Case Reports in Clinical Medicine
Vol.05 No.03(2016), Article ID:64178,4 pages
10.4236/crcm.2016.53012
Peripheral Central Venous Catheter Induced Supraventricular Tachycardia in a Patient of Acute Lymphoblastic Leukemia
Rangreze Imran1*, Asiri Abdulrahman2, Al-Hanash Ali2, Shehla Shafi Khan3
1Department of Internal Medicine, KKU, Abha, KSA
2Department of Medicine, Aseer Central Hospital, Abha, KSA
3Department of Family Medicine, Armed Force Hospital, Khemis Mushayt, KSA

Copyright © 2016 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 9 January 2016; accepted 29 February 2016; published 3 March 2016
ABSTRACT
Central venous catheters (CVCs) are used in intensive care units (and, increasingly, in other locations) to administer intravenous fluids and blood products, drugs, parenteral nutrition, and to monitor haemodynamic status. The risk of complication during the insertion or exchange of central venous catheters has been well documented. The majority of complications involve mechanical problems, although rarely it may induce arrhythmias as well [1] . Herein we present a case of peripheral central venous catheter induced supraventricular tachycardia in a young patient of acute lymphoblastic leukemia.
Keywords:
Central Venous Catheter (CVC), Supraventricular Tachycardia, Acute Lymphoblastic Lymphoma

1. Introduction
Insertion of a central venous catheter (CVC) in a human was first reported by Werner Forssman, a surgical intern, who described canalizing his own right atrium via the cephalic vein in 1929. However, insertion of a CVC using the Seldinger technique revolutionized medicine by allowing the central venous system to be accessed safely and easily. Central venous catheters are now commonly used among critically ill and leukemic patients for administering/guaging iv fluids and delivering medicines.
Numerous complications like ventricular dysrhythmias and bundle branch block are well recognized complications during central venous access procedures, as was the case with our patient. Periprocedural arrhythmias are universally the result of guidewire or catheter placement into the right heart and limiting the depth of guidewire insertion to less than 16 cm avoids this complication [2] . Catheter migration up to 3 cm is common with patient movement and repositioning may cause delayed symptoms.
2. Case Summary
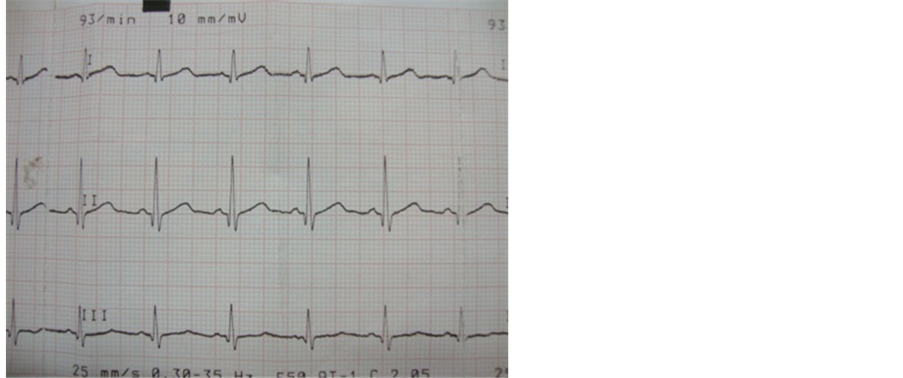
A 17-year boy was admitted with symptomatic anemia in our department. Examination revealed pallor, generalized lymphadenopathy and hepato-splenomegaly. He was investigated and diagnosed to have acute lymphoblastic lymphoma. His base line electrocardiogram (ECG) and echocardiography were normal (Figure 1). He was planned for chemotherapy and a peripherally inserted central venous catheter (PICC) was put through left ante-cubital vein. Procedure was uneventful and peripherally inserted central venous catheter position was confirmed by chest radiography (Figure 2).
After 6 hours, he complained of palpitations and ECG revealed supraventricular tachycardia (Figure 3). He was reverted with intravenous (i.v.) adenosine 6 mgs and oral diltiazem. He again developed supraventricular tachycardia next morning which was reverted back to normal sinus rhythm with i.v. diltiazem. It was followed by another episode few hours later. Patient was managed with 15 mg i.v. diltiazem this time and peripherally inserted central venous catheter was withdrawn by 5cms. Patient was symptom free thereafter and the repeat ECG, echocardiography and electrophysiological studies (EPS) were normal.
Figure 1. Normal ECG.
Figure 2. SVT induced after PICC placement.
Figure 3. CXR showing PICC in place.
Presently patient has completed Induction phases and intensification phase of chemotherapy and is in clinical and bone marrow remission. In addition, he is on prophylactic cranial irradiation.
3. Discussion
Paroxysmal supraventricular tachycardia (PSVT) is a common arrhythmia occurring with an incidence of 2.5 per 1000 adults [3] . PSVT in the absence of structural heart disease can present at any age but most commonly first presents between ages 12 and 30. Central venous catheters extending into cardiac chambers can provoke premature atrial and ventricular complexes, which have been reported to initiate SVT [4] . After blind placement of a CVC, an intracardial position is found in up to 50% of the cases [5] [6] .
Arrhythmias occur commonly during CVC insertion. In a recent study, atrial arrhythmias and ventricular ectopic occurred with a frequency of 41% and 25%, respectively [7] .
Vagal maneuvers should be attempted, and if the SVT cannot be terminated, then intravenous adenosine or calcium channel blockers should be administered. Adenosine is a shortacting drug that blocks AV node conduction; it terminates 90% of tachycardias. Synchronized cardioversion can also be used immediately in patients who develop hypotension, pulmonary edema, or ischemic chest pain [8] . In our patient, the SVT responded to the administration of adenosine and repositioning of guidewire.
CVCs placement procedure can induce dysrhythmias. So various measures must be taken like increased operator experience, fewer insertion attempts, ultrasound guided procedure and limiting the depth of guidewire insertion to less than 16 cm, to avoid mechanical or hemodynamic complications.
4. Conclusions
Although cardiac arrhythmia has been acknowledged as a possible complication, over-insertion of the guidewire, causing direct stimulation to the right side of the heart, has been postulated to be the causative factor. Hence immediate retraction of the guidewire or catherter should be done to abort the episode of dysarrythmia [7] .
We obtained consent from the patient as well as his parents to publish this case. In addition, hospital ethical committee was well aware of before writing this case report.
In addition, we tried our best to completely anonymise our patient by not giving any specific identifying features or details.
Cite this paper
Rangreze Imran,Asiri Abdulrahman,Al-Hanash Ali,Shehla Shafi Khan, (2016) Peripheral Central Venous Catheter Induced Supraventricular Tachycardia in a Patient of Acute Lymphoblastic Leukemia. Case Reports in Clinical Medicine,05,67-70. doi: 10.4236/crcm.2016.53012
References
- 1. Yavascan, O., Mir, S. and Tekguc, H. (2009) Supraventricular Tachycardia Following Insertion of a Central Venous Catheter. Saudi Journal of Kidney Diseases and Transplantation, 20, 1061-1064.
- 2. Tripathi, M., Dubey, P.K. and Ambesh, S.P. (2005) Direction of the J-Tip of the Guidewire, in Seldinger Technique, Is a Significant Factor in Misplacement of Subclavian Vein Catheter: A Randomized, Controlled Study. Anesthesia & Analgesia, 100, 21.
http://dx.doi.org/10.1213/01.ANE.0000139349.40278.77 - 3. Verdino, R.J., Pacifico, D.S. and Tracy, C.M. (1996) Supraventricular Tachycardia Precipitated by a Peripherally Inserted Central Catheter. Journal of Electrocardiology, 29, 69-72.
http://dx.doi.org/10.1016/S0022-0736(96)80116-6 - 4. McGee, W.T., Ackerman, B.L., Rouben, L.R., Prasad, V.M., Bandi, V. and Mallory, D.L. (1993) Accurate Placement of Central Venous Catheters: A Prospective, Randomized, Multicenter Trial. Critical Care Medicine, 21, 1118-1123.
http://dx.doi.org/10.1097/00003246-199308000-00008 - 5. Lumb, P.D. (1993) Complications of Central Venous Catheters. Critical Care Medicine, 21, 1105-1106.
http://dx.doi.org/10.1097/00003246-199308000-00001 - 6. Stuart, R.K., Shikora, S.A., Akerman, P., et al. (1990) Incidence of Arrhythmia with Central Venous Catheter Insertion and Exchange. Journal of Parenteral and Enteral Nutrition, 14, 152-155.
http://dx.doi.org/10.1177/0148607190014002152 - 7. Pawlik, M.T., Kutz, N., Keyl, C., Lemberger, P. and Hansen, E. (2004) Central Venous Catheter Placement: Comparison of the Intravascular Guidewire and the Fluid Column Electrocardiograms. European Journal of Anaesthesiology, 21, 594-599.
http://dx.doi.org/10.1097/00003643-200408000-00002 - 8. Trohman, R.G. (2000) Supraventricular Tachycardia: Implications for the Intensivist. Critical Care Medicine, 28, 129-135.
http://dx.doi.org/10.1097/00003246-200010001-00004
NOTES
*Corresponding author.