Open Journal of Immunology
Vol.4 No.2(2014), Article
ID:47090,6
pages
DOI:10.4236/oji.2014.42008
Seroprevalence of and Risk Factors for Cytomegalovirus among HIV-Infected Patients at University of Maiduguri Teaching Hospital, Nigeria
Ibrahim Musa Kida1, Ballah Akawu Denue1*, Bukar Bakki1, Baba Goni Waru1, Mohammed Abdullahi Talle1, Ibrahim Ummate1, Salisu Aliyu Kwayabura2, Ibrahim Shettima Kuburi1, Haruna Yusuph1
1Department of Medicine, College of Medical Sciences, University of Maiduguri, Maiduguri, Nigeria
2Department of Obstetrics and Gynaecology, College of Medical Sciences, University of Maiduguri, Maiduguri, Nigeria.
Email: *d_akawu@yahoo.co.uk
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 10 April 2014; revised 10 May 2014; accepted 12 June 2014
ABSTRACT
Although the distribution of cytomegalovirus (CMV) infection has a wide regional variation, it is more common in Africa and Asia with high prevalence approaching 100% in some communities. CMV is a frequent opportunistic infection and major cause of morbidity and mortality among HIV patients with severe immunosuppression. It can be contracted from body fluid, including saliva, urine, blood, cervical secretions, and semen. CMV seropositivity is considered the best laboratory measure of past infection. We determined the prevalence of CMV and the risk factors associated with its acquisition in a population of HIV positive patients. Anti-CMV IgG seroprevalence was 100% among HIV infected subjects and 98.6% among controls. Having multiple sexual partners and traditional practices were identified as risk factors associated with risk of contracting CMV infection.
Keywords:CMV Cytomegalovirus, HIV Human Immunodeficiency Virus, AIDS Acquired Immunodeficiency Syndrome, IgG Immunoglobulin

1. Introduction
Cytomegalovirus (CMV) is a ubiquitous infection with estimated seropositivity among adults ranging from 40% - 79% in western countries to 96% - 100% in Africa and Asia [1] . Human CMV may be transmitted from a variety of sources, including saliva, urine, blood, cervical secretions, and semen [2] . Although primary CMV infection is usually benign, the virus remains latent within the host, this characteristic is also exhibited by other herpesviruses [3] [4] . Under conditions of immune compromise, especially impairment of cell-mediated immunity as seen in HIV infected patients, latent virus may reactivate to produce a variety of clinical syndromes, including chorioretinitis, oesophagitis, colitis, pneumonia, encephalitis, and adrenalitis [5] [6] .
Autopsy and clinical studies indicate that 90% of patients with AIDS develop active CMV infection during their illness, with life or sight-threatening complication in about 25% attributable to direct effect of the virus [6] [7] . Dual infections may thus provide the potential for adverse virus-virus interaction including increase in sexual transmission.
The prevalence of infection in a given population can only be reliably estimated by laboratory testing as clinical symptoms are usually absent. Cytomegalovirus seropositivity is considered as the best laboratory measure of past infection [8] .
Determination of local CMV seroprevalence is important especially in regions where the infection is perceived to be common. This will assist identifying risk factors for its acquisition and developing prevention strategies. To the best of our knowledge, there are hitherto no seroepidemiological data available on the prevalence of CMV infection in HIV patients in north east Nigeria. We carried out a serological screening for IgG antibody to CMV (antiCMV) and determined the risk factors associated with acquisition of CMV infection in a population of HIV positive patients.
2. Methods
One hundred and eighty subjects including 100 newly diagnosed ART naïve, HIV-positive patients and 80 apparently healthy HIV negative individuals were consecutively recruited into the study. Consent was obtained from the participants, participation was voluntary, the benefits and risks if any were explained to the patients. Detailed history and information on socio-demographic characteristics were obtained using a structured questionnaire. A thorough clinical examination was done on each participant. Human IgG antibody to human CMV was detected using enzyme-linked immunosorbent assay (ELISA) (Calbiotech®). Human immunodeficiency virus infection was screened for and confirmed using ELISA and Western blot techniques respectively. Diagnosis of AIDS was established by the CDC clinical criteria and/or CD4+ cell count of <200 cells/µL [9] . SPSS version 11.0 (SPSS, Chicago, Illinois, USA) was used for statistical analysis. Continuous variables were expressed as mean ± standard deviation. Differences were determined using Chi-square test with Yates correction. A p value of <0.05 was considered significant.
Ethical approval for the study was obtained from the Research and Ethics Committee of the University of Maiduguri Teaching Hospital.
3. Results
Among the 100 HIV-positive subjects 34 were males and 66 females, (male to female ratio = 1:1.9). Amongst the 80 controls, 40 were males and 40 females (male to female ratio = 1:1).The mean age of the subjects and controls were 31.82 ± 8.25 years and 29.00 ± 8.03 years respectively. Majority of the study population were less than 40 years (Figure 1).
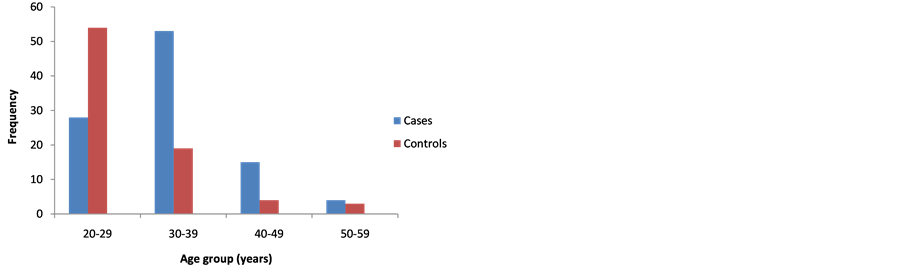
Figure 1. Age distribution of cases and controls.
The unschooled constituted the largest group among both cases (37%) and controls (60%). Many of the cases were unemployed (46% cases vs. 30% controls, p = 0.042) and from rural areas (60% cases vs. 44% controls, p = 0.044) (Table 1).
The mean CD4+ cell count of the HIV-positive cases was 223.5 cells/µL. Majority of the HIV positive patients had CD4+ counts < 200 cells/µL (Table 2).
The prevalence of anti-CMV IgG antibody was found to be 100% in the cases and 98.6% in the controls.
The distribution of risk factors for the acquisition of CMV infection between cases and controls in the study population is illustrated in Table 3. Having multiple sexual partners, traditional practices such as tattooing and cupping, and blood transfusion were significant risk factor among the cases. 4. Discussion We determined the seroprevalence of CMV among HIV positive patients and controls in a tertiary health institution north east Nigeria through detecting IgG antibody to CMV in the serum of participants. Seroprevalence of anti-CMV IgG was 100% among our HIV-infected cohort. This is in agreement with report from the Lagos University Teaching Hospital, south west Nigeria and Burkina Faso by Akinbami et al. [10] at and Ledru et al. [11] respectively that documented a prevalence of anti-CMV IgG antibody of 100% among HIV-infected patients. Table 1. Characteristics of CMV seropositive cases and controls. However Adjei et al. [12] reported a lower seroprevalence of 59.2% in Ghana. The higher mean CD4 count of their population may have contributed to this difference. The reported seroprevalence rate of 98.6% for CMV IgG among HIV-seronegative healthy controls is comparable to the rates of 97%, 96%, and 92% reported in Tunisia [13] , India [14] and north central Nigeria [15] respectively. These prevalence rates are higher than the figure recorded in another study by Olaleye et al. [16] in Ibadan, Nigeria where the authors found a prevalence of 54.6% among healthy blood donors. This may be attributed to differences in screening technique used. The prevalence rates reported in the aforementioned studies are higher than those reported in Western populations [17] . The high CMV seropositivity rate in this study is suggestive of widespread past exposure to infection and may explain the lack of statistically significant differences in the seroprevalence of CMV in HIV-seronegative healthy individuals and HIV-AIDS patients. The hyperendemicity of CMV infection in both HIV-seronegative individuals and HIV-seropositive patients poses a major threat to individuals at risk of CMV disease like HIV/AIDS patients. The reasons for the high prevalence may be an increase in the distribution of epidemiological risk factors prevalent in these areas, as well as lack of access to health information, education and communication. Majority of the subjects were either unschooled or had only primary education. This may be a reflection of the present poor state of education in Nigeria, which is more prevalent in these areas perhaps due to lack of proper commitment as well as poor governance at the local and state government levels [18] . Studies have shown lack of education or ignorance as one of the factors responsible for the acquisition of CMV infections [19] [20] . Having multiple sexual partners and blood transfusion were found to be significantly more in the cases than controls. Studies have shown sexual promiscuity and STDs to be associated with both HIV and CMV [21]
5. Conclusion/Recommendation
The high seroprevalence of CMV antibodies among both HIV-positive and HIV-negative individuals suggests endemicity of this infection in our environment. Sexual transmission and traditional practices plays a significant role in acquisition of CMV infections in this part of Nigeria, therefore health education on preventive measures is expedient with emphasis on identified risks of acquisition of CMV infection from this study.
Acknowledgements
We wish to acknowledge and thank the management of University of University of Maiduguri through its Research and Ethics committee for granting us permission to conduct this research and Mr Baba Sanda Bukar of the Immunology Department, University of Maiduguri Teaching who assisted in conducting ELISA and Western Blot tests on the samples.
Competing Interests
None.
Author Contributions
IMK, BAD, BB MAT, BGW, IU, ISK, SAK HY conceptualized the study, collected data and carried out the statistical analysis. IMK, BAD and BB wrote the manuscript.
References
- Ahmed, S.A., Al-Joudi, F.S., Wan Zaidah, A., et al. (2006) The Prevalence of Human Cytomegalovirus Seropositivity among Blood Donors at the Unit of Blood Transfusion Medicine, Hospital Universiti Sains Malaysia. Southeast Asian Journal of Tropical Medicine and Public Health, 37, 294-296.
- Chandler, S.H., Holmes, K.K., Wentworth, B.B., et al. (1985) The Epidemiology of Cytomegaloviral Infection in Women Attending a Sexually Transmitted Disease Clinic. The Journal of Infectious Diseases, 152, 597-605. http://dx.doi.org/10.1093/infdis/152.3.597
- Anderson, C.H. and Michaels, R.H. (1972) Cytomegalovirus Infection: Detection by Direct Fluorescent-Antibody Technique. Lancet, 2, 308-309. http://dx.doi.org/10.1016/S0140-6736(72)92910-8
- Armstrong, D., et al. (1985) Treatment of Infections in Patients with the Acquired Immunodeficiency Syndrome. Annals of Internal Medicine, 103, 738-743. http://dx.doi.org/10.7326/0003-4819-103-5-738
- Dietrich, D.T. and Rahmin, M. (1991) Cytomegalovirus Colitis in AIDS: Presentation in 44 Patients and a Review of the Literature. Journal of Acquired Immune Deficiency Syndromes, 4, 525-529.
- Drew, W.L. (1989) Cytomegalovirus Infection in Patients with AIDS. Journal of Infectious Diseases, 158, 449-456. http://dx.doi.org/10.1093/infdis/158.2.449
- Kreiss, J.K. and Castro, K.G. (1990) Special Consideration for Managing HIV Infection and AIDS in Patients from Developing Countries. Journal of Infectious Diseases, 162, 955-960. http://dx.doi.org/10.1093/infdis/162.4.955
- Cannon, M.J., Schmid, D.S. and Hyde, T.B. (2010) Review of Cytomegalovirus Seroprevalence and Demographic Characteristics Associated with Infection. Reviews in Medical Virology, 20, 202-213. http://dx.doi.org/10.1002/rmv.655
- Centers for Disease Control (1991) Review of Draft for Revision of HIV Infection Classification System and Expansion of AIDS Surveillance Case Definition. MMWR, 40, 787.
- Akinbami, A.A., Akanmu, A.S., Adeyemo, T.A., et al. (2009) Seroprevalence of CMV Antibodies among HIV Patients and Blood Donors at Lagos State University Teaching Hospital. South African Medical Journal, 99, 528-530.
- Ledru, E., Diagbouga, S., Ledru, S., et al. (1995) A study of Toxoplasma and Cytomegalovirus Serology in Tuberculosis and in HIV-Infected Patients in Burkina Faso. Acta Tropica, 59, 149-154. http://dx.doi.org/10.1016/0001-706X(95)00073-N
- Adjei, A.A., Armah, H.B., Gbagbo, F., et al. (2008) Seroprevalence of HHV-8, CMV, and EBV among the General Population in Ghana, West Africa. BMC Infectious Diseases, 8, 111-118. http://dx.doi.org/10.1186/1471-2334-8-111
- Gargouri, J., Elleuch, H., Karray, H., Rekik, H. and Hammami, A. (2000) Prevalence of Anti-CMV Antibodies in Blood Donors in the Sfax Region (Value in Blood Transfusion). La Tunisie Médicale, 78, 512-517.
- Kothari, A., Ramachandran, V.G., Gupta, P., Singh, B. and Talwar, V. (2002) Seroprevalence of Cytomegalovirus among Voluntary BLOOD donors in Delhi, India. Journal of Health, Population and Nutrition, 20, 348-351.
- Alao, O.O., Joseph, D.E., Mamman, A. and Banwat, E.B. (2008) The Seroprevalence of Cytomegalovirus Antibodies among Prospective Blood Donors in Jos. Nigerian Journal of Medicine, 17, 198-200. http://dx.doi.org/10.4314/njm.v17i2.37383
- Olaleye, O.D., Omilabu, S.A. and Baba, S.S. (1990) Cytomegalovirus Infection among Tuberculosis Patients in a Chest Hospital in Nigeria. Comparative Immunology, Microbiology and Infectious Diseases, 13, 101-106. http://dx.doi.org/10.1016/0147-9571(90)90522-U
- Bowden, R.A., Sayers, M., Flournoy, N., et al. (1986) Cytomegalovirus Immune Globulin and Seronegative Blood Products to Prevent Primary Cytomegalovirus Infection after Marrow Transplantation. The New England Journal of Medicine, 314, 1006-1010. http://dx.doi.org/10.1056/NEJM198604173141602
- Federal Ministry of Health, Nigeria (2005) National HIV/Syphillis Seroprevalence Sentinel Survey. Bosaca News, 1, 10-14.
- Dowd, J.B., Aiello, A.E. and Alley, D.E. (2009) Socioeconomic Disparities in the Seroprevalence of Cytomegalovirus Infection in the US Population: NHANES III. Epidemiology & Infection, 137, 58-65. http://dx.doi.org/10.1017/S0950268808000551
- Kenneson, A. and Cannon, M.J. (2007) Review and Meta-Analysis of the Epidemiology of Congenital Cytomegalovirus (CMV) Infection. Reviews in Medical Virology, 17, 253-276. http://dx.doi.org/10.1002/rmv.535
- Clarke, L.M., Duerr, A., Feldman, J., et al. (1996) Factors Associated with Cytomegalovirus Infection among Human Immunodeficiency Virus Type 1-Seronegative and-Seropositive Women from an Urban Minority Community. Journal of Infectious Diseases, 173, 77-82. http://dx.doi.org/10.1093/infdis/173.1.77
- Wester, C.W., Bussman, H., Moyo, S., et al. (2006) Serological Evidence of HIV-Associated Infections among HIV-1-infected Adults in Botswana. Clinical Infectious Diseases, 43, 1612-1615. http://dx.doi.org/10.1086/508865
- de Ory Manchón, F., Sanz Moreno, J.C., Castaneda López, R., et al. (2001) Cytomegalovirus Seroepidemiology in the Community of Madrid. Revista Espanola de de Salud Pública, 75, 55-62. http://dx.doi.org/10.1590/S1135-57272001000100007
- Williams, J.D., Fagbami, A.H. and Omilabu, S.A. (1989) Cytomegalovirus (CMV) Antibodies in Nigeria. Transactions of the Royal Society of Tropical Medicine, 83, 260. http://dx.doi.org/10.1016/0035-9203(89)90671-8
- Ghebrekidan, H., Rudén, U., Cox, S., Wahren, B. and Grandien, M. (1999) Prevalence of Herpes Simplex Virus Types 1 and 2, Cytomegalovirus, and Varicella-Zoster Virus Infections in Eritrea. Journal of Clinical Virology, 12, 53-64. http://dx.doi.org/10.1016/S0928-0197(98)00064-6
NOTES

*Corresponding author.


