Open Journal of Clinical Diagnostics
Vol.3 No.3(2013), Article ID:37227,4 pages DOI:10.4236/ojcd.2013.33018
Resident accuracy in locating the common femoral vein in normal weight vs. obese patients
![]()
Department of Emergency Medicine, East Carolina University, Greenville, USA
Email: *pattersonl@ecu.edu
Copyright © 2013 Leigh Patterson et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 26 June 2013; revised 26 July 2013; accepted 3 August 2013
Keywords: Ultrasound; Central Venous Access; Obesity
ABSTRACT
Objectives: Ultrasound guidance increases the success of internal jugular central venous catheter (CVC) placement. The common femoral vein (CFV) is considered an easier site and physicians frequently place CFV CVCs using anatomical landmark guidance. No research has demonstrated the effect of patient weight on placement of a femoral CVC. The authors hypothesized that resident physicians could determine by anatomical landmarks the insertion site of a femoral CVC in normal and overweight adults. Methods: Investigators consented adult patients in the Emergency Department to serve as study models. Patients were grouped by BMI: Normal (BMI < 25) and Overweight (BMI > 25). PGYI-III Emergency Medicine residents who volunteered to participate were included. Residents inspected and palpated the inguinal regions on a patient and marked the patient’s skin directly over the CFV. A faculty member assessed success using a 10 MHz linear probe (Sonosite Micro Maxx) centered over the mark. The attempt was successful if the mark was directly over the CFV and unsuccessful if distal, lateral, or medial to the CFV. Results: Nineteen residents (6 PGYI, 7 PGY II, and 6 PGYIII) assessed 17 patients. There were 43 attempts on Normal patients and 57 attempts on Overweight patients. The success rate on Normal patients was 74% and on Overweight patients was 42% (p = 0.0021). Conclusion: Residents were more successful in correctly identifying the CFV by anatomical landmarks in Normal patients. Training year had no effect on success. Ultrasound guidance may increase the success rate of placing a femoral CVC in patients with BMI > 25.
1. INTRODUCTION
The placement of a central venous line is a common and vital procedure in the emergency department in the treatment of patients in whom peripheral access is unobtainable or in whom invasive monitoring, cardiac pacing, or infusions of vaso-active agents are needed quickly. Research has shown that the use of ultrasound can reduce complications of central line placement and decrease the length of time needed to perform the procedure [1-4]. Many of these studies have focused on accessing the internal jugular vein, since this is a site that allows for invasive monitoring, but carries risk for serious complication such as pneumothorax, hematoma, line misplacement, and hemothorax. One such study showed the emergency department complication rate of placing internal jugular CVCs to be between 10% and 15% [5]. Given this rate of complications, data has supported the use of ultrasound for the placement of internal jugular central venous access.
The femoral vein (CFV) provides an alternative site that can be accessed emergently for central vascular access. The CFV is considered an easier location to insert a central line and is associated with fewer complications including a reduced risk of infection and thromboembolic disease [6]. During certain situations, such as a complicated intubation or the performance of cardiopulmonary resuscitation, the CFV may be the only central vein available for access. With fewer complications and the easier anatomy, the CFV can be accessed without the aid of ultrasound. However, studies examining the use of ultrasound on femoral vein access have shown ultrasound to be superior to landmark guided technique. One study showed ultrasound-guided CFV cannulation to have a first stick success rate of 93% compared to 55% in the landmark alone group [7]. In addition, total procedure time was significantly reduced, but time to access was not significantly affected. There has been no research that describes what factors may affect the success in accessing the CFV and predicting the need for US guidance. The goal of this investigation was to determine if patient body mass index (BMI) or level of physician training affected the ability to accurately determine the proper site for accessing the femoral vein using the landmark technique.
2. METHODS
All procedures were approved by The University and Medical Center Institutional Review Board of East Carolina University.
Study Design: This was an observational study of Emergency Medicine residents in all three years of a PGY I-III year program.
Study Setting and Population: The study was conducted at an academic emergency department with an annual census of approximately 80,000 patient visits per year. The total number of residents enrolled was 19. The total number of patients was 17, eight males and nine females. The patients used were adults with ages ranging from 33 - 90 yrs of age and body mass index ranged from 18 - 48.
Study Protocol: Patients who were currently receiving care in the emergency department were randomly selected and asked to serve as models for the study. Written consent was obtained from the patients and from the resident physicians who participated. After consents were obtained, residents were asked to evaluate each patient using landmarks as if they were going to place a central venous line in the CFV. Once they felt they had determined the accurate site for vascular access using landmarks they used a washable skin marker to place a dot directly superficial to the CFV, the area in which they would introduce the seeker needle had this been a real attempt. This was done on both the right and left legs of the patient. Each leg marked was considered a single attempt. After marking both legs, the resident then left the room and ultrasound confirmation was obtained.
An ultrasound image of the common femoral vein (Figure 1) was obtained by placing a 10 MHz linear probe (Sonosite MicroMaxx) centered over the resident’s mark. The attempt was considered accurate if the mark was placed directly over the common femoral vein or unsuccessful if the mark was placed distal, lateral, or medial to the common femoral vein. The ultrasounds were performed by a single attending. Each resident evaluated 2 - 4 patients depending on the availability of patients. The residents were not given feedback on their performance until data collection was completed.
Measurements: Results were recorded on a data sheet with patient demographic information including age, height, and weight. The data was entered in a spreadsheet divided by accuracy on the right and left leg, level of residency training, and patient’s BMI. Body mass index

Figure 1. Ultrasound image of the left common femoral vein and artery before (left) and after (right) compression.
was divided into two groups. Patients with a BMI greater than 25 were considered overweight and a BMI less than 25 were considered normal. Ten patients had a BMI > 25 and seven patients had a BMI < 25.
Data Analysis: The rate of successfully indicating the correct spot for cannulation of the CFV was compared between BMI groups, between sides of body (left vs. right) and across levels of training using a Fisher’s Exact test or chi-square test as appropriate. P < 0.05 indicated statistical significance. Sensitivity and specificity of using the landmark technique in determining proper placement of CFV cannula were calculated and reported as a percentage with 95% confidence intervals.
3. RESULTS
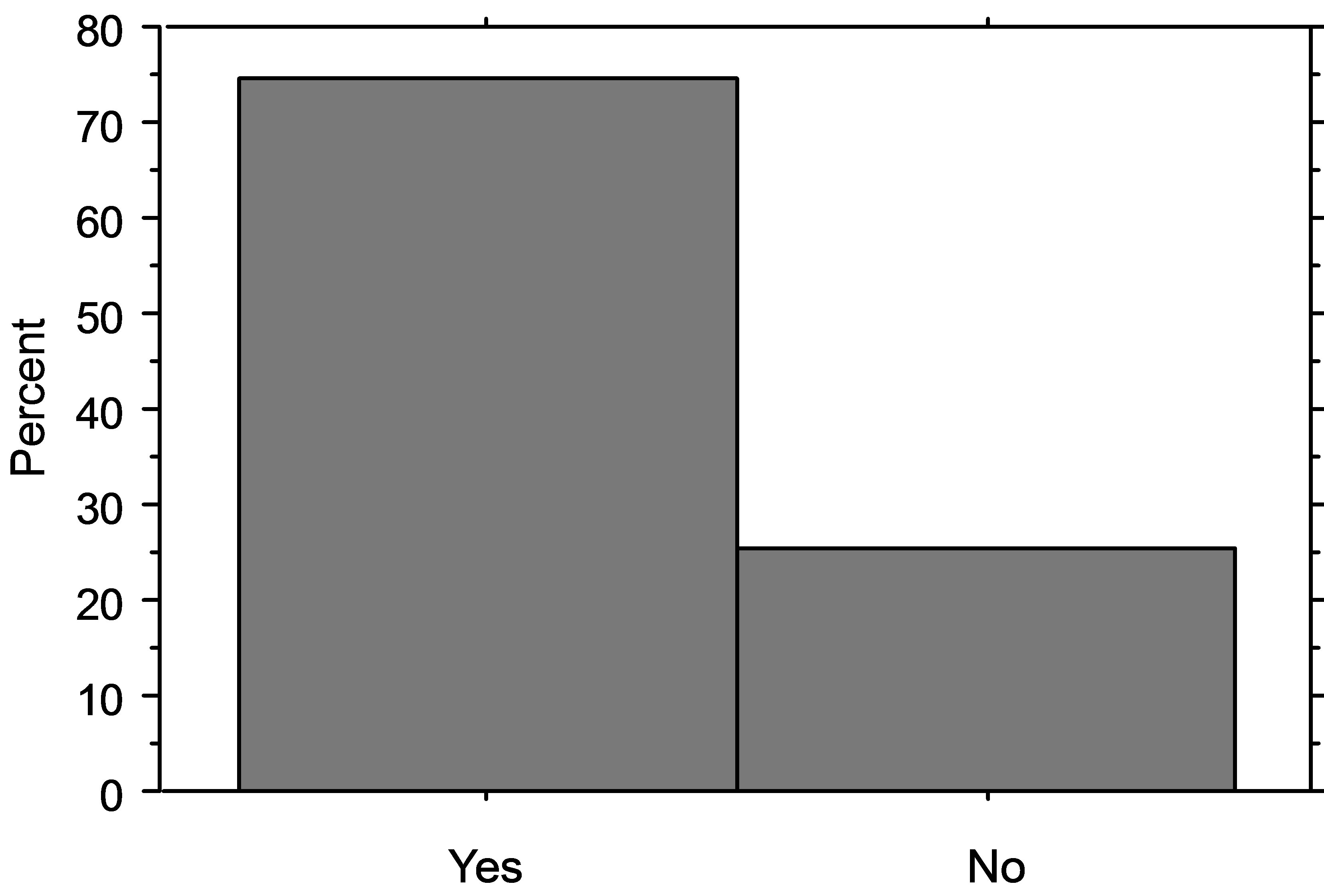
Residents marked 43 attempts on patients with BMI < 25 and 57 attempts on patients with BMI > 25, for a total of 100 data points. The CFV was accurately located in 56% of attempts overall. There was no significant difference in the accuracy between left and right legs (59% vs. 53% p = 0.55). The accuracy rate for locating the CFV on patients with BMI < 25 was 74% compared to 42% on patients with BMI > 25 (p = 0.02) (Figure 2).
The accuracy rate for 3rd year residents overall was 53%, for 2nd year residents was 58%, and for 1st year residents it was 57% (p = 0.25). The sensitivity and specificity for using landmarks to correctly locate the CFV in patients with a BMI > 25 was 42.1% (95% CI = 29.4 - 55.9) and 25.6% (95% CI = 14.0 - 41.5), respectively.
Limitations: Our study asked residents to use markers to place a dot over the femoral vein based on landmarks. While this non-invasive method allowed residents to identify the location of the CFV with minimal risk to
 BMI < 25
BMI < 25  BMI > 25
BMI > 25
Figure 2. The rate of success is significantly lower in patients with BMI > 25 (42%) than those with BMI < 25 (74%) (p = 0.002).
patient volunteers, it does not account for the additional complexities of actual catheter placement including the correct angle of entry or distance between the skin and anterior vein wall. If the resident has the correct site but not the correct depth success cannot be guaranteed. Though the markers are no replacement for actual needle sticks to determine success, they do allow assessment of resident’s ability to use landmarks for placing a femoral CVC.
Future research should study actual placement of central lines in the CFV and record time of procedure, number or attempts, and complications using landmark technique in placing a central line in the common femoral vein. With this data one could compare the different BMI groups to see if there is a significant difference between the two groups. Additionally, the impact of body mass index on placing lines in the subclavian vein or internal jugular vein should be assessed.
4. DISCUSSION
Previous studies have shown ultrasound guidance to decrease complications of central venous access and increase success rates in accessing the internal jugular vein [1-4]. Other studies have also shown this to be true for the femoral vein [5-7]. However, ultrasound may not be readily available or may be seen as an added step that will increase time to vascular access. Research focusing on ultrasound guided femoral access versus landmark techniques have been done, but since the femoral vein is associated with less risk, the question remains as to whether ultrasound is needed, given the extra time and training required for ultrasound guidance. When weighing the risks and benefits of whether to use ultrasound for placing a femoral line, one would like to know if there are predictors of success that would favor the use or non-use of ultrasound when placing a femoral line. Our study attempted to assess whether patient’s weight or a resident’s level of training affected the ability of a resident to accurately identify the CFV by anatomical landmarks. We assume that if these indicators negatively affected success, they could predict the need for US guidance when accessing the CFV. The overall success rate found in our subjects when using anatomical landmarks is similar to that reported by others when accessing the CFV [7]. Our data showed level of training beyond the intern year did not have a significant affect on success rates. However, residents were significantly more successful in identifying the CFV using anatomical landmarks in patients with BMI < 25. Therefore, when attempting to access the CFV for a central line, ultrasound should be highly considered in patients with body mass index greater than 25.
5. CONCLUSION
Our study looked at two predictors when considering using ultrasound for central venous access in the common femoral vein. Our study showed that the level of training did not offer a significant prediction of success, but BMI of the patient did. The use of ultrasound may be able to increase the success rate of placing a central venous line in patients with BMI greater than 25.
REFERENCES
- Karakitsos, D., et al. (2006) Real-time ultrasound-guided catheterisation of the internal jugular vein: A prospective comparison with the landmark technique in critical care patients. Critical Care, 10, R162. doi:10.1186/cc5101
- Leung, J., Duffy, M. and Finckh, A. (2006) Real-time ultrasonographically-guided internal jugular vein catheterization in the emergency department increases success rates and reduces complications: A randomized, prospective study. Annals of Emergency Medicine, 48, 540-547. doi:10.1016/j.annemergmed.2006.01.011
- Mey, U., et al. (2003) Evaluation of an ultrasound-guided technique for central venous access via the internal jugular vein in 493 patients. Support Care Cancer, 11, 148- 155.
- Milling Jr., T.J., et al. (2005) Randomized, controlled clinical trial of point-of-care limited ultrasonography assistance of central venous cannulation: The Third Sonography Outcomes Assessment Program (SOAP-3) Trial. Critical Care Medicine, 33, 1764-1769. doi:10.1097/01.CCM.0000171533.92856.E5
- Steele, R. and Irvin, C.B. (2001) Central line mechanical complication rate in emergency medicine patients. Academic Emergency Medicine, 8, 204-207. doi:10.1111/j.1553-2712.2001.tb01292.x
- Merrer, J., et al. (2001) Complications of femoral and subclavian venous catheterization in critically ill patients: A randomized controlled trial. JAMA, 286, 700-707. doi:10.1001/jama.286.6.700
- Kwon, T.H., Kim, Y.L. and Cho, D.K. (1997) Ultrasoundguided cannulation of the femoral vein for acute haemodialysis access. Nephrology Dialysis Transplantation, 12, 1009-1012. doi:10.1093/ndt/12.5.1009
NOTES
*Corresponding author.

