jeopardy.
An unfavourable Bishop score (<7) was found to increased the risk of complications during vaginal delivery on scarred uterus by a factor of 12. Lehman et al. in 1999 workin in France, found that a favourable Bishop score was predicitive of successful out during VBAC [13] while Weinstein et al. showed that a Bishop score less than 4, increases the risk of complications during vaginal delivery on scarred uterus [17] [18] . The Bishop score due to its relevant clinical parameters could therefore be an important tool in decision making on the mode of delivery. Thus in the case of CPD, which was the first indication of emergency cesarian in our study, the bishop score should be low.
In our study population, there was no statistical significance between labour induction or augmentation and morbidity during vaginal birth on a scarred uterus. The Canadian association of Gynaecologists and Obstetricians strictly prohibits the use of prostaglandins (misoprostol) for induction of labour on scarred uterus [19] . However, a study done in France in 2014 supported the use of a foley catheter for cervical ripening in parturients with single scarred uterus but with a failure rate of trial of scar of about 56.5% [20] [21] .
Current literature supports the fact that the use of oxytocics is associated with an increased risk of failure during trial of scar. This dissimilarity with our study could be explained by the fact that most parturients in this study did not need to be induced as they went into labour spontaneously. Moreover, the service protocol at the YGOPH does not authorize the use of oxytocin for augmentation of labor in women in with scarred uterus.
5. Conclusions
The independent factors associate to complications during vaginal delivery on single scarred uterus after multivariate logistic regression are: post-term, no prior vaginal delivery after scar, indication of previous caesarian being CPD, and a Bishop score less than 7.
It is important in our environment, to consider caesarian indications from the outset, or prepare the parturient for an eventual cesarean section when faced with one of these factors.
6. Limitations of the Study
The retrospective collection of data subjected the study to certain bias notably the reliability of information collected from medical files, the lack of uniformity in post operative notes, incomplete information on previous procedures.
Cite this paper
Meka, E.N.U., Fou- mane, P., Essiben, F., Ngwesse, E.R., Sama, J.D. and Mboudou, E.T. (2016) Predictive Factors of Complications of Vaginal Delivery on Scarred Uterus at the Yaoundé Gy- naeco-Obstetric and Paediatric Hospital. Open Journal of Obstetrics and Gynecology, 6, 851- 860. http://dx.doi.org/10.4236/ojog.2016.613103
References
- 1. Nkwabong, E., Kouam, L., Wamba, T., Ngassa, P., Doh, A.S., Mve, K.V., Takang, W. and Ekono, M.R. (2006) Indication des césariennes a la maternité du CHU de Yaoundé de 2000: A 2004 Clinics. Mother and Child Health, 3, 453-455.
- 2. Kemfang Ngowa, J.D., Ngassam, A., Tsuala Fouogue, J., Metogo, J., Medou, A. and Kasia, J.M. (2015) Complications maternelles précoces de la césarienne: à propos de 460 cas dans deux hopitaux universitaires de Yaoundé, Cameroun. The Pan African Medical Journal, 21, 265.
- 3. Cecatti, J.G. (2015) Antibiotic prophylaxis for caesarean section: Commentaire de la BSG.
- 4. Deneux-Tharaux, C. (2012) Utérus cicatriciel: Aspects épidémiologiques. Journal de Gynécologie Obstétrique et Biologie de la Reproduction, 41, 697-707.
https://doi.org/10.1016/j.jgyn.2012.09.022 - 5. Morin, C. and Rozenberg, P. (2010) Chapitre 56—Accouchement avec un utérus cicatriciel. In: Marpeau, L., Ed., Traité d’obstétrique, Elsevier Masson, Paris, 441-446.
http://www.sciencedirect.com/science/article/pii/B9782294071430500561 - 6. Haumonté, J.-B., Raylet, M., Sabiani, L., Franké, O., Bretelle, F., Boubli, L., et al. (2012) Quels facteurs influencent la voie d’accouchement en cas de tentative de voie basse sur utérus cicatriciel? Journal de Gynécologie Obstétrique et Biologie de la Reproduction, 41, 735-752.
https://doi.org/10.1016/j.jgyn.2012.09.032 - 7. Halle Ekane, G.E., Djoukam, Tchuente Nguefack, C., Tchounzou, R., Atashili, J., Mangala Nkwele, G., Mokube, M. and Egbe Obinchemti, T. (2015) Outcome of Delivery after a Previous Caesarean Section at the Department of Obstetrics and Gynecology, Limbe Regional Hospital, Cameroon: A Retrospective Study. African Journal of Integrated Health, 5, 24-30.
- 8. Flamm, B.L. and Geiger, A.M. (1997) Vaginal Birth after Cesarean Delivery: An Admission Scoring System. Obstetrics & Gynecology, 90, 907-910.
https://doi.org/10.1016/S0029-7844(97)00531-0 - 9. Quinones, J.N., Stamilio, D.M., Pare, E., Peipert, J.F., Stevens, E. and Macones, G.A. (2005) The Effect of Prematurity on Vaginal Birth after Cesarean Delivery: Success and Maternal Morbidity. Obstetrics & Gynecology, 105, 519-524.
https://doi.org/10.1097/01.AOG.0000153493.15922.85 - 10. Landon, M.B., Leindecker, S., Spong, C.Y., Hauth, J.C., Bloom, S., Varner, M.W., et al. (2005) The MFMU Cesarean Registry: Factors Affecting the Success of Trial of Labor after Previous Cesarean Delivery. American Journal of Obstetrics & Gynecology, 193, 1016-1023.
https://doi.org/10.1016/j.ajog.2005.05.066 - 11. Ola, E., Imosemi, O. and Abudu, O. (2000) Vaginal Birth after One Previous Caesarean Section-Evaluation of Predictive Factors. African Journal of Medicine and Medical Sciences, 30, 61-66.
- 12. Hashima, J.N., Eden, K.B., Osterweil, P., Nygren, P. and Guise, J.-M. (2004) Predicting Vaginal Birth after Cesarean Delivery: A Review of Prognostic Factors and Screening Tools. American Journal of Obstetrics & Gynecology, 190, 547-555.
https://doi.org/10.1016/j.ajog.2003.08.045 - 13. Schlesselman, J. (1974) Sample Size Requirements in Case-Control Studies of Disease. American Journal of Epidemiology, 99, 381-384.
- 14. Lehmann, M., Hedelin, G., Sorgue, C., Gollner, J.-L., Grall, C., Chami, A., et al. (1999) Facteurs prédictifs de la voie d’accouchement des femmes ayant un utérus cicatriciel. Journal de Gynécologie Obstétrique et Biologie de la Reproduction, 28, 358-368.
- 15. Bonono, R.C. and Ongolo-Zogo, P. (2012) Optimiser l’utilisation de la consultation prénatale au Cameroun. Centre pour le Développement des Bonnes Pratique en Santé.
- 16. Fomulu, F.J., Ngassa, P.N., Nong, T., Nana, P. and Nkwabong, E. (2013) Mortalité maternelle à la maternité du Centre Hospitalier et Universitaire de Yaoundé, Cameroun: étude rétrospective de 5 ans (2002-2006). Health Sciences and Disease, 10, 86-92.
http://hsd-fmsb.org/index.php/hsd/article/view/49 - 17. Foumane, P., Koh, V.M., Minkande, J.Z., Ngantcha, E.A.N., Dohbit, J.S. and Mboudou, E.T. (2014) Facteurs de risque et pronostic des césariennes d’urgence à l’Hopital Gynéco-Obstétrique et Pédiatrique de Yaoundé (Cameroun). Medecine et Sante Tropicales, 24, 89-93.
- 18. Weinstein, D., Benshushan, A., Tanos, V., Zilberstein, R. and Rojansky, N. (1996) Predictive Score for Vaginal Birth after Cesarean Section. American Journal of Obstetrics & Gynecology, 174, 192-198
https://doi.org/10.1016/S0002-9378(96)70393-9 - 19. Martel, M.-J. and MacKinnon, C. (2005) Directive clinique sur l’accouchement vaginal chez les patients ayant déjà subi une césarienne. Journal of Obstetrics and Gynaecology Canada, 27, 175-188
https://doi.org/10.1016/S1701-2163(16)30189-X - 20. Lamourdedieu, C., Gnisci, A., Marcelli, M., Heckenroth, H., Gamerre, M. and Agostini, A. (2015) Maturation cervical des utérus unicicatriciels à la sonde de Foley: Etude prospective de 41 patientes. Journal de Gynécologie Obstétrique et Biologie de la Reproduction, 44, 426-432
https://doi.org/10.1016/j.jgyn.2014.07.014 - 21. Fournié, A., Connan, L., Parant, O. and et Lesourd-Pontonnier, F. (1999) Souffrance foetale aigue. Obstétrique. 5-077-A-30, Encyclo Med Chir, Elsevier, Paris, 11 p.


