Case Reports in Clinical Medicine
Vol.1 No.2(2012), Article ID:25509,3 pages DOI:10.4236/crcm.2012.12003
Progressive pre-operative pneumoperitoneum is not necessary for large inguinoscrotal hernia repair: Report of a case
![]()
Department of Surgery, Northampton General Hospital, Northampton, UK; *Corresponding Author: ugoihedioha@hotmail.com
Received 24 October 2012; revised 27 November 2012; accepted 8 December 2012
Keywords: Large Inguinoscrotal Hernia; Pneumoperitoneum
ABSTRACT
Huge inguinoscrotal hernias are a challenging operation. The technical aspects of the procedure can be very difficult and the recovery may be complicated by ventilatory problems. Progressive preoperative pneumoperitoneum (PPP) is a method which has been used for many years to reduce both intra and postoperative complications. However, it is associated with a prolonged preoperative hospital stay which is expensive and often stressful to patients. We report a case of a morbidly obese patient with a huge inguinoscrotal hernia. PPP was not implemented. The operation was uneventful and he was discharged 8 days later with no major postoperative complications. This case therefore questions the necessity of PPP for huge inguinoscrotal hernias.
1. INTRODUCTION
Giant inguinoscrotal hernias are very rare in the developed world [1]. However, they do not cease to exist. Repairing these hernias is challenging due to the technical difficulties associated with their size and because of the high number of serious co morbidities patients with this kind of hernia usually have [1,2]. One of the greatest challenges of repairing giant inguinoscrotal hernias is the issue of reducing the herniating viscera back to the contracted peritoneal cavity. A commonly used method to overcome this is the progressive expansion of the abdominal wall cavity by creating a preoperative pneumoperitoneum over a number of days. This is a technique that has many advocates [1-4] but its effectiveness is questionable [1]. The aim of this case report is to show that a giant inguinoscrotal hernia can be repaired without the use of progressive preoperative pneumoperitoneum preparation (PPP).
2. CASE REPORT
A 41 year old gentleman who weighed 181 kg and had a BMI of 56 (Table 1) first presented to our clinic 3 years ago with a 17 year history of a huge inguinoscrotal swelling. This hanged between his knees and prevented him from driving. Physical examination revealed a massive left inguinoscrotal hernia.
He had previously been refused surgery due to his weight and social history (Smoked 40 cigarettes a day, consumed up to 2 bottles of vodka in an evening, and occasionally used recreational drugs such as cocaine).
We advised him to lose weight and reduce his smoking before considering him for surgery. He was referred to a clinical psychologist and a dietician.
He had lost 40 kg in weight in 6 months, reduced his smoking to 10 cigarettes per day, stopped using recreational drugs and reduced his alcohol intake to a minimum.
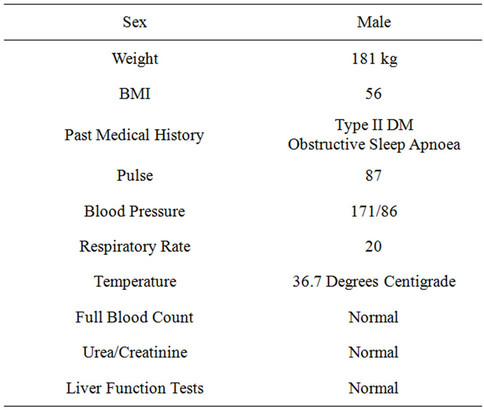
Table 1. Patient characteristics.
Other co-morbidities included type II diabetes mellitus and obstructive sleep apnoea.
The hernia was approached using a left groin incision. The indirect hernia contained sliding sigmoid, omentum and 4 litres of serous fluid. The contents of the sac were aspirated and reduced. The left testicle was sacrificed. We attempted to dissect the pre peritoneal plane but this was distorted so it was abandoned. As an alternative we plicated transversalis fascia with 1.0 vicryl to hold the hernia. We then proceeded to a “Maloney Darn” repair with 1 nylon to re-inforce the posterior wall and a 20 × 18 dynamesh sutured as “on lay” with 2/0 prolene. Following haemostasis and lavage a 30F silicon drain and a 19F Blakes drain were inserted. Scarpa’s fascia was closed with vicryl and clips for the skin.
Postoperatively, he was managed in the high dependency unit for 48 hours. He developed an ileus on the ward which was successfully managed conservatively. He was discharged home on day 8.
During his 6 week clinic follow up, the scrotal swelling was reducing in size and his quality of life had greatly improved.
3. DISCUSSION
Inguinoscrotal hernias are defined as giant when they extend below the midpoint of the inner thigh in the standing position [1,3]. These hernias are debilitating for the patient, affecting their mobility but also often their psychological status, often limiting them to their home. Even though their repair carries high morbidity risk, surgery is the only option [1]. Their repair is challenging because of the increased co-morbidities these patients carry and because of the technical aspects of the procedure. Since these hernias have been there for a long time abdominal viscera has often migrated into the herniating cavity and formed adhesions [5]. The peritoneal cavity, emptied from its normal contents, can contract, decrease in size and become unable to now accommodate the herniated abdominal viscera. This challenge is often referred to as “loss of right of domain” of the herniating viscera [5-7]. Abrupt reduction of the herniating viscera could be devastating because of the sudden increase in intra-abdominal and intra-thoracic pressure, which could impair diaphragmatic motion, reduce venous return and lead to abdominal compartment syndrome [5,8,9].
One of the techniques used to overcome this challenge is progressive preoperative pneumoperitoneum (PPP) preparation. This technique was first described by Goni Moreno in the 1940s [10,11]. It is usually done by the insertion of an intra-peritoneal catheter and the injection of air daily for a period of 9 to 15 days [4,12]. By progressively adding air in the peritoneal cavity the cavity is enlarged and can more easily accommodate the herniating contents.
PPP has many advocates but its effectiveness is questionable [1,13] and it is now used in a lesser degree [7]. The advantages are obvious, by expanding the abdominal cavity the lost space is recreated and the herniated contents can easily return to their natural space during surgery. The increased capacity of the abdominal cavity means that the intra-abdominal pressure does not rise as much once the herniating contents are reduced. This results in improved diaphragmatic function and better venous return which in turn decreases the risk of post operative ventilatory and haemodynamic complications [5]. Furthermore, there are reports that PPP performs a pneumatic lysis of intestinal adhesions [14]. One case report even describes during maintained pneumoperitoneum the spontaneous dissection of the gallbladder from the liver bed [14]. Reduced adhesions make the technical aspects of the procedure easier.
By far the greatest disadvantage of PPP is the need for prolonged preoperative hospitalisation which could be up to 18 days [15]. This, apart from being expensive, is often stressful to the patient. During PPP there is always a risk that the insuflated air enters the herniating cavity instead, only resulting in an increase in size of the herniating sac rather than the abdominal cavity [8,16]. This can increase the difficulty of the procedure and also lead to stretching or even ulceration of the scrotal skin. PPP also carries a risk of infection as associated with any procedure. Finally, in the literature there has been a case of neck and chest wall surgical emphysema induced by PPP [5]. However, this did not cause any problems and PPP was not interrupted.
In our case we demonstrated that PPP is not always necessary. We reduced a huge inguinoscrotal hernia back into the abdominal cavity without the need to preoperatively increase its capacity. It has been suggested that PPP would be particularly useful in obese patients [13]. This is because of the increased risk of postoperative ventilator complications associated with an already high intra abdominal and intra thoracic pressure secondary to obesity. However, our patient was extremely obese and a chronic smoker, yet with adequate pre operative preparation we avoided any respiratory complications. To minimise postoperative complications a HDU bed was prearranged. He was extubated normally in theatre and he maintained reasonable saturations with minimal oxygen supplementation throughout his recovery. He also remained haemodynamically stable throughout his recovery and the only problem he encountered was a post operative ileus which spontaneously resolved in two days. Whether this could have been avoided with the use of PPP is unknown but seems unlikely. Either way, the increased cost and stress of preoperative hospitalisation would by far outweigh the setback caused by this patient’s ileus.
PPP has been used for huge inguinal hernias for over 60 years [5]. It increases the capacity of the abdominal cavity making the procedure less difficult technically and decreasing the risk of post operative cardiorespiratory complications. However its use is declining as it prolongs hospital stay and its effectiveness is doubtful. In this report we demonstrated a case of a huge inguinoscrotal hernia repair performed on a morbidly obese high risk patient, which was done without the use of PPP. Our patient had a quick and uneventful recovery. Even though our patients’ weight and comorbidities would make him an ideal candidate for PPP, in this case it was not necessary. This poses the question, is pneumoperitoneum really necessary?
REFERENCES
- Vasiliadis, K., Knaebel, H.P., Djakovic, N., Nyarangi-Dix, J., Schmidt, J. and Büchler, M. (2010) Challenging surgical management of a giant inguinoscrotal hernia: Report of a case. Surgery Today, 40, 684-687. doi:10.1007/s00595-009-4125-3
- Serpell, J.W., Polglase, A.L. and Anstee, E.J. (1988) Giant inguinal hernia. Australian and New Zealand Journal of Surgery, 58, 831-834. doi:10.1111/j.1445-2197.1988.tb00988.x
- Hodgkinson, D.J. and McIlrath, D.C. (1980) Scrotal reconstruction for giant inguinal hernias. Surgical Clinics of North America, 64, 307-313.
- Edward, E.M. and Merril, T.D. (1989) Pneumoperitoneum in giant hernia. In: Nyhus, L.M. and Condon, R.E., Eds., Hernia, 3rd Edition, Lippincott, Philadelphia, 36, 521-530.
- Mayagoitia, J.C., Suárez, D., Arenas, J.C. and Díaz de León, V. (2006) Preoperative progressive pneumoperitoneum in patients with abdominal-wall hernias. Hernia, 10, 213-217. doi:10.1007/s10029-005-0040-8
- Forrest, J. (1979) Repair of massive inguinal hernia. Archives of Surgery, 114, 1087-1088. doi:10.1001/archsurg.1979.01370330109021
- El Saadi, A.S., Al Wadan, A.H. and Hamerna, S. (2005) Approach to a giant inguinoscrotal hernia. Hernia, 9, 277-279. doi:10.1007/s10029-004-0291-9
- Kyle, S.M., Lovie, M.J. and Dowle, C.S. (1990) Massive inguinal hernia. British Journal of Hospital Medicine, 43, 383-384.
- Barst, H.H. (1972) Pneumoperitoneum as an aid in the surgical treatment of giant herniae. British Journal of Surgery, 59, 360-364. doi:10.1002/bjs.1800590507
- Goni Moreno, I.G. (1978) The rational treatment of hernias and voluminous chronic eventrations: Preparation with progressive pneumoperitoneum. In: Nyhus, L.M. and Condon, R.E., Eds., Hernia, 2nd Edition, Lippincott, Philadelphia, 536-560.
- Goni Moreno, I. (1947) Chronic eventration and large hernias: Preoperative treatment by progressive pneumoperitoneum-original procedure. Surgery, 22, 945-953.
- Raynor, R.W. and Del Guercio, L.R. (1989) The place for pneumoperitoneum in the repair of massive hernia. World Journal of Surgery, 13, 581-585. doi:10.1007/BF01658874
- Kovachev, L.S., Paul, A.P., Chowdhary, P., Choudhary, P. and Filipov, E.T. (2010) Regarding extremely large inguinal hernias with a contribution of two cases. Hernia, 14, 193-197. doi:10.1007/s10029-009-0517-y
- Herszage, L. (2003) Abordaje de las eventraciones de pared. In: Mayagoitia, J.C., Ed., Hernias de la Pared Abdominal. Tratamiento Actual, McGraw-Hill, Mexico, 201-212.
- Beitler, J.C., Gomes, S.M., Coelho, A.C. and Manso, J.E. (2009) Complex inguinal hernia repairs. Hernia, 13, 61-66. doi:10.1007/s10029-008-0432-7
- Merrett, N.D., Waterworth, M.W. and Green, M.F. (1994) Repair of giant inguinoscrotal inguinal hernia using marlex mesh and scrotal skin flaps. Australian and New Zealand Journal of Surgery, 64, 380-383. doi:10.1111/j.1445-2197.1994.tb02231.x

