Utility of nelson’s modified card sorting test in patients with alzheimer’s disease or vascular dementia ()
1. INTRODUCTION
According to the Department of Statistics, Ministry of the Interior (MOI), December 2010, the aging index stood at 39.4 percent in 1999 but shot up to 65.05 in 2009 as the impact of Taiwan’s declining birth rate began to bite. Even though it is lower than in 2004 average of 88.24% in all developing countries. The MOI report shows that Taiwan’s elderly population was close to 2.5 million, or 1-to-10 as of the end of last year. The over-65 population accounts for 10.63 percent of the country’s 23.12 million people [1]. This increasing population of the elderly has led to the development of physical and mental problems for both patients and family members. Su’s report showed that a high prevalence in dementia (45.7% - 50.4%) and depression (25%) for long-term institutionalized elderly leprosy patients in Taiwan [2]. One study has shown that the percentage of elderly dementia patients has increased from 1.9% to 4.4% in Taiwan [3], where 91.5% of dementia patients are taken care of by their family members, and only a few dementia cases are under the care of a health facility. Chen’s (2009) research identified that dementia is a hidden health issue because of its underestimation in the elderly population in Taiwan and many other counties [4].
Chang’s (2012) research revealed that feeding difficulty has a higher prevalence in elderly patients with dementia in Taiwan [5]. Dementia is characterized by significant impairments in multiple cognitive domains, functioning, and behavior, and places a tremendous burden not only on individuals, but also on society.
Dementia refers to a syndrome of acquired cognitive impairment that is caused by cerebral dysfunction and interferes with social or occupational functioning [6]. The DSM-IV [7] further defines dementia as a disorder characterized by disturbances of memory and at least one additional cognitive function (e.g., language, praxis, gnosis, or executive function). The cognitive deficits present in dementia must represent a significant decline from premorbid functioning and must result in significant declines in activities of daily living (ADLs). Various dementias are associated with a wide range of neuropathological features, and it is generally acknowledged that patients with different types of dementias present with varied cognitive, behavioral, and affective disturbances [8].
Neuropsychometric assessment seems to be the best method to screen individuals in most developing countries [9]. Executive dysfunction may be an early sign of vascular cognitive impairment and may have considerable impact on the functional outcomes of patients with stroke [10]. Proposed executive processes include functions such as planning, monitoring, energizing, switching and inhibition [11]. The WCST is commonly used in neuropsychological assessment as a measure of executive function [12]. The WCST is particularly sensitive to frontal-lobe lesions [13] and is a well-validated neuropsychological tool for the assessment of executive functioning [14].
AD is the major focus for dementia cases in the Wisconsin sorting card test, which is used to identify problems in decision making, problem solving, conception structure and cognitive ability [15]. These are all closely related to the functioning of the frontal lobe. Studies have also shown that the WSCT shows a distinctive difference for cases of dementia, depression, and Parkinson’s disease, and the control group. However elderly persons sometimes find the WSCT too abstract, imperious, and time consuming, which decreases their motivation to complete the task, hence, Nelson developed a modified way to do the WSCT which increases the motivation to complete the task and increases the patient’s understanding of the method of the test via decreasing the number of cards from 128 to 24, and there by decreasing the time taken to complete the test [16]. The Modified Card Sorting Test [16], a simplification of the Wisconsin Card Sorting Test, consists of two sets of only 24 cards. MCST scoring is mainly based on the number of categories completed and the number of errors, classified as “perseverative” and “non-perseverative”. The capability to categorize and avoid perseveration is of greater clinical significance, and on this basis the MCST has proved useful in studying frontal lobe lesions or dysfunctions in adults [17]. The aim of this study was to explore the relation between Alzheimer’s disease/vascular dementia and the Nelson’s Modified Card Sorting Test.
2. METHODS
2.1. Participants
This study was reviewed and approved by the Institutional Review Board (IRB) of Chung Hwa University of Medical and Technology. Subjects selected for this study were elderly patients who are 65 years old and over. A total of 210 patients were evaluated for dementia at the Young-Kang Veteran Hospital between September 2009 and May 2011. From the 210 patients we then selected those with a clinical diagnosis and we used the minimental state examination (MMSE), the clinical dementia rating (CDR), the geriatric depression scale (GDS), DSMIV criteria of Alzheimer’s type, Hachinski’s ischemic scale and CT-scan of the brain as a standard to diagnose AD and VD. Finally we are collect of possible AD (N = 64) and VD (N = 40), yielding a total of 178 patients in the study. Patients excluded from this selection of dementia types had either “mixed” dementia, traumatic brain injury, depression, developmental disability, mental retardation, Down’s syndrome, hearing loss, or another diagnosis. The results were that 64 out of the 178 had AD, 40 had vascular dementia and 74 were in the control group. We used the Nelson’s MCST and subject’s age and qualification to judge the relationship between dementia and result of MCST.
2.2. Assessment
A comprehensive history, neurological examination, and mental status examination were performed by experienced geriatric psychiatrists. This assessment included a complete evaluation of any cognitive symptoms, using input from the patient’s family members and caregiver. Brain imaging (MRI or CT) and laboratory assessments (including chemistries, electrolytes, complete blood count, liver tests, thyroid tests, serum B12, serum folate, sedimentation rate, urinalysis, and chest X-ray) were performed.
The subjects in this study were 65 years old and over, and went through a series clinical and neurological examinations. Diagnoses were made by using the information obtained above, along with information from family members, other caregivers, and primary care physicians, to ensure reliability. Patients were also rated on the following standardized scales:
1) The mini-mental state examination (MMSE) or Folstein test, a brief 30-point questionnaire test that is used to assess cognition. It is commonly used in medicine to screen for dementia. In the time span of about 10 minutes, it samples various functions, including arithmetic, memory and orientation. It was introduced by Folstein et al. in 1975 [18], and is widely used with small modifications. The MMSE is a copyrighted test of Psychological Assessment Resources, Inc. The complete Folstein is available in the appendix of the original publication. Any score over 24 (out of 30) is effectively normal. The normal value is also corrected for degree of schooling and age [19]. Low to very low scores correlate closely with the presence of dementia, although other mental disorders can also lead to abnormal findings on MMSE testing. The presence of purely physical problems can also interfere with interpretation if not properly noted; for example, a patient may be physically unable to hear or read instructions properly, or may have a motor deficit that affects writing and drawing skills.
2) The Clinical Dementia Rating (CDR), a numeric scale used to quantify the severity of symptoms of dementia (i.e., its “stage”). Using a structured-interview protocol developed by John C. Morris and colleagues at Washington University School of Medicine, a qualified health professional assesses a patient’s cognitive and functional performance in six areas: memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care. Scores in each of these are combined to obtain a composite score ranging from 0 through 3 [20]. CDR is credited with being able to discern very mild impairments, but its weaknesses include the amount of time it takes to administer, its ultimate reliance on subjective assessment, and relative inability to capture changes over time.
3) The Geriatric Depression Scale (GDS), a 30-item self-report assessment used to identify depression in the elderly. The GDS questions are answered “yes” or “no”, instead of a five-category response set. This simplicity enables the scale to be used with ill or moderately cognitively impaired individuals. The scale is commonly used as a routine part of a comprehensive geriatric assessment. One point is assigned to each answer and the cumulative score is rated on a scoring grid. The grid sets a range of 0 - 9 as “normal”, 10 - 19 as “mildly depressed”, and 20 - 30 as “severely depressed”. A diagnosis of clinical depression should not be based on GDS results alone. Although the test has well-established reliability and validity evaluated against other diagnostic criteria, responses should be considered along with results from a comprehensive diagnostic work-up [21].
4) Hachinski Ischemic Scale. In the 1970s, the widespread understanding that cerebrovascular disease was preventable prompted the development of the Hachinski Ischemic Scale to help differentiate multi-infarct dementia from degenerative dementia. Since then, this scale has been validated for use in the differentiation of pure Alzheimer’s disease from multi-infarct dementia, although it is not capable of distinguishing between the multi-infarct state and mixed dementias. From a practical viewpoint, it is the identification of a potentially treatable vascular component that is important. Hence, the important distinction is between pure Alzheimer’s disease and multiinfarct or mixed dementia [22]. In this scale, scores of 7 or more suggest a vascular cause of dementia; scores of 4 or less suggest primarily a degenerative process.
5) Nelson’s MCST: Nelson developed a considerably shorter alternative version of the test. The MCST differs from the WCST in several ways [16].
Firstly, the 128 response cards have been reduced to 48, consisting pairs of identical packs of 24 response cards. For the set of 4 stimulus cards, each individual response will only apply to 1 stimulus card. It was claimed by Lineweaver et al. that the examiner’s feedback are able to provide the respondent more defined information due to the change, therefore the sorting strategy for the participant can be easily claimed that the change allows the examiner’s feedback to provide unambiguous information to the respondent, and the participant’s sorting strategy can be easily deduced [23].
Secondly, the MCST allows the participants to begin with the category of their own choice and allocate the other 2 categories in a self-selected order.
Thirdly, instead of 10 in the original version, the number of consecutive correct responses necessary for completing the category is reduced to 6 correct responses.
Fourthly, following 6 continuous correct answers, the participant is informed to form a new sorting principle and change the rule. As the average cognitive performance and attention capacity declines with age [23,24], the simple and clear instruction of the survey with the shorten length allows the elderly to complete without any difficulties. The elderly candidates are more likely perform to their true potential by using the modified version of MCST, as there are more flexibility and lesser ambiguity and confusion of the test [25].
The administration procedure and instructions given to the participants were as follows [26]:
“Here are 4 key cards, I want you to pair each of the cards in the deck [indicating the response cards] to one of these 4 key cards [indicating each of the 4 stimulus cards], by following certain rules. However, I am not allowed to tell you what the rules are. You have to deduce them by trying different rules. I will tell you whether your response is correct or not after each pair. You are only allowed to take one top card from the deck at all time, and place it below the key card that you think it matches. If you are told your match is incorrect, just leave this match, and try to match the next card. Now, let’s start.” As the participants are all ethnically Chinese, the instructions used were translated into Mandarin throughout the administration procedure and therefore the procedure was conducted in Mandarin.
Data analyses were performed with Statistical Package for Social Science version 15 for Windows (SPSS, Chicago Illinois, USA). ANOVA and Chi-square were used to estimate three different groups, and the differences of the groups were considered significant if pvalues were smaller than 0.05.
3. RESULTS
This study used ANOVA and Chi-square as a statistical analysis for the three different groups, and the results for MCST results were classified into five groups for analysis—number of categories completed (Cat), preservative error score (PE), non-preservative error score (NPE), unique error (UE) and total error (TE). For Cat, UE and TE showed a significant difference for all three groups whereas PE and NPE did not demonstrate a significant difference (Table 1). Also, in all three groups, there were no statistical differences for age (normal control group = 77.24 ± 5.59, Alzheimer’s disease = 78.09 ± 6.124, vascular dementia group = 77.6 ± 5.144, F value = 0.388, p-value = 0.679), education level (normal control group = 7.73 ± 4.60, Alzheimer’s disease = 5.44 ± 4.81, vascular dementia group = 6.45 ± 4.87, F value = 4.053, pvalue = 0.019), smoking, drinking and depression (Table 2).
4. DISCUSSION
The WCST is particularly sensitive to frontal-lobe lesions [27] and is a well-validated neuropsychological tool for the assessment of executive functioning [28]. The test involves individual presentation of up to 128 cards and requires the examinee to learn simple perceptual rules for classification on the basis of verbal feedback to their responses. The WCST is commonly used for psychiatric analysis, as a decision-making concept formation and recognition test. Despite the benefits of the WCST, it requires 30 to 60 minutes to administer and is particularly difficult for patients with dementia who invariably find it to be a demoralizing experience and may reject the test outright. It is much harder for the elderly to finish the WCST; hence, the results are unusable. This has resulted in the increased use of the MCST, which decreases the difficulty for elderly patients finishing the test. A preferable option is to modify the WCST so that the important test characteristics are not sacrificed and the test is less frustrating to the patient.
The relatively poorer performance in category completion may be related to excessive preservative errors and/or non-preservative errors. Since most errors made were non-preservative, the unsuccessful completion of 6 categories was probably due to an inability to understand the nature and concepts of the task, or to remember previous responses [29]. Since the present study evaluated older people, with a mean age over 77.6 years, the fewer categories obtained may be explained by the declination of executive function in older adults. Further study in the comparison of MCST performance in different age groups should be conducted to address this hypothesis.
This study was designed to control for age and education level in the three groups, so no prominent difference in preservative errors and/or non-preservative errors were noted in these groups, although there were high proportions rate of preservative errors and/or non-preservative errors in these three groups. This study showed a significant difference between the control group, and AD and vascular dementia patients in Cat, UE and TE. (This can be explained by the grater declination of executive function in AD and vascular dementia patients than in the normal control group). Hence, a modified MCST is a suitable tool for dementia analysis, yet there still is a need to develop a standard data for special elderly dementia
Table 1. MCST results of the three groups.

*p < 0.05.
Table 2. Demographic results of the three groups.
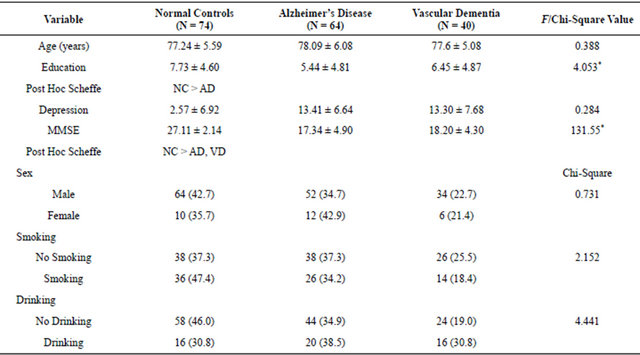
*p < 0.05.
cases. Therefore, to effectively use the MCST as a clinical assessment of neurological or psychiatric problems in elderly people, ageand education-based normative data should be developed.
5. CONCLUSION
The Nelson’s Modified Card Sorting Test is an important neuropsychological test. The test is mainly reliant on frontal lobe function and provides a measure of executive function. Our results suggest that cognitive function appears to significantly impair MCST performances in AD and VD patients, so these should be taken into consideration during an interpretation of the clinical assessment, and our finding suggest that some executive function tests are more sensitive than others for predicting specific functional abilities and that they may be most useful to healthcare professionals for treatment planning. For the effective use of the MCST in a clinical setting, further studies of specific clinical populations are planed to develop normative data for elderly Taiwanese people.