Case Reports in Clinical Medicine
Vol.06 No.01(2017), Article ID:73595,7 pages
10.4236/crcm.2017.61003
Intravesical Migration of Intrauterine Device and Calculi Formation 12 Years Post Missing: A Case Report
Ahmad Rezaee Azandaryani1, Pezhman Ghaderzadeh1, Leili Ebrahimi Farsangi2*
1Radiology Department, Hamadan University of Medical Sciences, Besat Hospital, Hamadan, Iran
2Cardiology Department, Alborz University of Medical Sciences, Karaj, Iran

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: November 20, 2016; Accepted: January 16, 2017; Published: January 19, 2017
ABSTRACT
Intraunterine device (IUD) is a safe, effective and feasible method used for reversible contraception worldwide. Transvesical migration of an Intrauterine device (IUD) is a rare complication. We describe a case in whom initially a plain abdominopelvic radiography demonstrated calcified string of an IUD in a 42-year-old woman with recurrent lower urinary symptoms (LUTS) and urinary tract infection since 2 years earlier. The IUD had been inserted 12 years earlier and 3 years after placement of the IUD, the patient experienced an uneventful pregnancy and a successful delivery. Sonographic images and later on the cystoscopic procedure confirmed the diagnosis of transvesical migration of the IUD. The IUD was removed using cystoscopic procedure, leaving no complication.
Keywords:
Bladder Stone, Intrauterine Contraceptive Device, Intravesical Migration

1. Introduction
Currently, Intrauterine device (IUD) is a safe, cheap, effective and feasible method used for reversible contraception by nearly 100 million women worldwide, mainly because of its high efficiency and low complication rate [1] [2] [3] . IUD could cause complications ranged from mild discomfort to sepsis leading to death [4] . Some of its uncommon complications include infection, bleeding, ectopic pregnancy and uterine perforation [5] [6] . Uterine perforation by IUD can occur in an incidence of 1 - 3 in 1000 insertions [7] . The precise reason behind migration of IUD to organs and cavity near the uterus is unknown. Even so, misplacement or transvesical migration of IUD is a very infrequent complication and a high proportion of them form calculus [3] [8] . We present this case in order to note that recurrent urinary tract infection (UTI), lower urinary tract symptoms (LUTS) and unexpected pregnancy in a woman with history of missed IUD could be associated with transvesical migration of IUD and calculi formation.
2. Case Report
A 42-year-old woman para 3 with no history of abortion was referred to our hospital for investigation of recurrent lower abdominal pain, irritative lower urinary tract symptoms (LUTS) and strangury which had begun in the last 2 years. The patient had a history of IUD placement in the form of Copper T for contraception, 12 years earlier (10years before the onset of these symptoms). She had had no symptoms after insertion of the IUD. Follow-up examinations had been performed during the first year after placement of the IUD and the insertion had been successful. The woman in our case had been lost to medical follow up for the next 2 year (3 years from the IUD insertion); until she became pregnant. She had not removed the IUD, but routine prenatal sonography did not show any IUD in her endometrial cavity, and the patient delivered her baby by caesarean section at term on account of two previous caesarean sections without any complications. Noteworthy, she underwent simultaneous bilateral tubal ligation (TL) during her caesarean section surgery.
About 2 years before her referral to our hospital, the patient had developed recurrent lower abdominal pain, irritative lower urinary tract symptoms including dysuria, nocturia, increased frequency of urination and strangury. The patient had no history of macroscopic hematuria, but the urinalysis revealed numerous red blood cells and pyuria every time. She referred to different clinics and doctors with these symptoms in the past 2 years and was treated medically for urinary tract infection (UTI) repeatedly. Other laboratory tests were normal.
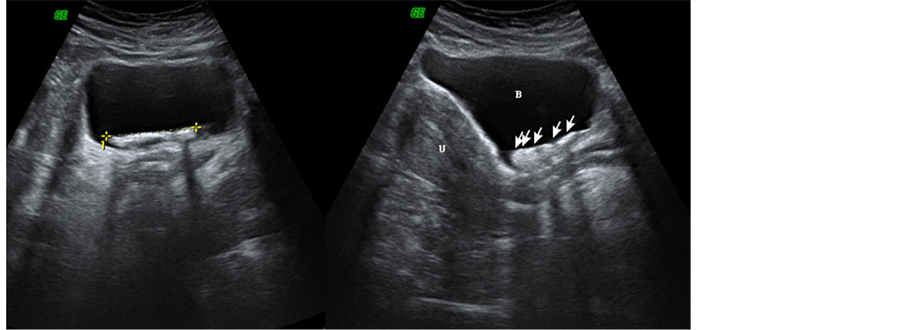
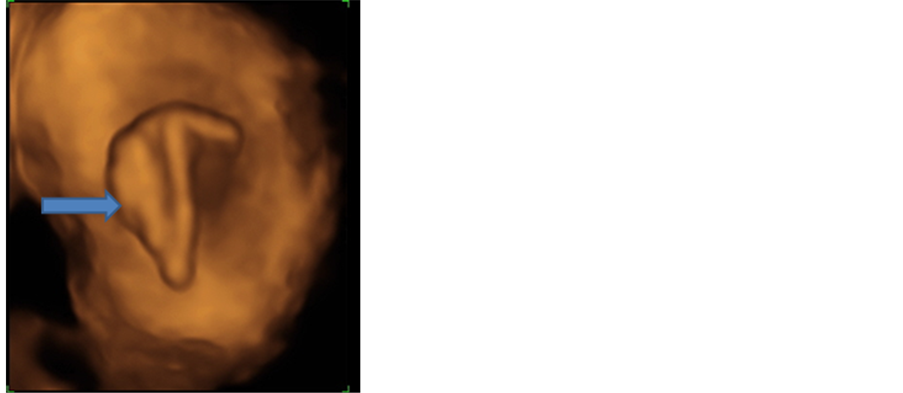
Then the patient was referred to our hospital for further evaluation. Initially a plain abdominopelvic radiography was performed for the patient and calcification of the IUD string and the IUD itself was visible in the pelvic region (Figure 1). Then transabdominal sonography of the pelvis was performed using an ultrasound scanner (GE, USA) equipped with a 3.5-MHz phased-array transducer. The sonographic images revealed a dense intra bladder stone like structure with metallic artifact consistent with a calculus IUD (Figure 2). Also, three dimensional ultrasound imaging showed intra bladder IUD and its calcified components (Figure 3).
The location of the IUD on sonography did not change when the patient was positioned differently. The patient was referred to Urologist and was hospitalized for a cystoscopic examination, which confirmed the sonographic findings of a calculus IUD implanted in the left anterior wall of the bladder. At first Holmium laser lithothripsy was performed then allowed removal of a copper-T IUD (Figure 4). After the procedure, the patient’s symptoms resolved completely on follow-up visits. Noteworthy, informed consent was obtained from the patient regarding publishing the case report and there was no objection.
Figure 1. Plain abdominopelvic radiography shows calcification of the IUD string (arrow), intrauterine IUD calcification is unusual and provokes intra bladder IUD migration.
Figure 2. Axial and sagittal trans abdominal ultrasound images shows dense intra bladder stone like lesion with metallic artifact (arrows), (U) uterus, (B) bladder.
Figure 3. Three dimensional ultrasound image, elegantly demonstrates intra bladder IUD and its calcified component (arrow).
Figure 4. Photograph shows removed IUD by transuretral cystoscopy procedure.
3. Discussion
IUD is one of the most safe, effective and reversible contraceptive method popular all over the world. Though rare, it can cause uterine perforation and migration to adjacent organs such as bowels, bladder, peritoneum, omentum, adnexa and iliac vein [8] [9] [10] [11] . The exact mechanism of uterine perforation is yet to be known. Probable factors that can influence the risk of uterine perforation are the time of insertion, insertion technique, congenital anomalies, infections, thinning of the uterine wall and hypoestrogenemia in the lactation and postpartum periods and anatomy of the cervix and uterus [12] [13] [14] . Perforation of the uterine by an IUD may basically occur via two mechanisms [15] . First, perforation at the time of placement primarily, called misplacement, which can present with bleeding, acute pelvic pain, or lost thread. IUD applicator’s experience and placement by specialists is an extremely important factor in prevention of misplacement, supported by many authors [16] [17] [18] [19] . Second, gradual and spontaneous perforation of the uterine after a long time since IUD insertion called migration, with late development of symptoms or being asymptomatic [20] . Forceful contractions of the uterine because of sexual stimulation or delivery, genital or bladder trauma, spontaneous irregular bladder contractions, bowel movements, and inflammatory effect of the IUD itself accompanied by the aforementioned risk factors, may be the mechanism of migration.
Kassab and Audra et al. collected 165 cases of uterine perforation in a literature review in 1999. Transvesical migration with or without calculi formation was seen in about 90 cases [21] . Although, the commonly asymptomatic nature of perforation supports the fact that the true incidence of perforation is most likely higher than what is reported in the literature.
Transvesical migration of the IUD is either within the bladder lumen or embedded in the bladder wall [22] . Most patients with intra bladder IUD are symptomatic with recurrent or persistent UTI and its symptoms, being the most common presentation [23] . Kart et al. reported a case of a 44 year old woman with transvesical migration of IUD who presented with dysuria and intermittent hematuria [19] . Gunbey et al. reported a case of a 46 year old woman with IUD partially embedded in the wall of the cervix and extending into the bladder lumen, presented with lower abdominal pain lasting for 2 years [24] . The patient in our case presented with recurrent LUTS, lower abdominal pain and UTIs. The coexistence of pregnancy and misplaced or migrated IUDs should be evaluated first by transabdominal or transvaginal sonography, especially in cases with amenorrhoea. Otherwise, initial investigation via plain abdominopelvic radiography may be of choice. In our case, the patient had a history of bilateral TL. Therefore, we initially performed a plain abdominopelvic radiography and calcified string of the IUD was visible in the pelvic region. Then sonographic images revealed a dense intra bladder stone like structure with metallic artifact consistent with a calculus IUD. Also, three dimensional ultrasound imaging showed intra bladder IUD and its calcified components. After pregnancy has been ruled out, the ideal and least expensive method for detecting a misplaced or migrated IUD is plain abdominopelvic radiography since all IUDs are radio-opaque [25] . Sonography is a useful method in the detection of patients with a suspected intra bladder IUD. IUDs misplaced in the abdominal cavity can be evaluated by CT scan for almost exact localization [5] . All transvesical migrated IUDs must be removed even if they are symptomless, to prevent bladder rupture and calculi formation [22] . Transvesical migrated IUDs could be removed by cytoscopic removal or by open suprapubic cystotomy [26] . Removal of the IUD and stone fragments with cystoscopic procedure after laser lithotripsy seems to be the least invasive and adequate treatment modality. In our case a cystoscopic examination confirmed the sonographic findings of a calculus IUD implanted in the left anterior wall of the bladder. Holmium laser lithothripsy was performed then allowed removal of a copper-T IUD leaving no complications. Open suprapubic cystotomy is performed at centres which do not have cystoscopic facilities and also intra bladder IUDs that could not be removed with cystoscope. We suggest that in our case the uterine perforation did not occur at the time of IUD placement, because the patient became pregnant around 3 years after the insertion of the IUD. Soft consistency of uterus in pregnancy, strong uterine contractions in delivery, and uterine contractions due to sexual intercourse, genital and bladder trauma, inflammatory effect of the IUD itself after pregnancy may be the cause of IUD migration in our case. Hence in similar cases with unexpected pregnancy, persistent or recurrent UTI and LUTS and intra bladder calculus should raise the suspicion for uterine perforation and transvesical IUD migration. Whenever suspected, evaluation could be done using plain abdominopelvic radiography. Nevertheless, CT scan could be used whenever sonography cannot detect the IUD and exact localization is required.
4. Conclusion
Follow up visits and examination immediately after IUD insertion and periodically, could prevent IUD misplacement, migration and other complications. Unexpected pregnancy, LUTS, persistent or recurrent UTI, intra bladder calculus should raise the suspicion for uterine perforation and transvesical IUD migration. Early sonography for evaluation of recurrent or persistent UTI is recommended. Removal of the IUD and stone fragments with cystoscopic procedure after laser lithotripsy seems to be the least invasive and adequate treatment modality.
Cite this paper
Azandaryani, A.R., Ghaderzadeh, P. and Farsangi, L.E. (2017) Intravesical Migration of Intrauterine Device and Calculi Formation 12 Years Post Missing: A Case Report. Case Reports in Clinical Medicine, 6, 24-30. http://dx.doi.org/10.4236/crcm.2017.61003
References
- 1. Mosher, W.D. and Pratt, W.F. (1990) Contraceptive Use in the United States, 1973-88. Patient Education and Counseling, 16, 163-172.
https://doi.org/10.1016/0738-3991(90)90092-Y - 2. Oruc, S., Vatansever, H.S., Karaer, O., Eskicioglu, F. and Narlikuyu, B. (2005) Changes in Distribution Patterns of Integrins in Endometrium in Copper T380 Intrauterine Device Users. Acta Histochemica, 107, 95-103.
https://doi.org/10.1016/j.acthis.2005.01.001 - 3. Tuncay, Y.A., Tuncay, E., Guzin, K., Ozturk, D., Omurcan, C. and Yucel, N. (2004) Transuterine Migration as a Complication of Intrauterine Contraceptive Devices: Six Case Reports. The European Journal of Contraception & Reproductive Health Care: The Official Journal of the European Society of Contraception, 9, 194-200.
https://doi.org/10.1080/13625180400007165 - 4. el-Diasty, T.A., Shokeir, A.A., el-Gharib, M.S., Sherif, L.S. and Shamaa, M.A. (1993) Bladder Stone: A Complication of Intravesical Migration of Lippes Loop. Scandinavian Journal of Urology and Nephrology, 27, 279-280.
https://doi.org/10.3109/00365599309181267 - 5. Sinha, M., Gupta, R. and Tiwari, A. (2013) Minimally Invasive Surgical Approach to Retrieve Migrated Intrauterine Contraceptive Device. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 2, 147-151.
- 6. Nitke, S., Rabinerson, D., Dekel, A., Sheiner, E., Kaplan, B. and Hackmon, R. (2004) Lost levonorgestrel IUD: Diagnosis and Therapy. Contraception, 69, 289-293.
https://doi.org/10.1016/j.contraception.2003.11.017 - 7. Heinberg, E.M., McCoy, T.W. and Pasic, R. (2008) The Perforated Intrauterine Device: Endoscopic Retrieval. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 12, 97-100.
- 8. Ozcelik, B., Serin, I.S., Basbug, M., Aygen, E. and Ekmekcioglu, O. (2003) Differential Diagnosis of Intra-Uterine Device Migrating to Bladder Using Radiographic Image of Calculus Formation and Review of Literature. European Journal of Obstetrics, Gynecology, and Reproductive Biology, 108, 94-96.
https://doi.org/10.1016/S0301-2115(02)00240-3 - 9. Schoenfeld, A., Pardo, J., Engelstein, D., Ovadia, J. and Servadio, C. (1991) Bladder Perforation by an Intrauterine Device. Journal of Clinical Ultrasound: JCU, 19, 175-177. https://doi.org/10.1002/jcu.1870190310
- 10. McNamara, M., Kennan, N. and Buckley, A.R. (1985) Copper-7 Perforation of the Uterus and Urinary Bladder with Calculus Formation—Sonographic Demonstration. The British Journal of Radiology, 58, 558-559.
https://doi.org/10.1259/0007-1285-58-690-558 - 11. Guvel, S., Tekin, M.I., Kilinc, F., Peskircioglu, L. and Ozkardes, H. (2001) Bladder Stones around a Migrated and Missed Intrauterine Contraceptive Device. International Journal of Urology, 8, 78-79.
https://doi.org/10.1046/j.1442-2042.2001.00249.x - 12. Farmer, M. and Webb, A. (2003) Intrauterine Device Insertion-Related Complications: Can They Be Predicted? The Journal of Family Planning and Reproductive Health Care, 29, 227-231.
https://doi.org/10.1783/147118903101197854 - 13. Behtash, N., Akhavan, S. and Mokhtar, S. (2010) Pelvic Mass Due to Transmigrated IUD. Acta medica Iranica, 48, 125-126.
- 14. Boortz, H.E., Margolis, D.J., Ragavendra, N., Patel, M.K. and Kadell, B.M. (2012) Migration of Intrauterine Devices: Radiologic Findings and Implications for Patient Care. Radiographics, 32, 335-352.
https://doi.org/10.1148/rg.322115068 - 15. Zakin, D., Stern, W.Z. and Rosenblatt, R. (1981) Complete and Partial Uterine Perforation and Embedding Following Insertion of Intrauterine Devices. II. Diagnostic Methods, Prevention, and Management. Obstetrical & Gynecological Survey, 36, 401-417.
https://doi.org/10.1097/00006254-198108000-00001 - 16. Atakan, R.H., Kaplan, M. and Ertrk, E. (2002) Intravesical Migration of Intrauterine Device Resulting in Stone Formation. Urology, 60, 911.
https://doi.org/10.1016/S0090-4295(02)01883-6 - 17. Hoscan, M.B., Kosar, A., Gumustas, U. and Guney, M. (2006) Intravesical Migration of Intrauterine Device Resulting in Pregnancy. International Journal of Urology, 13, 301-302.
https://doi.org/10.1111/j.1442-2042.2006.01291.x - 18. Guner, B., Arikan, O., Atis, G., Canat, L. and Caskurlu, T. (2013) Intravesical Migration of an Intrauterine Device. Urology Journal, 10, 818-820.
- 19. Kart, M., Gulecen, T., Ustuner, M., Ciftci, S., Yavuz, U. and Ozkurkcugil, C. (2015) Intravesical Migration of Missed Intrauterine Device Associated with Stone Formation: A Case Report and Review of the Literature. Case Reports in Urology, 2015, Article ID: 581697.
https://doi.org/10.1155/2015/581697 - 20. Eke, N. and Okpani, A.O. (2003) Extrauterine Translocated Contraceptive Device: A Presentation of Five Cases and Revisit of the Enigmatic Issues of Iatrogenic Perforation and Migration. African Journal of Reproductive Health, 7, 117-123.
https://doi.org/10.2307/3583296 - 21. Kassab, B. and Audra, P. (1999) The Migrating Intrauterine Device. Case Report and Review of the Literature. Contraception, Fertilite, Sexualite, 27, 696-700.
- 22. Kandirali, E., Topcuoglu, M.A., Semerciöz, A. and Metin, A. (2008) Double Intrauterine Device: Presented with Protruding Urethral Stone. Marmara Medical Journal, 21, 61-63.
- 23. Dietrick, D.D., Issa, M.M., Kabalin, J.N. and Bassett, J.B. (1992) Intravesical Migration of Intrauterine Device. The Journal of Urology, 147, 132-134.
- 24. Gunbey, H.P., Sayit, A.T., Idilman, I.S. and Aksoy, O. (2014) Migration of Intrauterine Devices with Radiological Findings: Report on Two Cases. BMJ Case Reports 2014.
- 25. Bozkurt, M., Yumru, A.E., Coskun, E.I. and Ondes, B. (2011) Laparoscopic Management of a Translocated Intrauterine Device Embedded in the Gastric Serosa. JPMA The Journal of the Pakistan Medical Association, 61, 1020-1022.
- 26. Hick, E.J., Hernandez, J., Yordan, R., Morey, A.F., Aviles, R. and Garcia, C.R. (2004) Bladder Calculus Resulting from the Migration of an Intrauterine Contraceptive Device. The Journal of Urology, 172, 1903.
https://doi.org/10.1097/01.ju.0000142135.94531.bb